Translate this page into:
Comparing MRI and arthroscopic appearances of common knee pathologies: A pictorial review

*Corresponding author: Nikhil N. Patel, Department of Orthopaedic Surgery, Division of Sports Medicine, University of Miami Miller School of Medicine, Miami, Florida, United States. nnp20@med.miami.edu
-
Received: ,
Accepted: ,
How to cite this article: Lamour RJ, Patel NN, Harris GB, England JS, Lesniak BP, Kaplan LD, Jose J. Comparing MRI and arthroscopic appearances of common knee pathologies: A pictorial review. J Clin Imaging Sci. 2024;14:15. doi: 10.25259/JCIS_98_2023
Abstract
Knee pathology, including anterior cruciate ligament (ACL) tears, meniscal tears, articular cartilage lesions, and intra-articular masses or cysts are common clinical entities treated by orthopedic surgeons with arthroscopic surgery. Preoperatively, magnetic resonance imaging (MRI) is now standard in confirming knee pathology, particularly detecting pathology less evident with history and physical examination alone. The radiologist’s MRI interpretation becomes essential in evaluating intra-articular knee structures. Typically, the radiologist that interprets the MRI does not have the opportunity to view the same pathology arthroscopically. Thus, the purpose of this article is to illustratively reconcile what the orthopedic surgeon sees arthroscopically with what the radiologist sees on magnetic resonance imaging when viewing the same pathology. Correlating virtual and actual images can help better understand pathology, resulting in more accurate MRI interpretations. In this article, we present and review a series of MR and correlating arthroscopic images of ACL tears, meniscal tears, chondral lesions, and intra-articular masses and cysts. Short teaching points are included to highlight the importance of radiological signs and pathological MRI appearance with significant clinical and arthroscopic findings.
Keywords
Arthroscopy
Knee pathology
Orthopedic surgeons
Radiologists
Magnetic resonance imaging
INTRODUCTION
In this article, we present MRI alongside the respective arthroscopic knee images to better correlate radiological findings with arthroscopic knee findings. Arthroscopy is a widely used, non-invasive method used to directly visualize and repair pathologies within the joint capsule. Knee arthroscopy specifically involves the creation of several percutaneous incisions at various locations surrounding the joint to allow for the insertion of the arthroscope and arthroscopic instrumentation. The arthroscope enables real-time visualization of the internal structures of the knee on a monitor, guiding the surgeon in addressing identified issues through tissue repair or resection. Noteworthy, attributes of knee arthroscopy include its minimally invasive nature, abbreviated post-operative recovery period relative to conventional open surgery approaches, and reduced susceptibility to complications such as infection or hemorrhage.[1,2] The following series of cases will cover arthroscopic and MR images of various knee pathologies and complications to bring significant findings to the radiologist.
Anterior cruciate ligament (ACL) pathology
The ACL tear is the most common ligament injury in the body that is treated operatively. However, the true incidence of ACL injuries is difficult to assess because some injuries still need to be diagnosed.[3,4] The incidence of ACL reconstructions has been studied and shown to be significantly increasing.[5] Estimated rates of reconstructions in the United States range from 60,000 to 175,000,123) An epidemiological study of ACL reconstructions identified an increase from 6178 in 1997 to 7507 in 2006 in New York State alone.[5] This increasing volume of ACL reconstructions has made magnetic resonance imaging (MRI) an invaluable tool for accurately diagnosing various degrees of ACL injury for pre-operative evaluation.
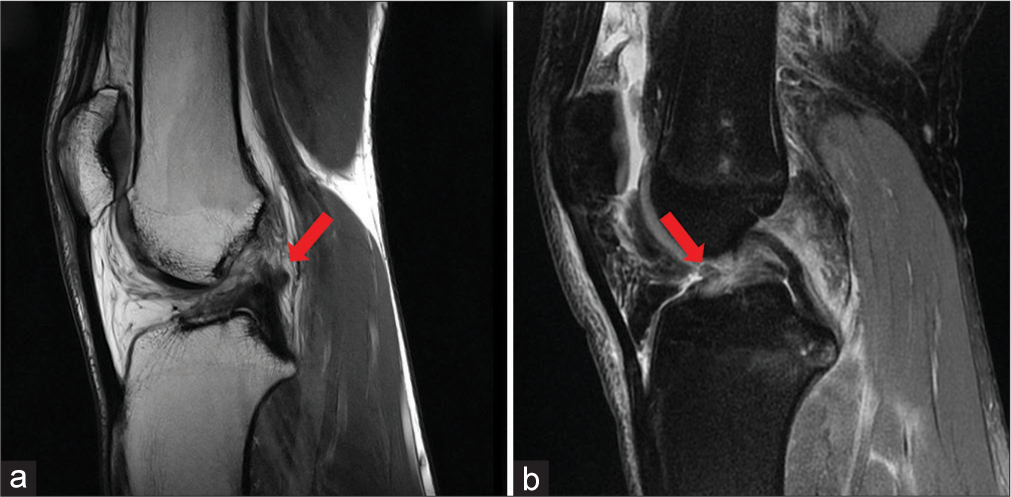
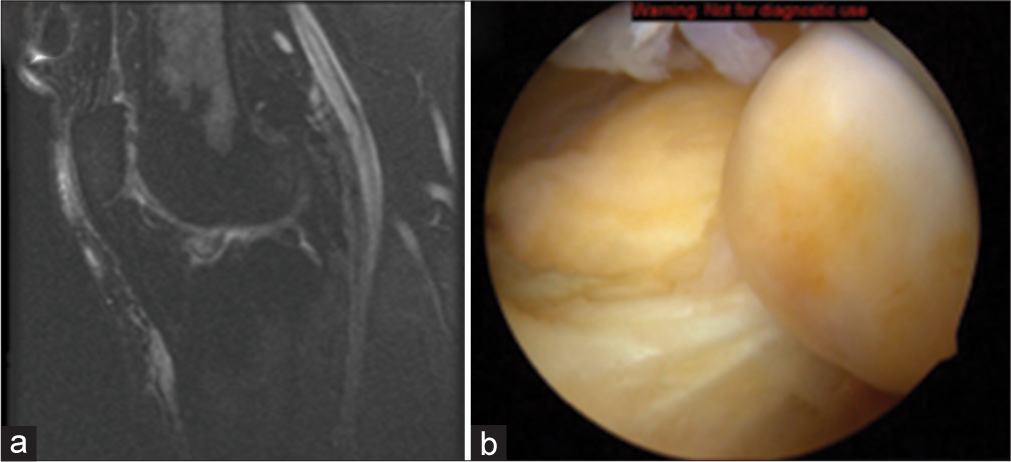
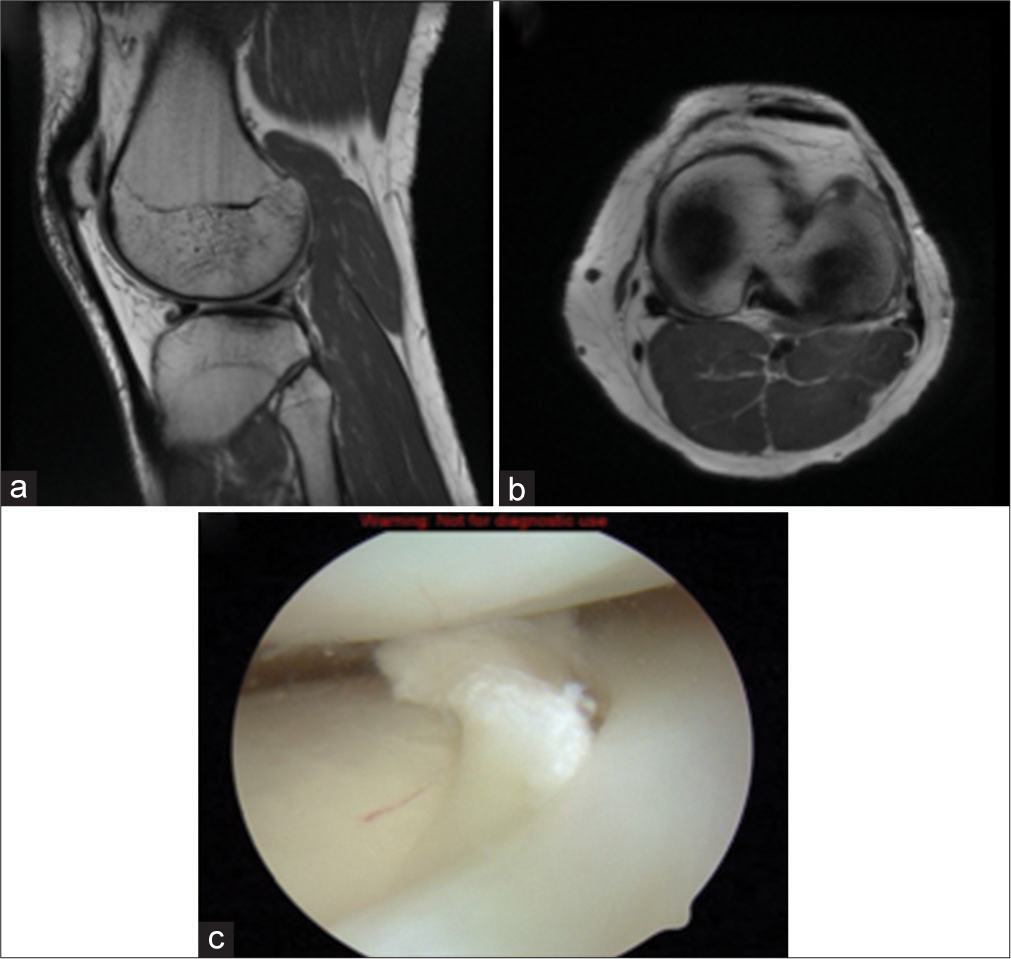
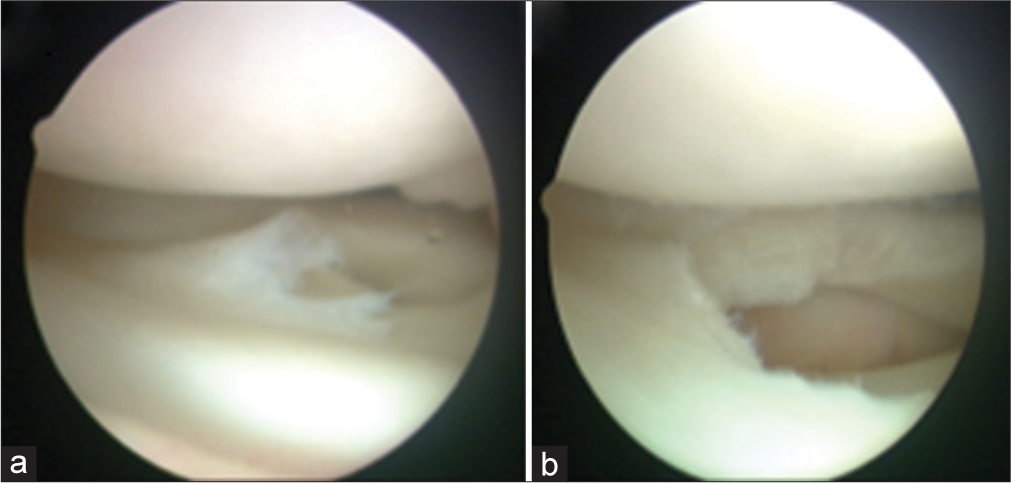
Case 1: Partial ACL rupture
Teaching point: Descriptions of partial ACL tears vary from bleeding at the femoral origin to complete rupture of the anteromedial (AM) or posterolateral (PL) bundle.[6] This variability in the degree of ligament disruption makes the definitive diagnosis of partial ACL tear very difficult, even with MRI.[6-9] The variable MRI appearance of partial ACL rupture results in low sensitivity and specificity in diagnosis, with reported 55% of sensitivity and 75% of specificity when using primary MRI signs of partial ACL tear.[10] Therefore, arthroscopy is used in combination with history, physical examination, and MRI to unequivocally diagnose, in the setting of a partial ACL tear, a functionally ACL deficient knee, and develop an appropriate treatment plan [Figure 1].[4,6,9]
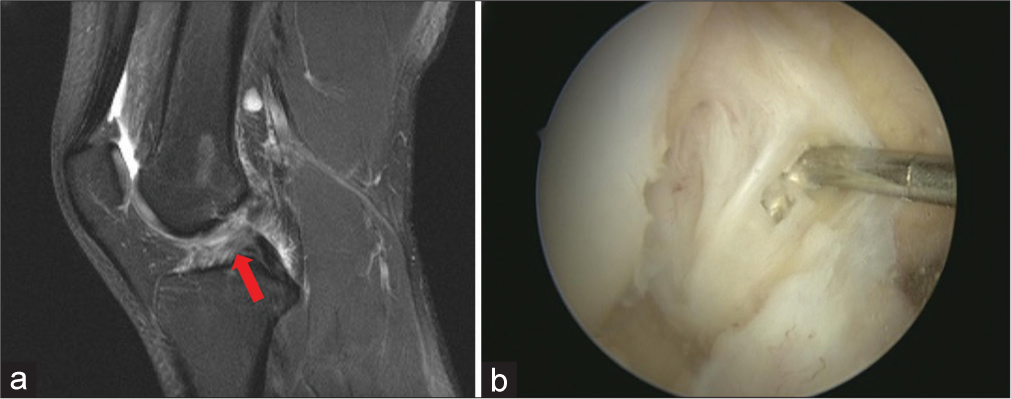
- A 25-year-old male athlete presents with localized knee pain, swelling, and instability. The injury was sustained during a non-contact pivoting event on the soccer field. (a) A sagittal fat-suppressed proton density magnetic resonance image of a right knee demonstrates thinning and increased signal intensity of the ACL. Note that the orientation and overall continuity are maintained (red arrow). (b) Arthroscopic image, right knee. The probe demonstrates substantial interstitial damage of the ACL and laxity of the remaining fibers. Before ultimate failure, the ligament may elongate by more than 50% compared with its resting length, potentially rendering the damaged ACL non-functional. (ACL: Anterior cruciate ligament.)
