Translate this page into:
A call to action; national survey of teaching radiology curriculum to medical students

*Corresponding author: Scott Andrew Rohren, School of Medicine, Baylor College of Medicine, Houston, Texas, United States. scottrohren@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rohren SA, Kamel S, Khan ZA, Patel P, Ghannam S, Gopal A, et al. A call to action; national survey of teaching radiology curriculum to medical students. J Clin Imaging Sci 2022;12:57.
Abstract
Objectives:
Radiology and medical imaging are important yet often an underrepresented facet of medical education. Notably, there is concern among radiologists that students do not receive enough radiology exposure and that they struggle to interpret image findings on entering residency. Therefore, this survey aims to identify how medical students perceive the radiology curriculum and to determine gaps in delivery.
Material and Methods:
Students were recruited from United States (US) medical schools and given a 21-question survey assessing their perception of the radiology curriculum as well as asking about their confidence levels regarding medical imaging. The inclusion criteria were age >18 and enrolled in US medical school. The surveys were completed in April–July 2020 by students across the US. Objective parameters were measured as percentage correct, while subjective parameters used a 4-point Likert scale.
Results:
A total of 472 medical students across 31 medical schools completed the surveys with a response rate of 69%. Responses represented all class years within medical schools and showed equal distribution among the future career plans. Students responded that didactic lectures were the most common teaching method and that radiologists were their primary teachers during preclinical education. Students were unfamiliar with the American College of Radiology appropriateness criteria with 65% responding they had never heard of it and 33% reporting that they have heard of it but never used it. In assessing students’ perceptions of radiology education, 72% of students responded that they received too little, and 28% of students responded, “Just right.” <1% of students responded that there was “Too much” radiology in their curriculum.
Conclusion:
Radiologists are increasing their educational representation in medical school curricula. Despite this, radiology continues to be under-represented with students desiring more exposure to medical imaging. Integrating the student’s perceptions with existing curricula suggests that efforts should focus on increasing awareness of which studies are appropriate and teaching students how to systematically interpret an image.
Keywords
Education
Curriculum
Teaching
Perspective
Appropriateness
INTRODUCTION
The medical school education system in the United States (US) traditionally has been split into two parts: Preclinical years and clinical years.[1] During the preclinical years, students are expected to gather a basis for the foundational sciences while gaining a conceptual view of disease processes.[2] During clinical years, students rotate through specialties to further improve their skills and prepare to select the specialty they want to pursue.[3]
Within many medical schools, courses are taught on a systems-basis during preclinical education, and by core clerkships during the clinical years. Imaging education is incorporated into different disciplines, and a radiology clerkship is not required by many medical schools. Thus, a high variation in how medical students receive radiology education is present.[4]
Over the years, several methods of teaching medical imaging and the concepts of radiology have been implemented. These strategies have included various efforts such as incorporating imaging into anatomy lectures, requiring a radiology clerkship, as well as teaching imaging during non-radiology clinical clerkships.[5-7] These methods have been implemented to varying degrees of success.[8] One pertinent challenge is the lack of consensus as to the best methodology to teach radiology. Subsequently, there has been no uniform method to teach medical imaging with concepts being taught frequently by non-radiologists. Moreover, there is a disparity in which concepts are given emphasis. As a result, there is concern that students are not being properly exposed to radiology and that its education does not align with the rest of the curriculum.[9]
Interpretation of medical imaging is paramount to clinical practice, even for non-radiologists.[10] Through radiology exposure and radiology education, students are better prepared for entering their postgraduate training and can derive more meaningful clinical information when diagnosing patients. Particularly, there is a need for students to be able to recognize emergent radiographic findings.[11] On top of image interpretation, students need to understand the steps necessary to order the correct imaging study for the diagnostic question, they are hoping to answer as the future clinicians. The American College of Radiology (ACR) has created the ACR Appropriateness Criteria in which they have compiled evidence, outcomes, and clinical perspectives to create lists of the most appropriate imaging studies for a given clinical presentation.[12] Implementation of these criteria has not been without issues. Adoption of the ACR appropriateness criteria has been slow in clinical practice.[13] Moreover, students are seldom educated about proper usage given its low usage in clinical medicine.