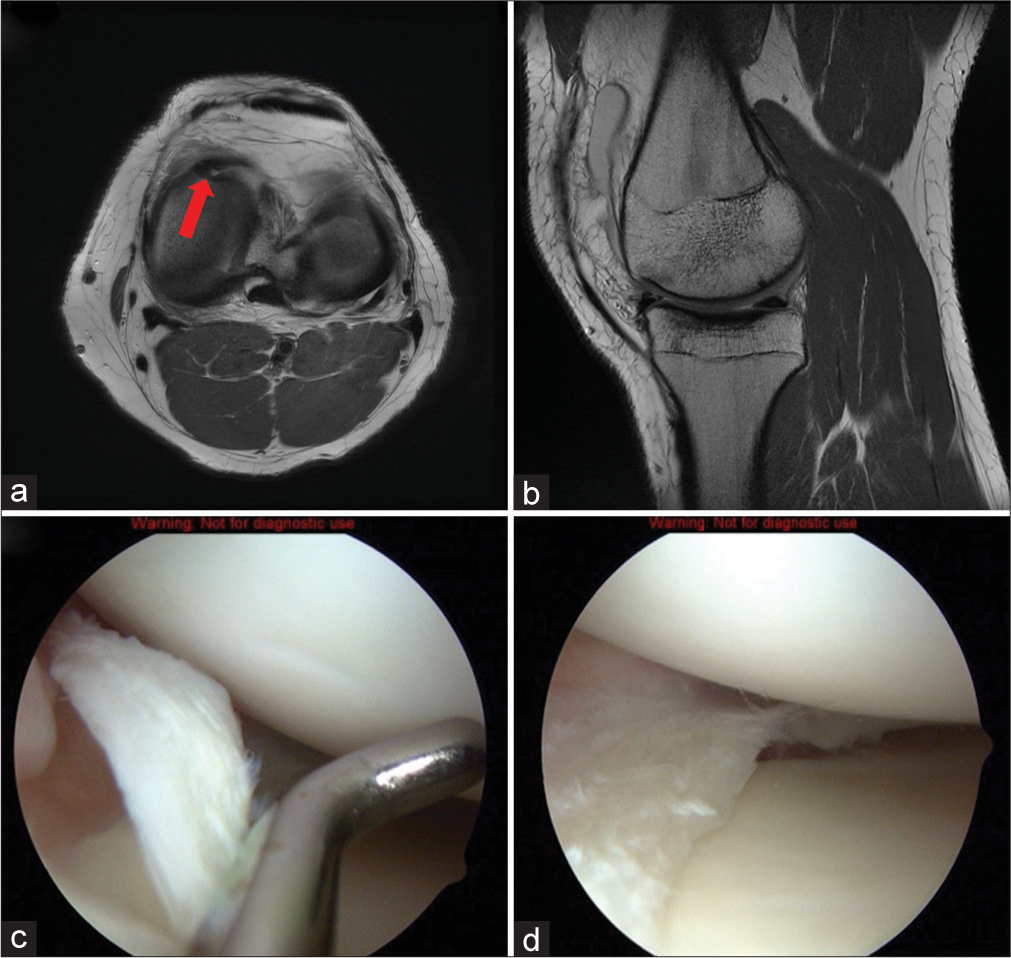
Case 2: ACL high-grade partial rupture of quadrupled hamstrings autograft
Teaching point: Clinically, a high-grade partial rupture of the autograft can be difficult to diagnose without significant instability.[7] With well-positioned grafts, the same principles apply when evaluating ACL integrity for non-operative versus operative decision-making [Figures 2 and 3].[9,10]
- A 30-year-old female, years after prior ACL surgery presenting with acute knee pain, effusion, and mechanical instability after participating in a recreational basketball game. (a) A sagittal T1-weighted image demonstrating the torn anterior portion of autograft displaced anteriorly, which can become symptomatic with the knee in extension. (b) A sagittal T1-weighted magnetic resonance image of the torn anterior hamstrings autograft with the contused posterior portion in continuity and normal orientation (red arrow). (ACL: Anterior cruciate ligament.)
- (a) Arthroscopic image of the extended right knee. The distal stump of the ruptured graft can displace anteriorly, causing a mechanical block to extension. (b) Arthroscopic image of flexed right knee. The ruptured autograft stump is shown debrided with residual hematoma of intact graft posteriorly (red arrow). The thin epiligamentous synovial tissue surrounding the graft suggests a later stage of ligament maturation or “ligamentization.” (c) Arthroscopic image of a right knee. The bare intercondylar wall of the lateral femoral condyle is not typically visualized arthroscopically unless a tear of the ACL is present. A complete femoral-sided tear of the ACL or mid-substance tear with resorption of the proximal end can give the “empty wall” appearance. The ACL is at the bottom right of the image, lying more horizontal than its native position. (ACL: Anterior cruciate ligament.)
Case 3: Complete ACL rupture
Teaching point: The absence of ACL femoral insertion at the intercondylar notch (“empty wall/notch sign”) is an indication of complete rupture [Figure 4].[7]
- A 22-year-old male who presents with marked knee swelling, hemarthrosis, and inability to bear weight sustained during a skiing accident. Lachman’s test was positive, with notable anterior tibial translation (a) a coronal fat-suppressed proton density magnetic resonance image shows the empty wall with an abnormal orientation of the ACL (red arrow). (b) An arthroscopic image of the right knee demonstrates a femoral-sided ACL tear. Note the probe pulling the ruptured ligament forward. The vascular synovial lining of the ACL can be appreciated as well. (ACL: Anterior cruciate ligament.)
Case 4: Complete ACL rupture
Teaching point: The normal orientation of the ACL is typically parallel to the intercondylar roof (Blumensaat’s line) or slightly steeper. A lack of parallelism of ACL fibers and Blumensaat’s line indicates ACL rupture [Figure 5].[7]
- A 27-year-old female presents with sudden knee pain, audible pop, and immediate swelling following a jump during a volleyball game. (a) A sagittal T1-weighted magnetic resonance (MR) image. Note the difference in orientation of Blumensaat’s line and the torn ACL. (red arrow) (b) A sagittal fat-suppressed proton density MR image demonstrates of loss of continuity of ACL fibers and a dense increase in signal intensity at the intercondylar notch representative of hematoma (red arrow).(ACL: Anterior cruciate ligament).
Case 5: Acute ACL rupture
Teaching point: The acutely disrupted ACL commonly presents with associated characteristic injuries.[7] Hemorrhagic effusion, “coup-contrecoup” bone bruising, and “kissing” bone contusions from the pivot shift or hyperextension mechanism are some signs detected radiologically.[7,11,12] It is important for radiologists to make the distinction between acute and chronic tears. ACL reconstruction in the acute setting (1–3 weeks) can lead to arthrofibrosis and permanent loss of knee motion in some patients. The radiologist can further improve MR interpretation of ACL injuries by including findings such as anterior tibial translation, uncovering of the posterior horn of the lateral meniscus, and buckling of the posterior cruciate ligament (PCL). These particular findings are important in diagnosing an unstable ACL tear [Figure 6].[5,13-15]
- 26-year-old male basketball player presents after an abrupt change of direction on the court with a sensation of “giving way” in the knee. He recalls hearing a distinct “pop” and experiencing immediate swelling. Physical examination reveals joint effusion and positive anterior drawer sign. (a) A sagittal fat-suppressed proton density magnetic resonance image demonstrates the characteristic “coup-contrecoup” bone bruising found on the weight-bearing portion of the lateral femoral condyle and the posterior aspect of the lateral tibial plateau from the pivot shift mechanism (red arrows). The impacted depression of the lateral femoral condyle, also known as the “lateral femoral notch sign” or the “deep sulcus sign,” also results from the internal rotation and valgus force of the pivot shift mechanism. (b) An arthroscopic image of the right knee shows an acutely ruptured ACL examined by the probe. Notice the hematoma along the torn ligament. (ACL: Anterior cruciate ligament).
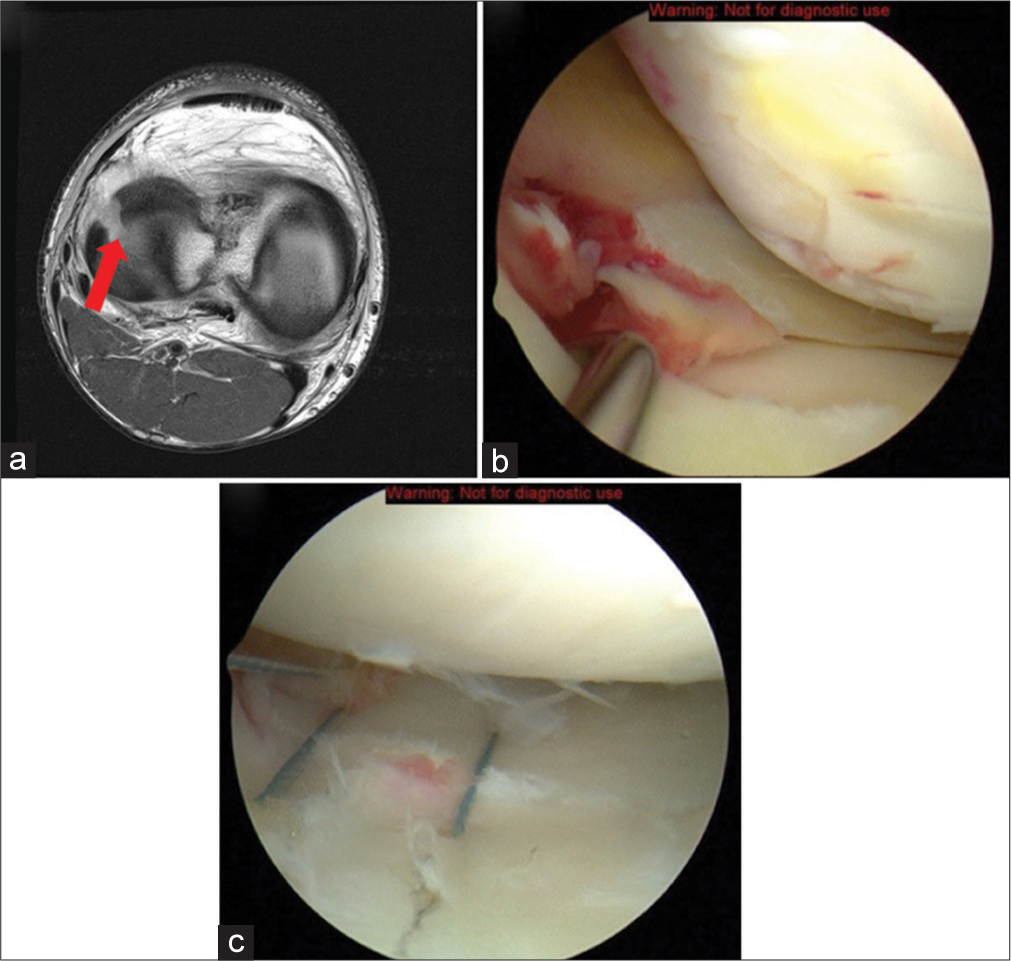
Case 6: ACL ganglion cyst
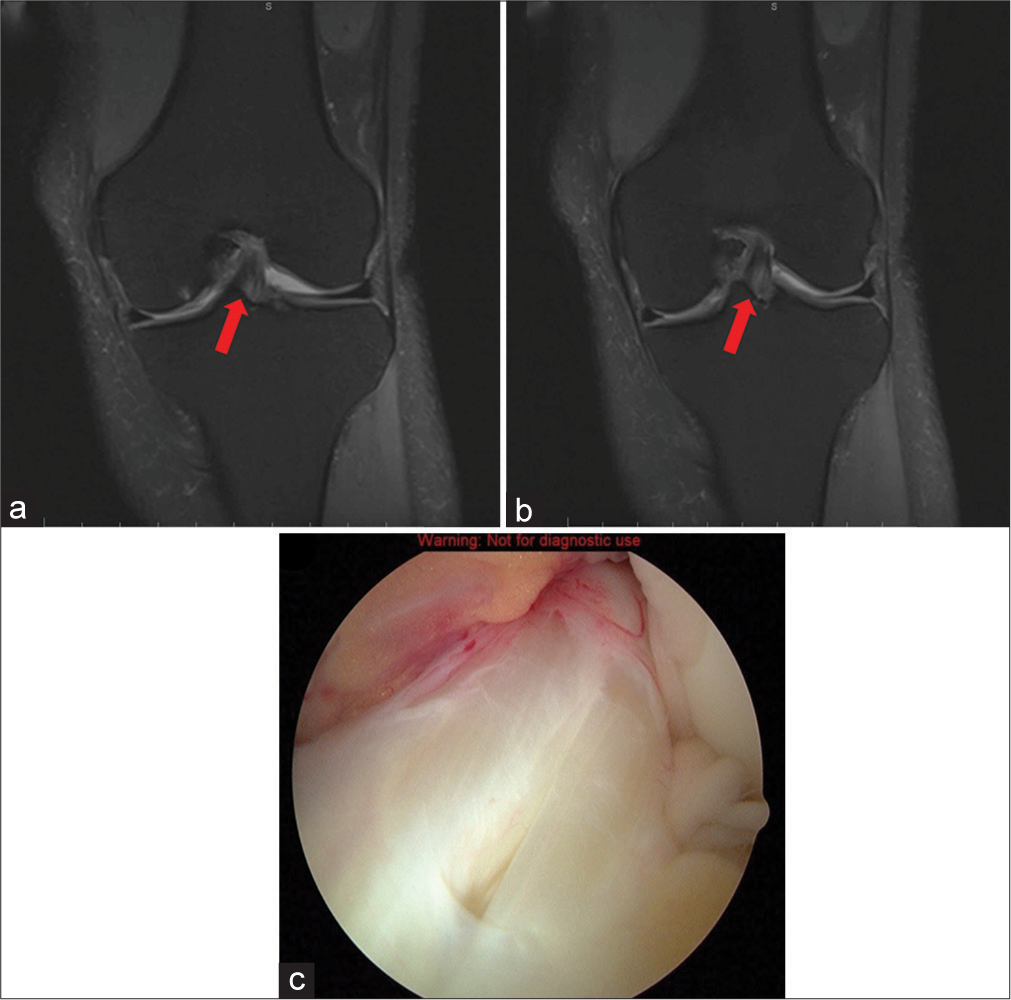
Teaching point: ACL ganglion cysts are rare and currently of unknown etiology.[16-19] It is believed that they may develop from a congenital abnormality, previous injury, mucoid deterioration, or proliferation of pluripotential mesenchymal stem cells.[16-18] The relevance of ACL ganglion cysts is a factor when they become symptomatic, particularly with chronic knee pain, mechanical symptoms, limited range of motion, or instability.[18] When interpreting an MRI of this lesion, a broad differential diagnosis must be formed because a para-ligamentous or intra-ligamentous ganglion cyst can be mistaken for a tear [Figure 7].[7,15-18]
- 34-year-old female avid runner presents with intermittent knee pain and a sensation of fullness in the anterolateral aspect of her knee, especially during flexion. She denies any acute trauma but recalls increasing her training intensity in the past 6 months. On examination, there is mild joint effusion without significant ligamentous instability. (a and b) T1- and T2-weighted sagittal magnetic resonance images of the right knee displaying hypointense and hyperintense, respectively, oval-shaped masses within the ACL, as described in several case reports of ACL ganglion cysts (red arrow). (c) Arthroscopic image of ganglion cystic formation of the ACL with fiber-like projections draped over the ACL. (ACL: Anterior cruciate ligament).
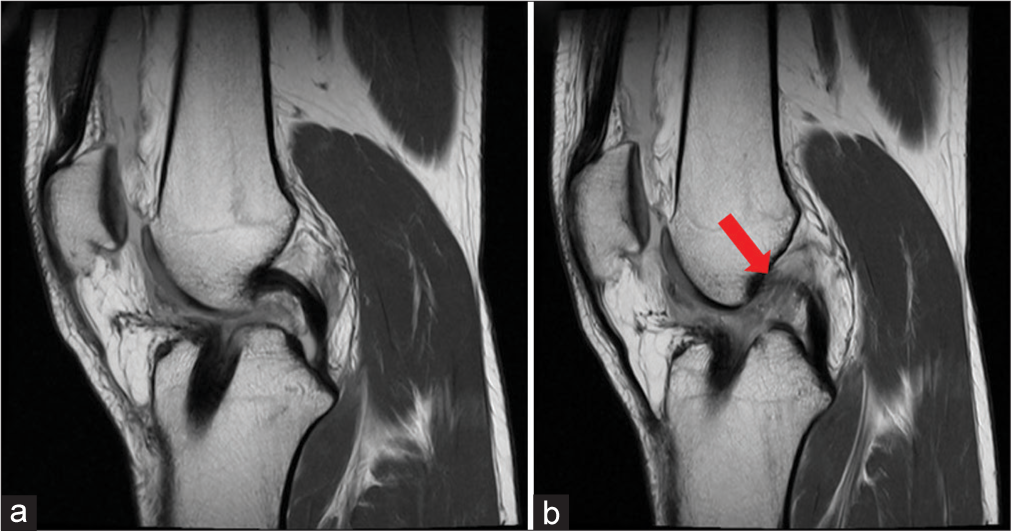
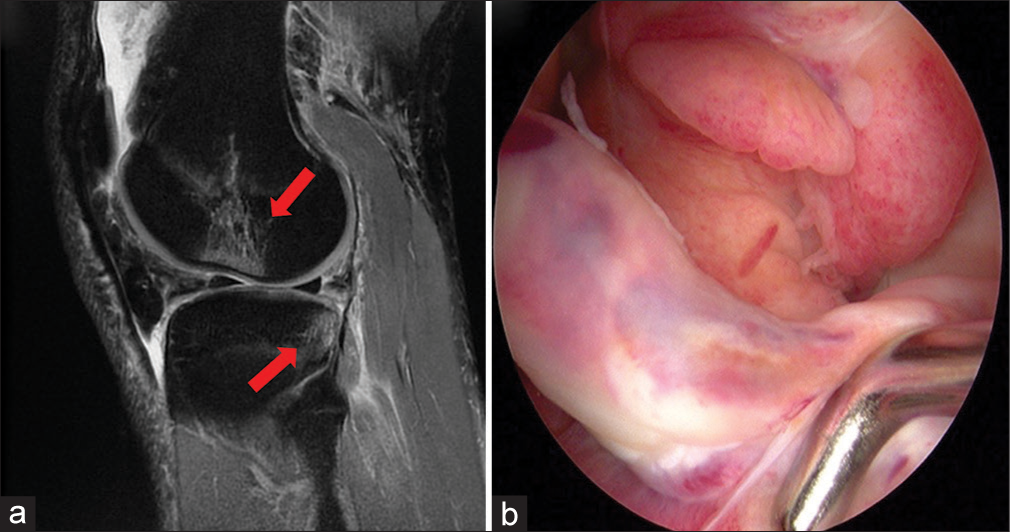
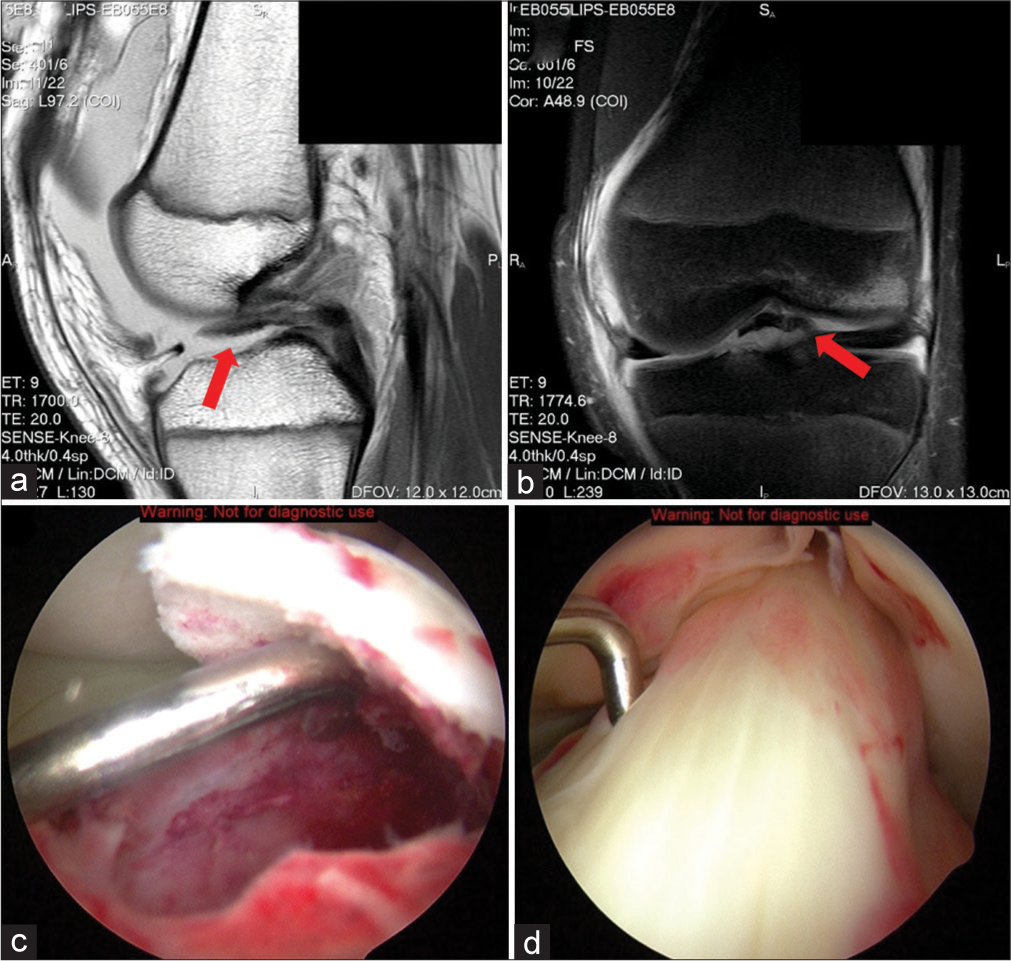
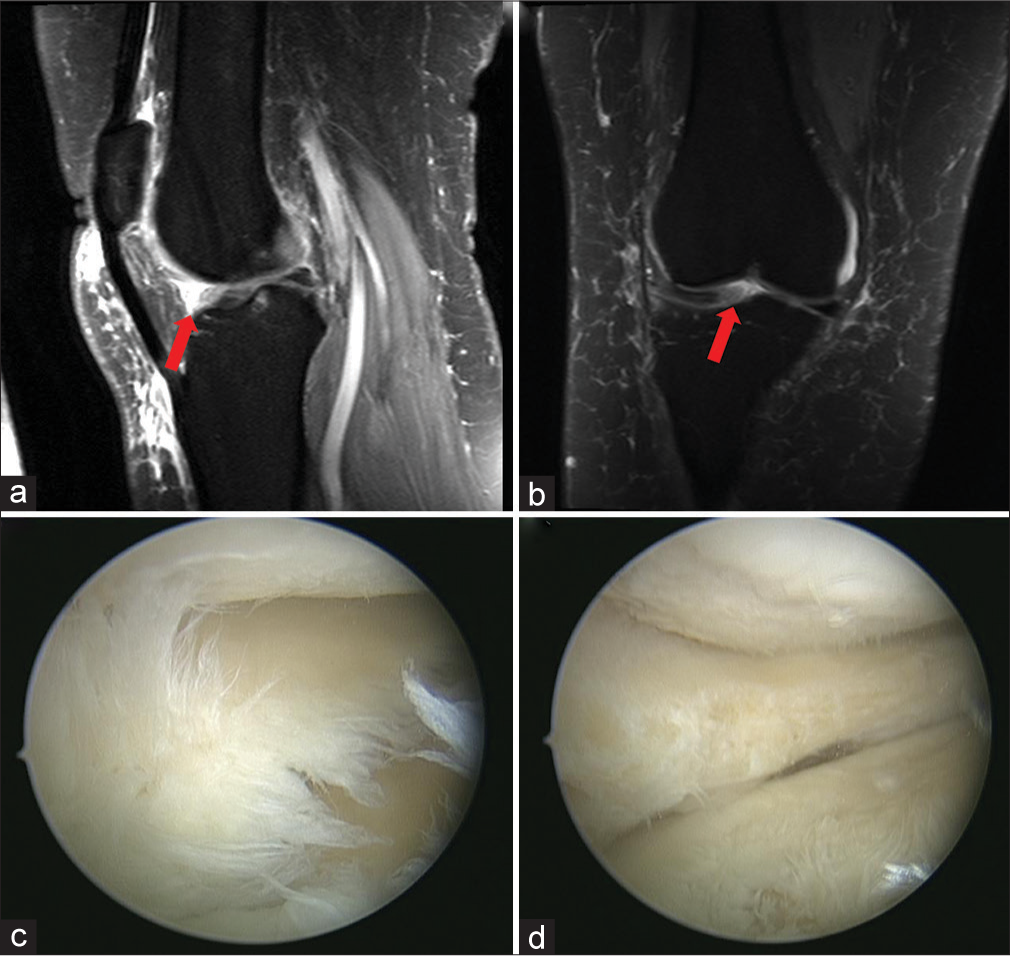
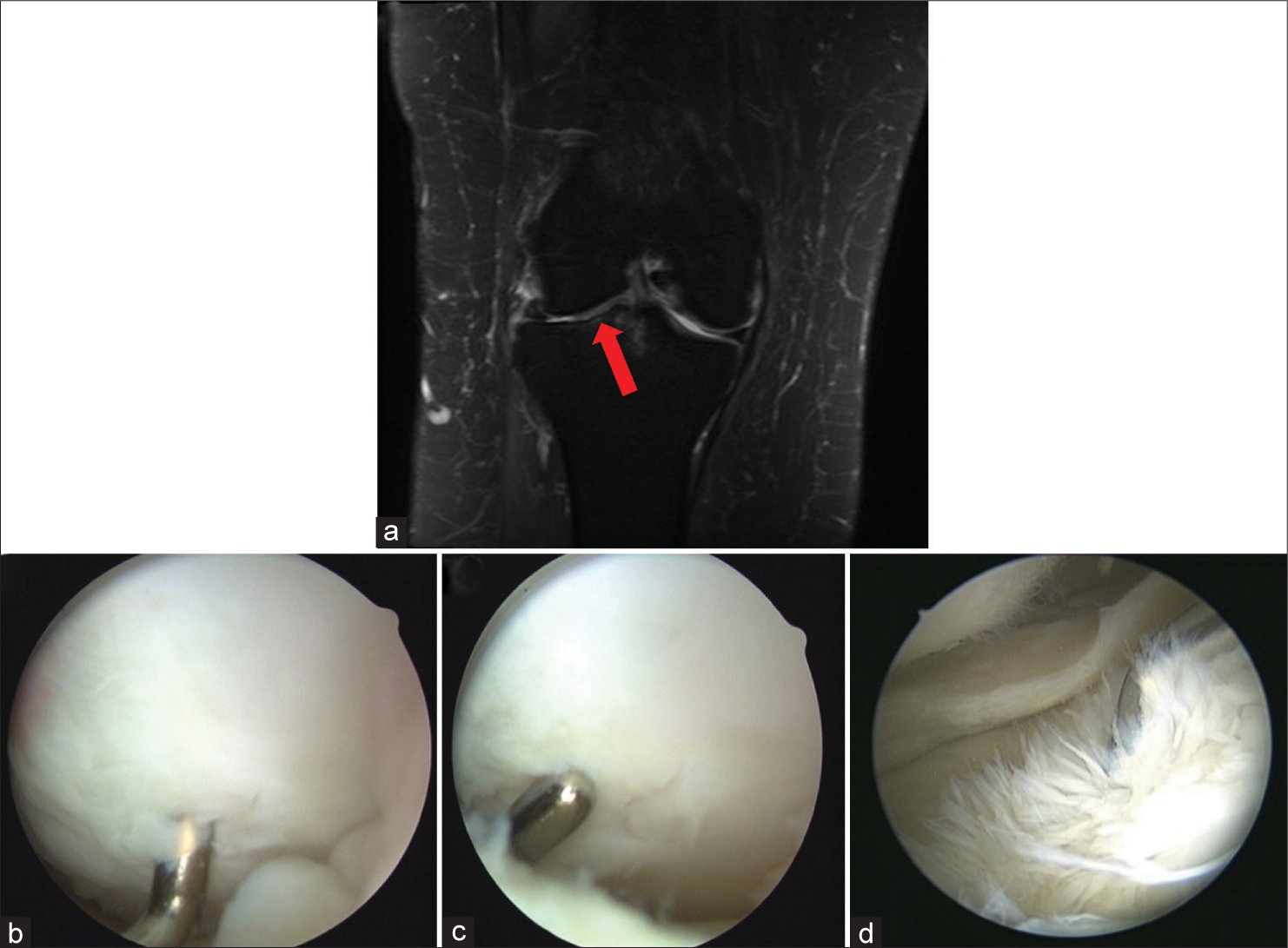
Case 7: Cyclops lesion
Teaching point: The cyclops lesion is a type of localized arthrofibrosis in the form of a fibrous nodule found at the anterior intercondylar notch.[20-23] It typically forms at the tibial insertion of the reconstructed ACL graft resulting in a mechanical block to extension.[7,21] The etiology is unknown, but several theories explaining its formation are described. Repetitive trauma of graft against bone from anterior graft placement resulting in impingement and graft hypertrophy with fibrous proliferation is a reported explanation.[22,23] An undebrided ACL stump and poorly debrided drilling debris of the tibial tunnel could also cause fibrous nodular development.[22,23] Arthroscopically assisted debridement is the accepted treatment of symptomatic patients [Figure 8].[7,20,21,23]