The ACR has developed educational goals to standardize the way radiology is taught and ensure that students are able to adequately be exposed to the field. Some of the key recommendations are having imaging taught by radiologists, having students interact with radiologists during their clinical rounds, and teaching students about the ACR appropriateness criteria to help them order the proper studies.
With the wide variation in how medical students are taught radiology, it is important to understand students’ perspectives on how they are taught medical imaging. In this study, the authors assess US medical students’ opinions on their radiology curricula and their impact on their education.
MATERIAL AND METHODS
This is a multicenter and institutional review board-approved survey where we assessed medical students across five broad categories: (1) Demographic information; (2) preclinical radiology teaching methods; (3) clinical radiology teaching methods; (4) ACR appropriateness criteria exposure; and (5) confidence in image evaluation. We designed the online questionnaire using SurveyMonkey (SurveyMonkey Inc., San Mateo, CA, USA). Survey questions were derived from similar questionnaires in the literature.[14,15] The questions were reviewed by radiologists and educational specialists for clarity and to remove bias.
Distribution of the survey was achieved by recruiting student ambassadors through radiology interest group emails. The ambassadors were then asked to forward the invitation to their classmates and have them complete the questionnaire. We obtained informed consent electronically at the start of the online survey. The current enrollment in a US medical school was the only requirement to complete the survey. Descriptive statistical analyses were conducted through SurveyMonkey (SurveyMonkey Inc., San Mateo, CA, USA). Likert scale responses were weighted by assigning a numeric value (1=Not Important, 2=Somewhat Important, 3=Moderately Important, and 4=Very Important). The mean and standard deviation were calculated for these responses.
RESULTS
Between April 2020 and July 2020, the survey was sent to 686 students with a total of 472 responses from 31 medical schools in the US for a response rate of 68.8%. Two hundred and seventeen (46%) of respondents were male, 246 (52%) were female with 9 (2%) preferring not to answer. Responses represented students from all regions (North-east, Southeast, Midwest, South-west, West coast), all class years within medical schools, and showed equal distribution among the future career plans [Table 1]. When asked about the amount of radiology experience in medical school, 72% of students responded that they received “Too Little” and 28% of students responded, “Just right.” <1% of students responded that there was “Too much” radiology in their curriculum.
| Frequency (n) | Percentage | |
|---|---|---|
| Gender | ||
| Male | 217 | 46.0 |
| Female | 246 | 52.1 |
| Prefer Not to Answer | 9 | 1.9 |
| Class Year | ||
| 1st-year student | 179 | 37.9 |
| 2nd-year student | 118 | 25.0 |
| 3rd-year student | 128 | 27.1 |
| 4th-year student | 47 | 10.0 |
| Future Career Plans | ||
| Clinician in Medical Field | 213 | 45.1 |
| Clinician in Surgical Field | 99 | 21.0 |
| Radiology | 71 | 15.0 |
| Undecided | 89 | 18.9 |
Radiology teaching in preclinical years
Nearly all students responded that their preclinical examinations included radiology imaging (96%). Furthermore, the majority of students (67%) responded that imaging was primarily taught by radiologists. The most encountered teaching methods for radiology were didactic lectures (86%), and self-guided learning (61%). Less than half (38%) responded that their schools provided students with resources to go through medical imaging on their own outside of the classroom. Students were taught a varying degree of modalities. X-ray, ultrasound, computed tomography, and magnetic resonance imaging were taught the most frequently with less representation for positron emission tomography and fluoroscopy [Figure 1]. Only 21.4% of respondents reported that they received formal training in radiation safety. Despite this, 43.4% of students correctly answered a question asking how much background radiation an X-ray exposes a patient to.
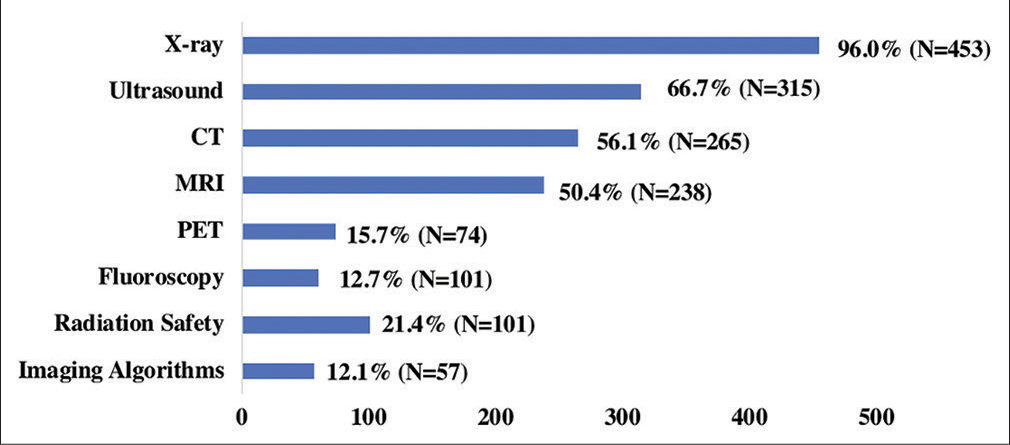
- Student’s exposure to imaging modalities.
Radiology teaching during clinical years
For students who have had clinical experience, 22% of students encountered medical imaging on rounds while discussing with a radiologist, 91% on rounds while discussing with a non-radiologist doctor, 84% discussing with a resident, and 9% of students reporting they did not encounter medical images. During clinical rounds, 2% of students responded that they interacted with radiologists daily, 3% of students interacted a few times a week, 22% responded they interacted a few times a month, 45% interacted once or twice during the year, and 27% responded that they never interacted with radiologists.
ACR appropriateness exposure
When students were asked about whether they were familiar with the ACR appropriateness criteria, 65% of all respondents had never heard of it, 18% had heard of it but are not familiar, 13% were somewhat familiar, and 4% were very familiar. For third and 4th year students, 48% had never heard of it, 23% had heard of it but are not familiar, 25% were somewhat familiar, and 4% were very familiar. Students who indicated that they have entered clinical training were asked how often they used the ACR Appropriateness Criteria. The majority (81%) had never used it, 14% have used it a few times in a year, 2% have used it a few times in a month, and 2% used it a few times each week.
Image interpretation importance and confidence
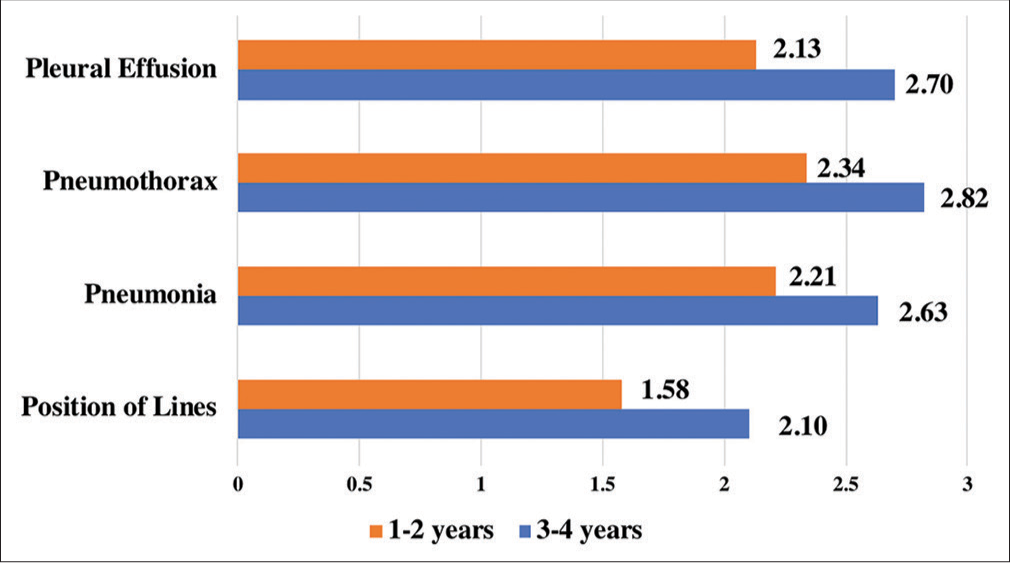
Students were asked to rate how important they thought it was for interns to interpret varying imaging studies. Most students responded that chest radiographs were important to interpret (98%) while only 92% of students felt computer tomography scans of the head were important [Table 2]. Students reported varying confidence levels in reading several common radiological findings, such as pneumothorax and pleural effusion, on a radiograph. First- and 2nd-year students responded mostly that they did not have confidence in interpretation. Conversely, 3rd-and 4th-year students demonstrated greater confidence in interpretation but still noted that many did not yet develop confidence [Figure 2].