- A 28-year-old male soccer player, 6 months post-operative from an ACL reconstruction using a patellar tendon graft, presents with progressive knee stiffness and a catching sensation during extension. He mentions that his post-operative rehabilitation was initially going well, but he has recently faced difficulty in fully extending the knee. On clinical examination, a restriction in terminal knee extension is noted. (a) T1-weighted sagittal image of the knee shows the intermediate signal intensity nodule of the intercondylar notch anterior to the ACL (red arrow). (b) A proton density-weighted coronal image of the knee demonstrates the same low-intermediate signal intensity nodule and its proximity to the tibial tunnel (red arrow). (c) Arthroscopic image of an extended right knee shows the “cyclops lesion” initially described by Jackson and Schaefer. The probe is firmly pressed into the nodule and demonstrates its fibrous consistency. This nodule was dubbed the “cyclops lesion” due to its head-like appearance and its characteristic focal reddish-blue areas of discoloration due to venous channels, which resemble an eye at arthroscopy. (d) Arthroscopic image of the right knee. The ganglion fiber-like projections are moved to the side to reveal the ACL tibial insertion. (ACL: Anterior cruciate ligament).
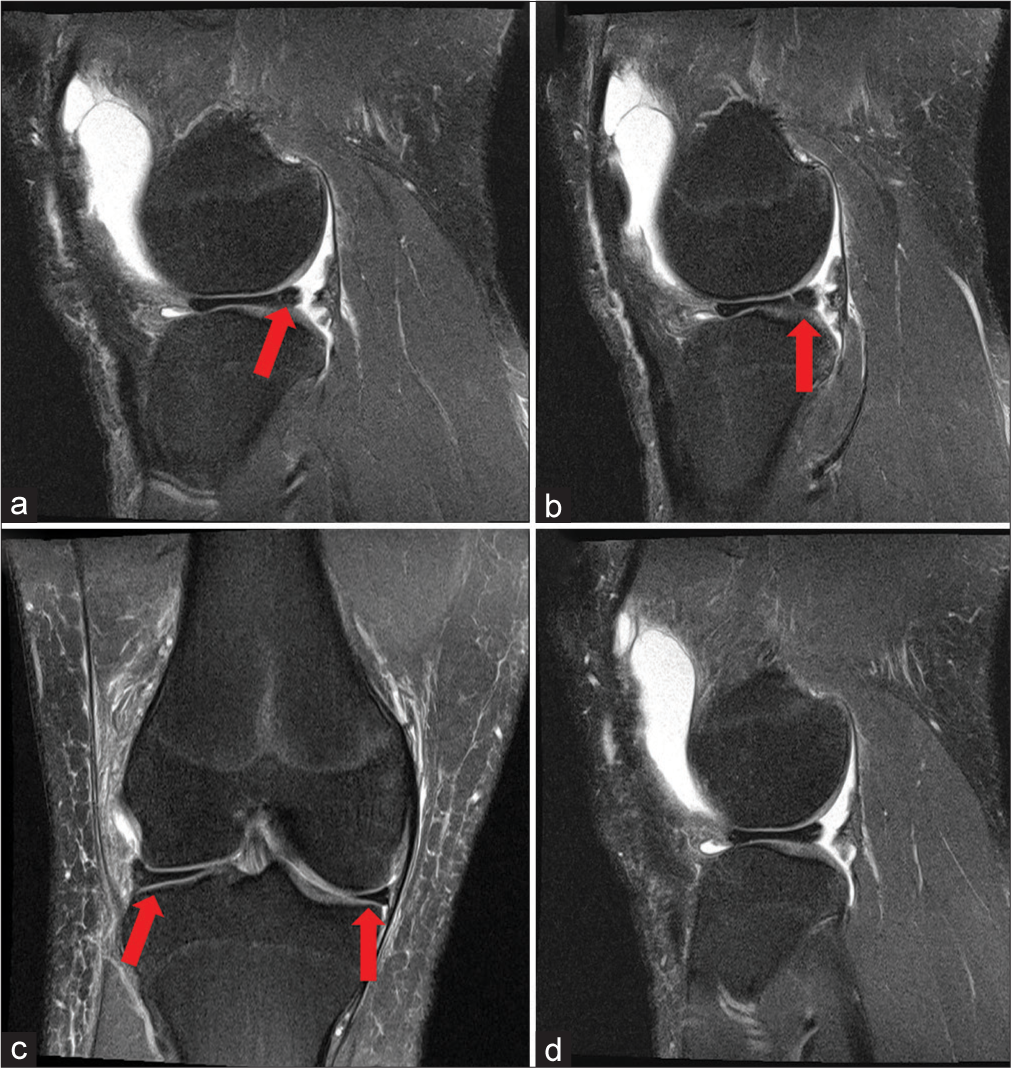
Case 8: Normal ACL (AM and PL bundles)
Teaching point: It is well established that there are two distinct bundles of the ACL, anteriomedial (AM), and posterolateral (PL), with separate femoral and tibial attachment sites.[23-27] The bundles are named by their relative insertional positioning at the ACL footprint of the tibia.[24] Using the clock face over the frontal view of the knee, AM and PL bundles are reported to originate on the posterior part of the medial wall of the lateral femoral condyle at the 10:30/1:30 (left/right knee) and 9:30/2:30 (left/right knee) positions, respectively. Although they have different rupture patterns, with the AM bundle commonly failing at the femoral origin and the PL bundle rupturing at the mid-substance or tibial insertion,[26] the normal separation between the bundles should not be mistaken for a tear on MRI [Figure 9].[23,25]
- A 24-year-old female avid runner presents for evaluation after a minor fall during a trail run. She experienced immediate pain but was able to continue running after a brief rest. On examination, her knee is stable with negative Lachman and pivot-shift tests. She reports no instability or giving way episodes in the past. (a and b) Consecutive T2-weighted coronal images of the left knee demonstrate the anteromedial and posterolateral bundles of the ACL (red arrow). The separate tibial insertion sites can also be appreciated. The distance between the two sites is reported to range from 8 mm to 10 mm. (c) Arthroscopic image of the left knee shows the normal separation in the AM (left) and PL (right) bundles. ACL: Anterior cruciate ligament, (AM: Anteromedial, PL: Posterolateral).
Case 9: Tibial eminence avulsion fracture, Meyers and McKeever type III
Teaching point: Tibial intercondylar eminence fractures are most commonly seen in the pediatric population aged 8–14.[5,7,26,28] Similar to adults, a non-contact pivot shift mechanism of injury causes avulsion fracture of the tibia intercondylar eminence and resultant compromised ACL function.[28] The following modified Meyers and McKeever classification describes the varying degree of injury that can occur and guides treatment. Type I, non-displaced; Type II, displaced anteriorly with an intact posterior cortical hinge; Type III, completely displaced and void of all bony contact; and Type IV, comminuted.[28] This injury can be identified on initial radiographic workup, but MRI is important to determine the extent of damage and comminution [Figure 10].
- A 14-year-old male football player presents after a sudden pivot and deceleration during a match. He recalls a “pop” sound and immediate pain in his left knee, preventing him from continuing to play. On examination, there is significant swelling and tenderness over the anterior aspect of the knee. (a) T1-weighted sagittal magnetic resonance imaging (MRI) of the left knee demonstrating an avulsed osteochondral fragment completely displaced and void of any bony contact (red arrow). Note the proximity of the intermeniscal ligament to the fragment and the fracture bed. This structure, as well as, the anterior horns of medial and lateral menisci can become entrapped in the fracture requiring arthroscopic versus open reduction. The anterior horn of the medial meniscus is involved most commonly. (b) Proton density-weighted fat suppressed coronal MRI of the left knee demonstrates another view of the Meyers and McKeever type III intercondylar eminence fracture (red arrow). The weight-bearing portion of the lateral femoral condyle has increased signal intensity indicative of the bone edema from the acute pivot shift mechanism of injury. (c) Arthroscopic image of the left knee. The fractured tibial intercondylar eminence is elevated by the probe exposing the fracture bed. Repair techniques rely on bone-to-bone healing of the osteochondral fragment to the underlying fracture bed resulting in superior results. (d) Arthroscopic image of the tibial eminence fracture reduced with the intact ACL attached to the fragment. (ACL: Anterior cruciate ligament).
Intra-articular cysts and tumors
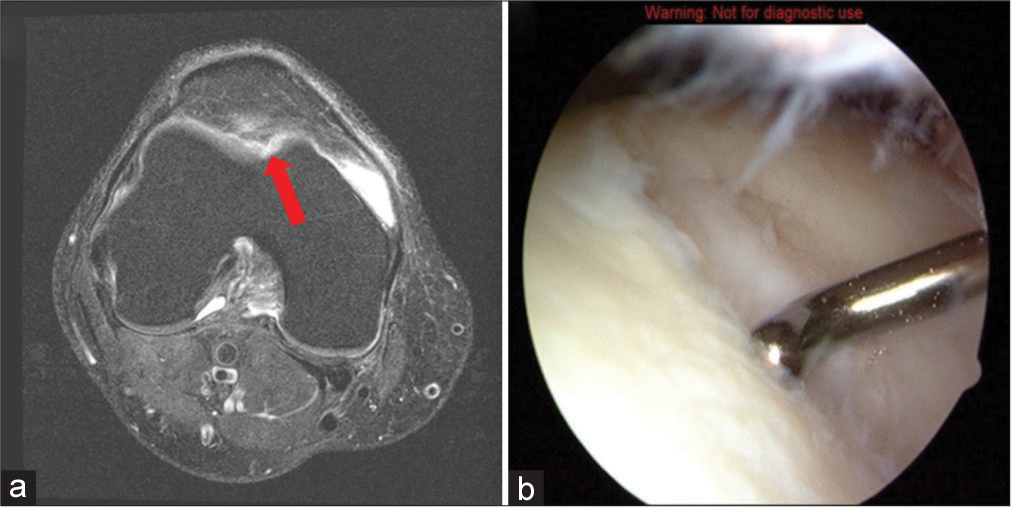
Case 10: Parameniscal cyst of the anterior lateral meniscus
Teaching point: Radiological and arthroscopic studies have confirmed that parameniscal cysts arise from synovial fluid extrusion through underlying meniscal tears.[29-31] A Horizontal cleavage tear is the most commonly described tear pattern associated with cyst formation.[29-31] The goal of treatment is to treat the tear with either meniscal debridement or repair and cyst decompression.[30,31] Of note, there is a reported high frequency (>95%) of medial parameniscal cysts with medial meniscus tears and lateral parameniscal cysts with tears of the body and posterior horn of the lateral meniscus.[29] More recent literature found that 36% of underlying meniscal tears were absent, with cysts adjacent to the anterior horn or 1/3 of the lateral meniscus.[29] If parameniscal cysts exist anterior to the lateral meniscus with no identifiable meniscal tear, other causes should be considered, such as Hoffa fat pad ganglia, intermeniscal ligament tears, or degeneration [Figures 11 and 12].[29]
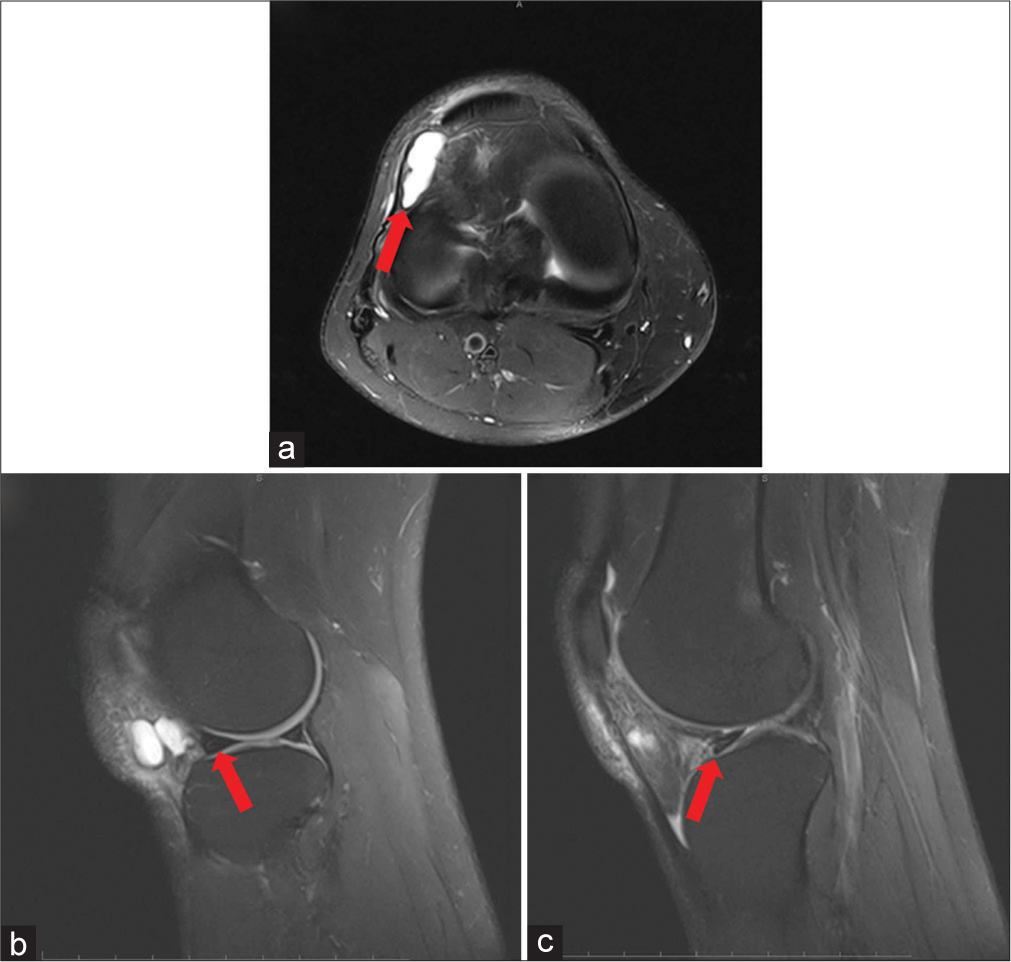
- A 34-year-old female presented with a 6-month history of intermittent lateral knee pain. She denied any prior trauma but mentioned increased discomfort when climbing stairs. On physical examination, a palpable fullness was felt anteriorly at the lateral joint line, without signs of joint effusion. There was tenderness over the area with passive range of motion. (a) T2-weighted axial magnetic resonance (MR) image of a right knee demonstrates the anterior position of the signal-intense, lobular cyst and its relationship to the lateral meniscus and the infrapatellar fat pad (red arrow). (b and c) T2-weighted sagittal MR images of a right knee show the tear in the lateral meniscus and the communication of the joint fluid into the cyst (red arrow).
- (a and b) Arthroscopic images of a large anterior lateral parameniscal cyst (the view is from superior portal looking through patellofemoral joint). The thin-walled, cystic appearance of the fluid-filled mass can be appreciated.
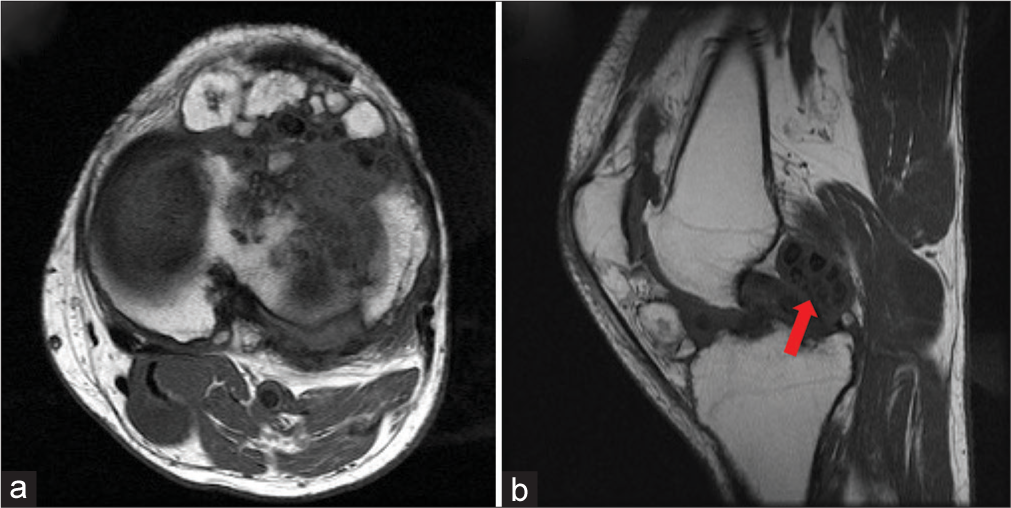
Case 11: Focal pigmented villonodular synovitis (PVNS)
Teaching point: PVNS is a proliferative disease of synovial joints but most commonly affects the knee in young adults.[7] It occurs as a single nodule (focal), a cluster of synovial nodules, or diffuse, boggy proliferative synovitis.[5,7,30,32,33] Initially, diagnosis can be challenging because the most common clinical presentation in the knee is a painless or mildly painful effusion. The nodules can cause mechanical symptoms and mimic meniscal tears, loose bodies, or patellofemoral disorders.[7] PVNS also frequently involves the posterior compartment.[7] When evaluating a knee effusion with an insidious onset, the astute radiologist should be suspicious of PVNS because treatment is surgical.[7,32,33] Current recommendations favor arthroscopic synovectomy.[7,32,33] Lesions in the posterior compartment must be identified on MRI for appropriate preoperative planning, as nonstandard posterior arthroscopic portals are made to access the posterior knee joint and complete the synovectomy [Figure 13].
- A 27-year-old male presented with swelling and discomfort in his right knee for the past 9 months. The pain was insidious in onset and gradually progressive. He denied any history of trauma but mentioned occasional locking and a feeling of “giving way” when walking for extended periods. There was no family history of any joint diseases or inflammatory conditions. The range of motion was reduced, especially in extension, and there was tenderness along the joint line. No warmth or erythema was observed. (a) A T2/proton density-weighted sagittal magnetic resonance image with the typical areas of low signal intensity within the nodule. T1-weighted images will also demonstrate low-intensity signal PVNS nodules. Posterior involvement is common and should be noted. Bony erosion of PVNS nodules is rare but should also be noted. (b) Arthroscopic image of PVNS nodule attached to synovium. The brownish color of the lesion and the surrounding synovium is secondary to hemosiderin leaked from microscopic areas of hemorrhage. Lipid-laden macrophages in the nodules add a yellow tint to the color as well. (PVNS: Pigmented villonodular synovitis).