| Not very important (%) | Important (%) | 4-point Likert | |
|---|---|---|---|
| Bone radiographic | 7.1 | 92.9 | 3.6 |
| Chest radiographic | 3.0 | 97.0 | 3.81 |
| Head CT | 7.7 | 92.3 | 3.64 |
| Abdomincal radiographics | 5.2 | 94.8 | 3.65 |
- Student’s responses to image interpretation on a 4-point Likert scale.
DISCUSSION
The primary goal of this study was to identify how radiology is being taught, and the perspectives of students toward the curriculum. The previous studies have found a need for radiologists to be further involved in teaching radiology and imaging to medical students.[3,4,8] Our results show that radiologists have developed a greater role within the preclinical curriculum with 67% of students reporting that radiologists taught their imaging and nearly all students responding that they were tested on diagnostic imaging.
When previously surveyed, students and clinicians alike wished that radiology education focused on distinguishing normal from abnormal and developing methods to systematically review a scan.[3,16,17] Moreover, residents noted that they wished they had more confidence in their interpretations.[18] The results demonstrate that students are getting exposed to images and that as time progresses their confidence grows. However, only about half of 3rd- and 4th-year students responded that they were “moderately confident” or “very confident” in their image interpretation, suggesting a further increased need to expose students to diagnostic imaging.
The previous literature has identified a gap in student’s knowledge of the ACR appropriateness criteria.[11] Our results corroborated this with 65% of students not knowing about it and an additional 18% who knew but were unfamiliar. Proper imaging studies are of increasing concern as health care aims to reduce expenditures.[19] Knowledge of ACR appropriateness criteria can help guide clinicians and trainees alike about proper imaging modalities.
Our data also highlighted the importance of radiologist interaction with students during their clinical years. While improvements have been made in the preclinical curriculum with radiologists teaching images and being incorporated into exams, there is progress to go with the majority of students having no interactions with radiologists on rounds and not being familiar with the ACR appropriateness criteria.
Including radiology in school’s medical curriculum poses a unique challenge. Imaging compliments many aspects of practice and is often implemented as a supplement to the main teaching concepts. As many medical schools currently teach by organ systems, this allows different specialties to give students the breadth of their practice while radiology does not have this advantage. Previously, students have said that they wish radiology was better represented within their curricula.[20-22] Our findings corroborated this with students wishing for more radiology education. This poses a challenge for radiologists as a main issue facing education is a lack of time allotted to imaging.[23] Of note, radiology educators need to consider how radiology is being taught in both preclinical as well as clinical years. Preclinical students learn image interpretation in more formal settings, often beginning with normal anatomy. Conversely, clinical clerkship students interact with images informally during patient care and as such are exposed to more pathologic findings. This, in part, may explain the increased confidence, students have in their image interpretation skills once they have clinical experience.
As it stands, radiology education is still primarily taught with traditional didactic lectures before students move to the clinical stages of their training and view patient’s images. While didactic lectures have been historically used, innovative teaching methods should be emphasized to the radiology educator.[24] Engaging students using active learning styles such as flipped classrooms, interactive case discussions, and application exercises may improve students’ skills and confidence in image interpretation, regardless of their future career paths.
There are a few limitations to our study. The student ambassadors used to distribute surveys were recruited from radiology interest groups. As a result, the students sampled may view radiology more favorably, and there was over-representation of students who were interested in radiology as a career. Despite this, most respondents were not interested in radiology and had interest in diverse career paths. Another limitation is that this study surveyed only US allopathic (MD) schools and not osteopathic (DO) schools, which limits the generalizability of these results to all students in the US.