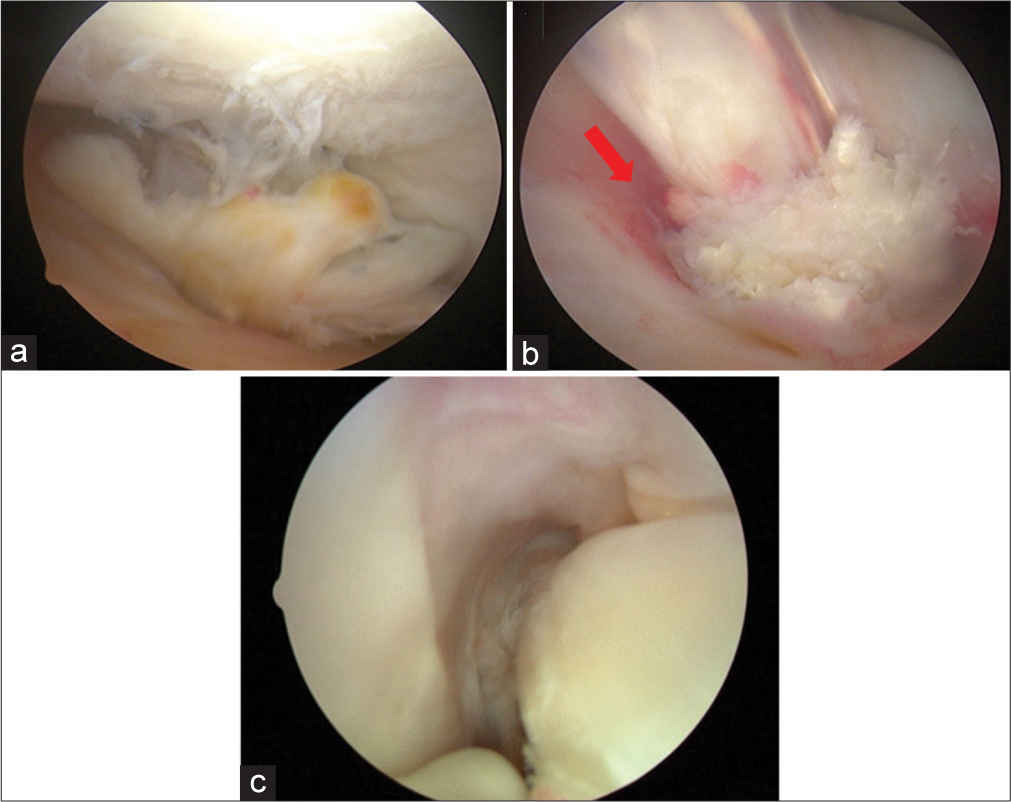
Case 12: Synovial chondromatosis
Teaching point: Synovial chondromatosis is a rare tumor-like disorder characterized by cartilaginous metaplasia of the intimal layer of the synovium, including synovial structures outside of the joint (i.e., tendon sheaths and bursa).[7,34,35] The cartilaginous nodules can detach from the synovium resulting in loose bodies that may undergo secondary calcification and ossification.[14] When viewed arthroscopically, the accumulated nodules resemble a “snowstorm” in the knee joint. Due to its high recurrence rate (>25%) after arthroscopic synovectomy, it is important for radiologists to identify among other benign synovial disorders that can mimic its MRI appearance, such as tumoral calcinosis and PVNS [Figures 14 and 15].[7,34-36]
- A 42-year-old female presented with intermittent pain and swelling in her left knee over the past 2 years. She described episodes where the knee would “lock” momentarily during movement. The pain was non-radiating and occasionally associated with a clicking sensation. No prior trauma or relevant family history was reported. Physical examination revealed a mildly swollen left knee with palpable loose bodies, tenderness along the joint line, and a limited range of motion due to pain during flexion and extension. (a and b) T1-weighted axial and sagittal magnetic resonance images demonstrate multiple cartilaginous lesions with variable appearance, indicating the degree of mineralization. The most common pattern reveals low to intermediate signal intensity with T1-weighting and very high signal intensity with T2-weighting with hypointense calcifications (red arrow).
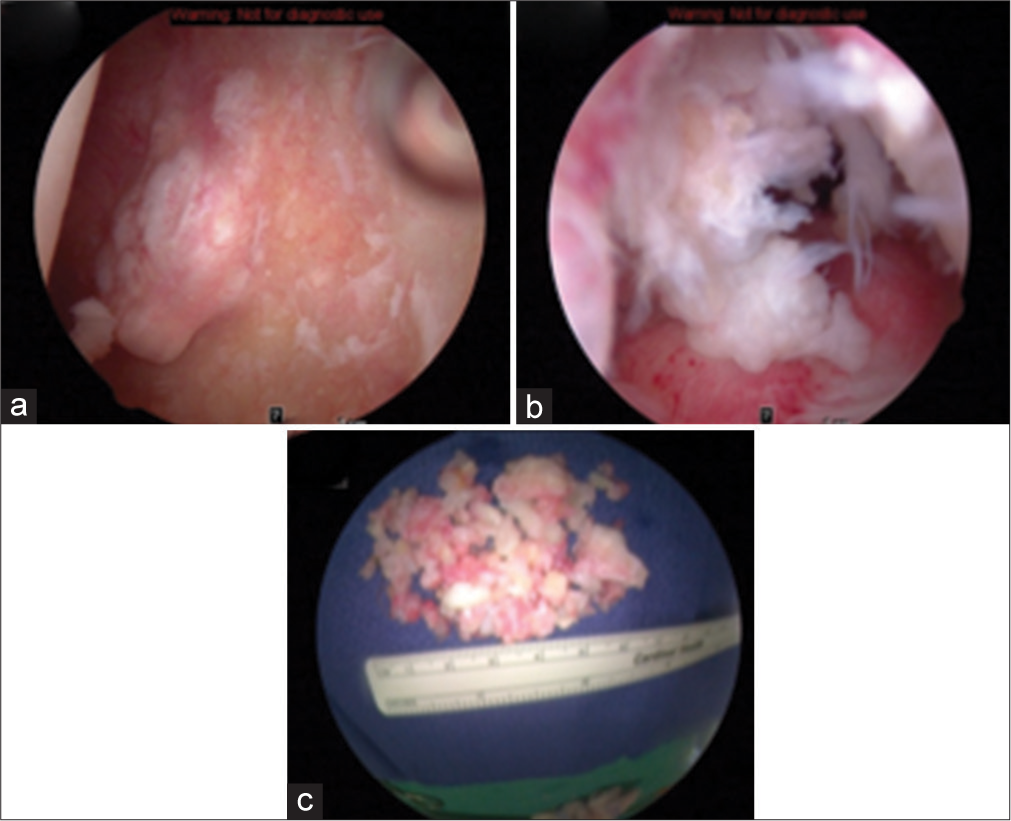
- (a) Arthroscopic image of cartilaginous metaplastic nodule attached to the synovial wall. (b and c) Arthroscopic image shows loose bodies floating in knee joints giving a “snow storm” appearance. Intraoperative image of resected cartilaginous nodules and loose bodies before being sent for the pathological analysis.
Meniscal pathology
The following cases review fundamental MRI principles when interpreting various meniscal tears. Correlating arthroscopic images are included for added appreciation of the pathology present.
Case 13: Acute lateral meniscus retears, unstable
Teaching point: The altered meniscal anatomy can make diagnosing a retear in the postoperative meniscus challenging.[37,38] MR arthrography can increase the sensitivity of meniscal retear detection[7,37,38] but conventional MRI may still provide some utility. Even in a previously debrided or repaired meniscus, abrupt change in the contour of a postoperative meniscus should be met with reasonable suspicion for reinjury [Figure 16].[37]
- A 38-year-old male athlete presents to the clinic with a complaint of sudden onset of sharp pain in his right knee. He describes the pain as localized to the outer aspect of the knee and exacerbated by twisting motions or full knee flexion. The patient recalls a similar episode 1 year ago, for which he underwent arthroscopic lateral meniscus repair. On examination, the lateral joint line was tender to palpation. The McMurray test was positive, eliciting pain and a click during the maneuver. The swelling was noted around the joint, but no ligamentous laxity was observed. The patient described difficulty in fully extending his knee without discomfort. (a and b) T1-weighted coronal and axial magnetic resonance images of a left knee demonstrate a previously partially resected unstable lateral meniscus with a sharp right angle of the anterior one- third. Notice the contour changes drastically as the inner margin is followed on the axial image (red arrow). This finding is indicative of a retear. The extrusion of the thin-rimmed lateral meniscus on the coronal image demonstrates the instability of the reinjured post-operative lateral meniscus. (c and d). Arthroscopic images of a left knee. The thin-rimmed lateral meniscus is indicative of a previous partial meniscectomy. The popliteal tendon (asterisk) can be seen on its course through the popliteal hiatus. The probe is pulling the remaining lateral meniscus into the lateral compartment demonstrating the instability of the damaged meniscus.
Case 14: Displaced lateral meniscus undersurface flap tear
Teaching point: A meniscal flap tear is the result of a short-segment, horizontal meniscal tear with either superior or inferior displacement. MRI findings are subtle, but this tear pattern can be clinically significant, warranting arthroscopic resection. Careful examination of the triangular meniscal shape on sagittal images should be performed to detect abnormalities [Figure 17].
- A 34-year-old female presented with recurrent episodes of locking and giving way of her left knee. She recounted a recent hiking trip where she stumbled on uneven terrain, after which she began to experience intermittent sharp pains in the lateral aspect of her knee. Physical examination revealed joint line tenderness on the lateral side, and her range of motion was limited due to pain during terminal extension. (a and b): T1-weighted sagittal and axial magnetic resonance images of a left knee demonstrating flap tear of anterior 1/3 body of lateral meniscus displaced anteriorly. When evaluating the sagittal cross-section of the meniscus, the difference of the triangular shape between the anterior and posterior meniscus can be appreciated, as well as the displaced fragment anteriorly (red arrow). (c) The correlating arthroscopic image demonstrates the torn fragment from the undersurface of the lateral meniscus flipped into the lateral compartment. One can appreciate the relationship of the displaced fragment in between the lateral femoral condyle and lateral tibial plateau, and the potential to become symptomatic.