CONCLUSION
Image interpretation is an important yet often under-taught subject within medical school curricula. From students’ perspectives, it is clear that radiologists are continuing to increase their educational representation, yet many shortcomings still exist. Particularly, radiologists need to further help students develop methods to interpret studies and locate abnormalities. The future studies should focus on how innovative educational strategies can be implemented into existing curricula to target these weak points to improve student understanding as well as assessing clinician knowledge of the ACR appropriateness criteria.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A primer on medical education in the United States through the lens of a current resident physician. Ann Transl Med. 2015;3:270.
- [Google Scholar]
- Flexner revisited: The role and value of the basic sciences in medical education. Acad Med. 2010;85:349-55.
- [CrossRef] [PubMed] [Google Scholar]
- Radiology undergraduate and resident curricula: A narrative review of the literature. J Chiropr Humanit. 2015;22:1-8.
- [CrossRef] [Google Scholar]
- Radiology education in medical school and residency. Acad Radiol. 2018;25:1333-43.
- [CrossRef] [PubMed] [Google Scholar]
- The role of radiology in preclinical anatomy: A critical review of the past, present, and future. Acad Radiol. 2013;20:297-304.
- [CrossRef] [PubMed] [Google Scholar]
- Radiology clerkship requirements in Canada and the United States: Current state and impact on residency application. J Am Coll Radiol. 2020;17:515-22.
- [CrossRef] [PubMed] [Google Scholar]
- Medical student radiology education: Summary and recommendations from a national survey of medical school and radiology department leadership. J Am Coll Radiol. 2014;11:606-10.
- [CrossRef] [PubMed] [Google Scholar]
- Radiology in the undergraduate medical curriculum: Too little, too late? Med Sci Educ. 2015;25:223-7.
- [CrossRef] [PubMed] [Google Scholar]
- The vital role of radiology in the medical school curriculum. AJR Am J Roentgenol. 2003;180:1239-42.
- [CrossRef] [PubMed] [Google Scholar]
- The value of good medical student teaching: Increasing the number of radiology residency applicants. Acad Radiol. 2000;7:960-4.
- [CrossRef] [Google Scholar]
- Radiology medical student education: An outcome-based survey of PGY-1 residents. Acad Radiol. 2013;20:284-9.
- [CrossRef] [PubMed] [Google Scholar]
- The American college of radiology. ACR appropriateness criteria project. Radiology. 2000;214:3-46.
- [CrossRef] [Google Scholar]
- Awareness, utilization, and education of the ACR appropriateness criteria: A review and future directions. J Am Coll Radiol. 2016;13:131-6.
- [CrossRef] [PubMed] [Google Scholar]
- Fourth-year medical student opinions and basic knowledge regarding the field of radiology. Acad Radiol. 2013;20:272-83.
- [CrossRef] [PubMed] [Google Scholar]
- Undergraduate radiology teaching from the student's perspective. Insights Imaging. 2013;4:103-9.
- [CrossRef] [PubMed] [Google Scholar]
- Radiology curriculum for medical students: Clinicians' perspectives. Australas Radiol. 2006;50:442-6.
- [CrossRef] [PubMed] [Google Scholar]
- Radiology curriculum topics for medical students. Acad Radiol. 2006;13:880-4.
- [CrossRef] [PubMed] [Google Scholar]
- Developing a national medical student curriculum in radiology. J Am Coll Radiol. 2005;2:8-11.
- [CrossRef] [PubMed] [Google Scholar]
- Preclinical medical student training in radiology: The effect of early exposure. AJR Am J Roentgenol. 2007;188:W9-14.
- [CrossRef] [PubMed] [Google Scholar]
- Introducing first-year medical students to radiology: Implementation and impact. Acad Radiol. 2018;25:780-8.
- [CrossRef] [PubMed] [Google Scholar]
- Medical student perceptions of radiology use in anatomy teaching. Anat Sci Educ. 2015;8:510-7.
- [CrossRef] [PubMed] [Google Scholar]
- The state of radiologic teaching practice in preclinical medical education: Survey of American medical, osteopathic, and podiatric schools. J Am Coll Radiol. 2015;12:403-8.
- [CrossRef] [PubMed] [Google Scholar]
- A review of innovative teaching methods. Acad Radiol. 2019;26:101-13.
- [CrossRef] [PubMed] [Google Scholar]