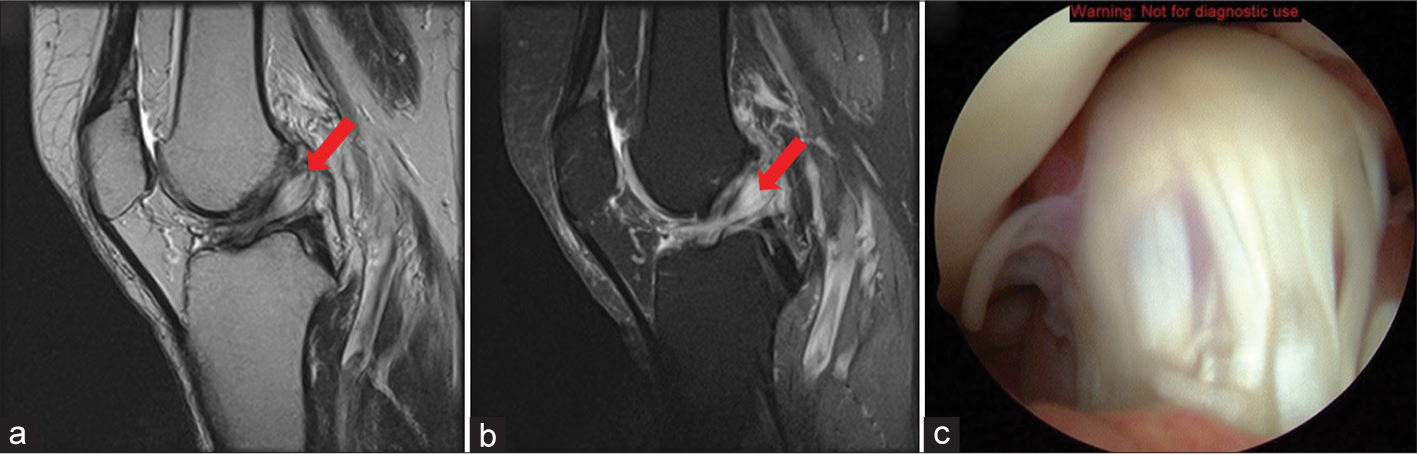
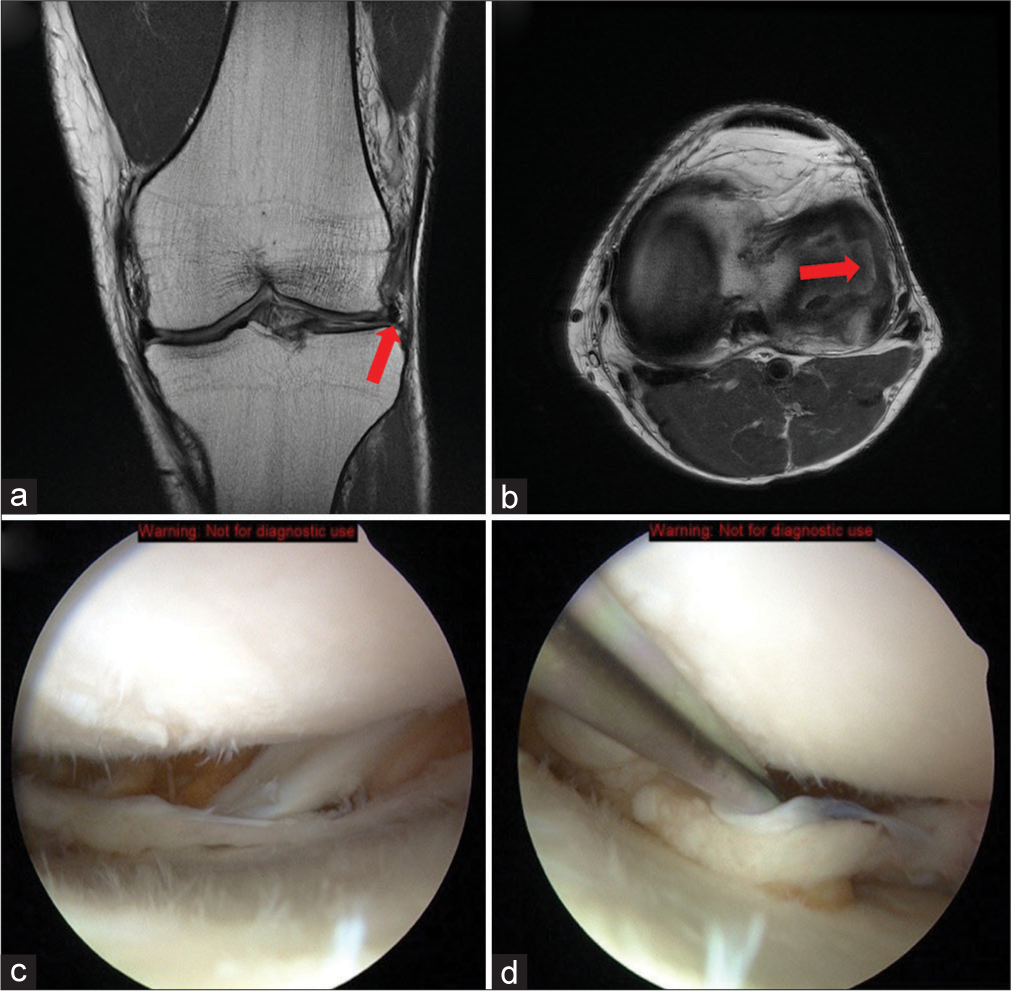
Case 15: Displaced, large medial meniscus horizontal tear
Teaching point: Flap tears of the meniscus can continue propagating without treatment and become large floating pieces in the joint, potentially causing mechanical symptoms.[7] Again, abrupt changes in the thickness of the meniscus suggest tears and detailed descriptions of the locations of torn fragments should be made to facilitate arthroscopically identification [Figure 18].[38]
- A 21-year-old male presented with complained of persistent medial knee pain and occasional clicking sounds in his right knee, exacerbated when arising from a seated position. He recalled a twisting injury to the knee while playing football 2 months prior. Physical examination revealed pronounced joint line tenderness medially and a positive McMurray test. (a and b) T1-weighted axial and sagittal magnetic resonance images of the left knee demonstrating a large flap tear of the medial meniscus displaced into the joint space (red arrow). The change in contour and thickness from the anterior one-third to the mid-body of the medial meniscus on the axial cut indicates the presence of a tear. The detached fragment folds in the joint towards the intercondylar notch when following its path. (c) Arthroscopic image of the correlating left knee demonstrates the large flap tear floating in the knee. (d) After debridement of the unstable, free-floating flap tear fragment, the extent of delamination of the superior portion of the medial meniscus can be appreciated.
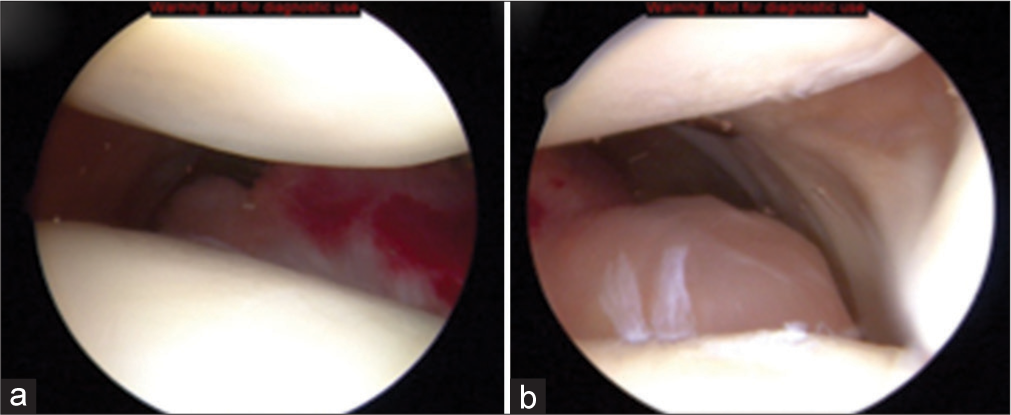
Case 16: Acute radial tear of the lateral meniscus mid-body
Teaching point: Acute radial tear of the mid-body of the lateral meniscus is often a result of the pivot shift mechanism and is associated with acute ACL rupture.[7,39,40] This particular tear pattern has detrimental effects on the contact pressures experienced by the articular cartilage secondary to the disruption of the circumferential collagen fibers of the meniscus.[41] Identifying meniscal tears with concomitant ACL ruptures is important because if repairable, there is a greater healing potential of the meniscal repair due to the release of growth factors when drilling bone tunnels for ACL reconstruction [Figure 19].[7]
- A 22-year-old male football player presented with acute-onset lateral knee pain, following a sudden pivot on his left leg during practice. He described the pain as sharp, localized to the lateral aspect of the knee. There was no history of previous knee injuries. On examination, there was notable tenderness along the lateral joint line without significant effusion. (a) T1-weighted axial magnetic resonance image of the right knee demonstrates a large mid-body radial tear of the lateral meniscus (red arrow). The tear is complete extending from the inner margin to the periphery. There is a concomitant ACL tear, as well (not shown). (b and c) The correlating arthroscopic images of the right knee detail the extension of the tear into the red-red zone of the meniscus and the capsulomeniscal junction. The bleeding ends of the torn lateral meniscus are appreciated in (b). An excellent all-inside suture repair is achieved in (c). This technique has been shown to be promising and an effective alternative to partial meniscectomy. (ACL: Anterior cruciate ligament).
Case 17: Diagnosis: Lateral discoid meniscus, radial tear
Teaching point: Being able to see the meniscal body on three or more consecutive MR sagittal images is suggestive of discoid meniscus.[1]
Arthroscopically, a thick meniscal rim is present even after cauterization [Figures 20 and 21].
- A 26-year-old male basketball player presented with recurrent episodes of locking and discomfort in his right knee, especially when performing squatting motions. He mentioned a history of similar episodes in the past, but they usually resolved with rest. However, the current episode has persisted longer. Physical examination revealed tenderness over the lateral joint line and a positive McMurray’s test (left to right). (a, b) Two consecutive T2-weighted sagittal images of a right knee demonstrate a thick mid-body of the lateral meniscus with a small, symptomatic radial tear posteriorly (red arrows). (c) A stark comparison in size is made between the discoid lateral meniscus and the smaller medial meniscus in the bottom left coronal image (red arrows). Extension of the lateral meniscus over the majority of the lateral tibial plateau can be appreciated in the coronal view. Image (d) is another consecutive T2-weighted sagittal image of a right knee demonstrating a thick mid-body of the lateral meniscus with a small, symptomatic radial tear posteriorly.
- (a) An arthroscopic image of the lateral discoid meniscus “draping” over the lateral tibial plateau. (b) Images demonstrating the saucercized lateral meniscus. The increased thickness of the residual meniscus is evident.
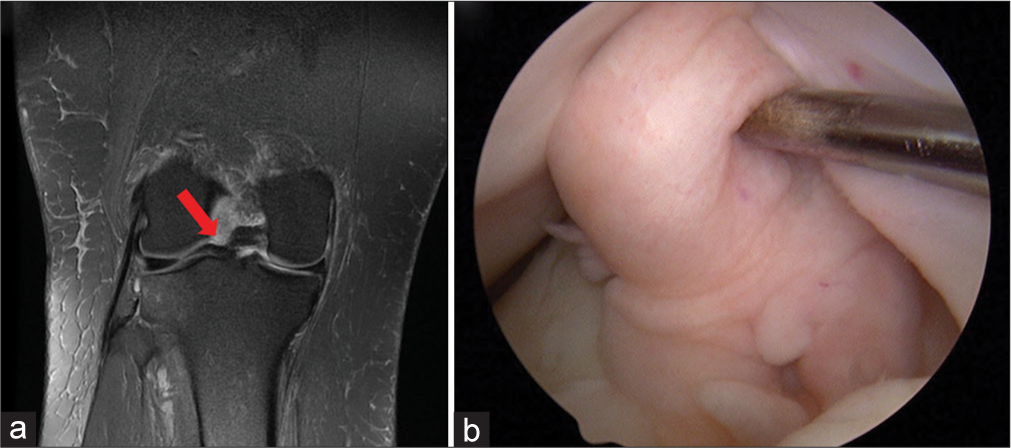
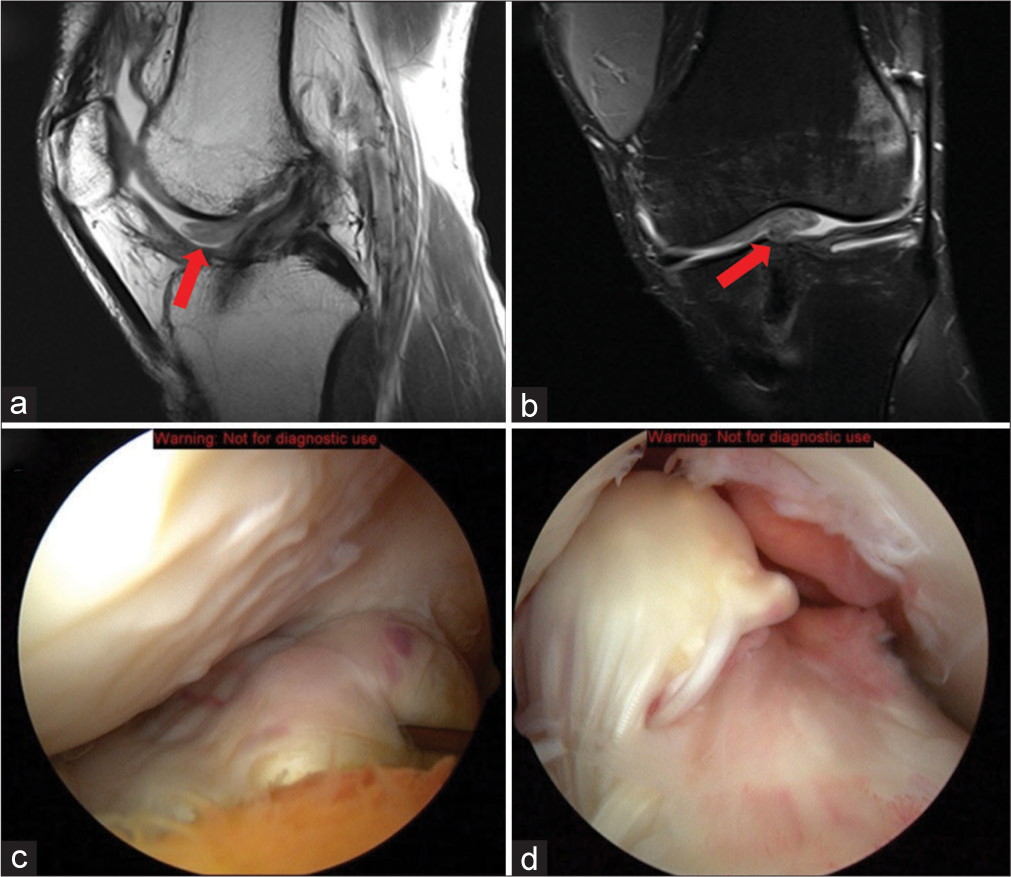
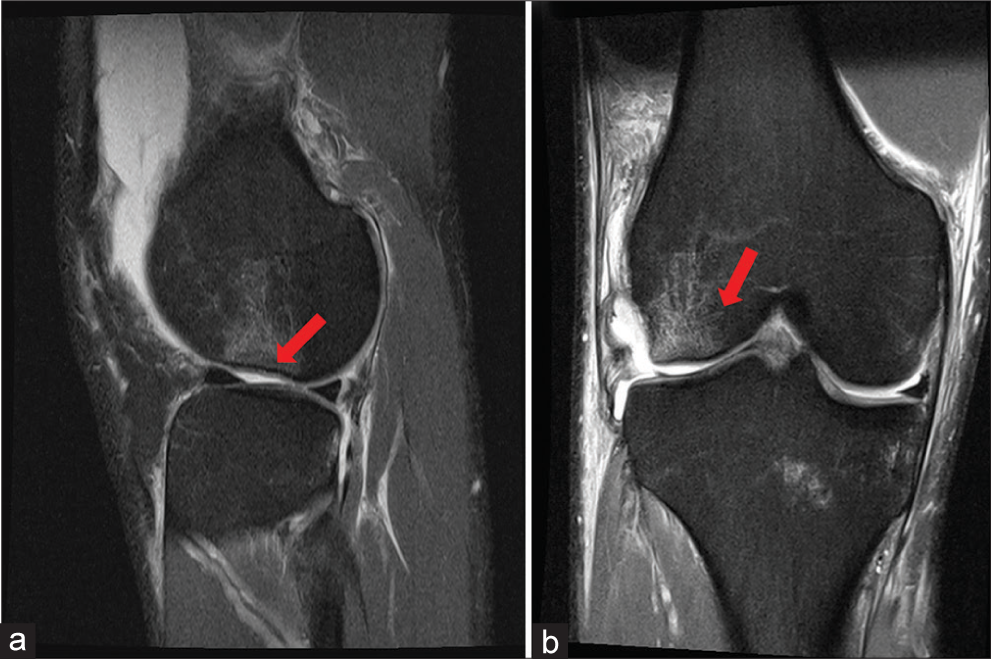
Case 18: Lateral meniscus anterior horn tear, degenerative
Teaching point: Degenerative tears arthroscopically can have a frayed appearance with correlating increased intrasubstance signal intensity on MRI.[7]
Isolated anterior horn lateral meniscus tears are rare but do occur [Figure 22].
- A 58-year-old female office worker complained of persistent pain in her left knee, particularly noticeable when ascending stairs or after prolonged sitting. She described the pain as a dull ache, which occasionally felt sharp with certain movements. She denied any history of trauma but noted the discomfort gradually increased over the past year. On examination, there was mild swelling of the knee joint, tenderness over the lateral joint line, and limited range of motion due to pain. (a and b) Coronal and sagittal T2-weighted images demonstrate increased signal intensity of the lateral meniscus anterior horn suggestive of a frayed, degenerative tear (red arrow). (c) Correlating arthroscopic image shows the frayed and degenerative appearance of the anterior horn lateral meniscus in a right knee. (d) The debrided anterior horn lateral meniscus.
Case 19: Medial meniscus tear, bucket handle type
Teaching point: The “Double PCL sign” is a characteristic finding of bucket handle medial meniscus tears.[7] This tear can cause significant mechanical symptoms [Figure 23].
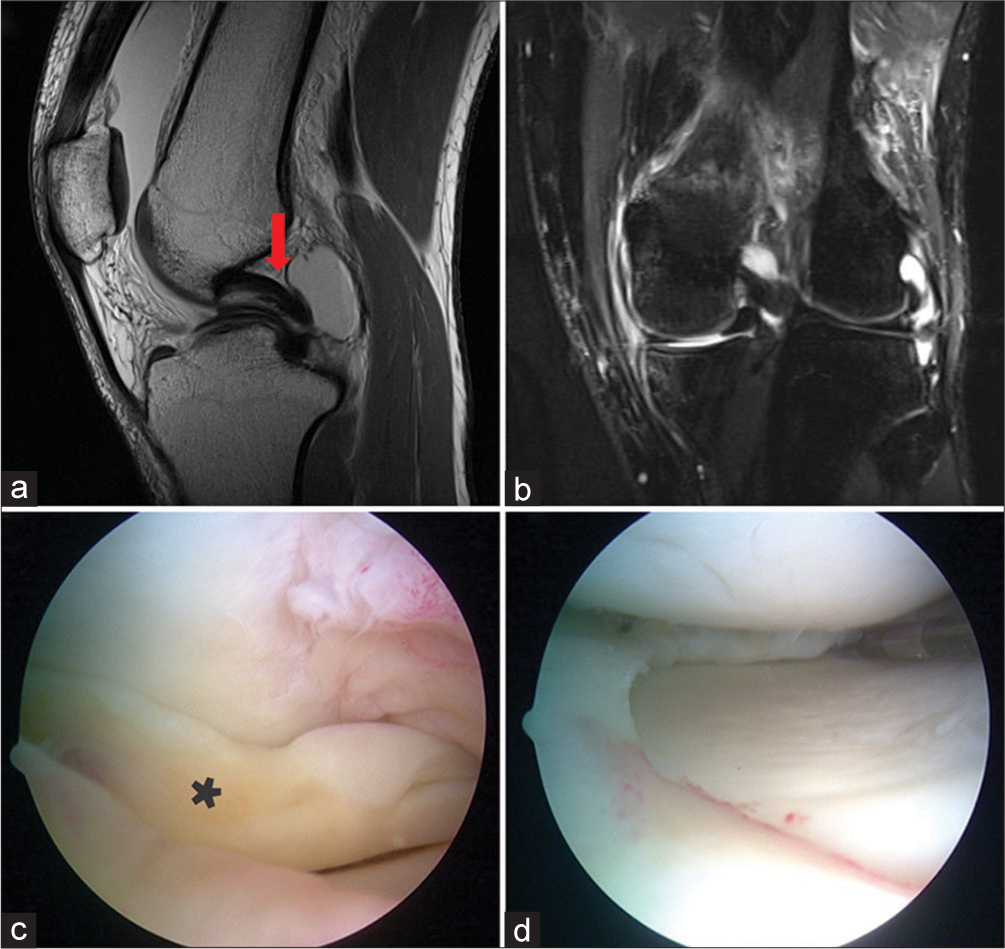
- A 35-year-old female presented to the clinic after experiencing a sudden, sharp pain in her left knee when she was descending a flight of stairs at her home. She recalled missing a step, which caused her knee to twist awkwardly. Immediately after the incident, she observed swelling in the knee and had difficulty fully extending the leg. (a and b) Sagittal T1 and coronal T2-weighted magnetic resonance imaging images demonstrate the classic medial meniscus bucket handle tear patterns. The “Double PCL sign” (red arrow) is evident in (a) (red arrow) with residual attachment of the torn fragment to the posterior horn. (b) The bucket handle portion of the medial meniscus folded underneath the medial femoral condyle. The coronal image also shows the thin medial meniscal rim which further confirms the presence of a tear. (c and d) Arthroscopic images of the medial compartment. In (c), the medial meniscus (asterisk) is folded underneath the medial femoral condyle above. The tear is debrided away leaving behind a stable medial meniscus in (d). (PCL: Posterior cruciate ligament.)
Chondral pathology
Case 20: Grade I chondral injury (Chondromalacia)
Teaching point: Swelling and softening of articular cartilage are much more prone to further damage and degradation. Commenting on areas of chondromalacia allows the arthroscopist to understand how fragile the articular surface is before surgery [Figure 24].
- A 28-year-old male runner, presented with a persistent dull ache in his right patella, particularly noticeable after long runs or descending stairs. There was no history of trauma or previous knee injuries. On examination, there was tenderness on the patellar facets with mild effusion but no ligamentous instability. Crepitus was noted during knee flexion and extension. (a) Coronal T2-weighted image a left knee demonstrates focal area of increased thickness and decreased signal intensity of the articular cartilage overlying the lateral tibial plateau representative of chondromalacia (red arrow). (b) Arthroscopic image of the lateral compartment of a left knee. Examination of the tibial articular surface of the lateral compartment finds soft and swollen articular cartilage. This is indicated by the metal probe sinking into the abnormally soft tissue.
Case 21: Grade II and III chondral injury
Teaching point: Outerbridge grade II and III cartilage lesions can be difficult to differentiate, but size dimensions should be reported to allow the surgeon to prepare for a microfracture technique or simple debridement of the unstable portions of the lesion [Figure 25].[7]
- A 42-year-old female presented complaining of recurrent episodes of sharp pain in her left knee, exacerbated by prolonged walking or standing. She also reported occasional catching sensations but denied any locking or giving way. The pain had been progressively worsening over the past year. She recalled a minor twisting injury to the knee about 18 months ago, but there was no significant swelling or bruising at the time. (a) Coronal T2-weighted image of a right knee demonstrates grade II and III chondral lesions of the femoral and tibial surfaces of the lateral compartment (red arrow). (b and c) demonstrate a grade II chondral lesion of the lateral femoral condyle. (d) A significantly fibrillated grade III chondral lesion of the tibial surface.
Case 22: Grade IV chondral injury, femoral trochlea
Teaching point: Malalignment, ligamentous laxity, and location of full-thickness defects of cartilage are deciding factors in the surgical treatment of cartilage defects in the knee. Correction of alignment and/or ligamentous instability would precede any cartilage restorative procedures or be performed concomitantly.[7] Thus, it is important for radiologists to specify the location of high-grade lesions and other knee derangements for pre-operative planning [Figure 26].
- A 56-year-old male executive presented with complaints of persistent deep-seated pain in his right knee and a grinding sensation, especially while ascending or descending stairs. He reported no specific history of trauma but mentioned frequent participation in recreational running over the past two decades. Recently, he noticed that the pain would intensify after periods of prolonged sitting, often referred to as the “theater sign.” (a) Axial T2-weighted image demonstrates a full-thickness articular cartilage defect of the femoral trochlea (red arrow). (b) Arthroscopic image of the patellofemoral joint reveals a large, full thickness, and femoral trochlear chondral lesion. The 2 mm metal probe tip length provides a reference for the actual size of the defect. The calcified cartilage layer at the base of the lesion was debrided, and the defect was treated with a microfracture technique (not shown).
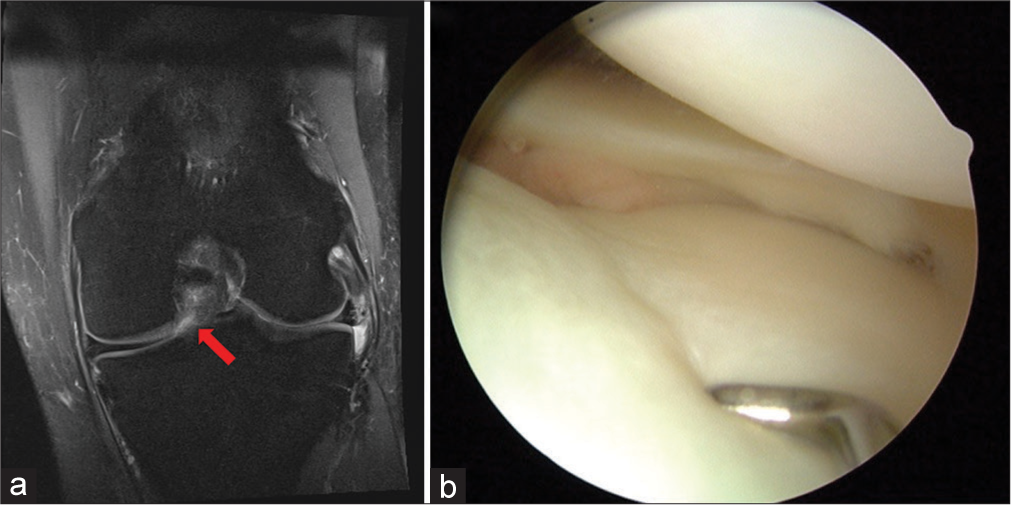
Case 23: Chondral impaction fracture, lateral femoral condyle
Teaching point: Subchondral depression from a pivot shift injury is technically a fracture and should be treated as such. Findings may be subtle and can be mistaken for a bone bruise, but any depression or loss of the normal distal femoral contour should be appreciated and reported. Chondral impaction fractures should be treated with a period of non-weight bearing in addition to addressing potential concomitant injuries from the pivot shift mechanism, that is, ACL and meniscal tears [Figure 27].
- A 38-year-old female dance instructor presented to the orthopedic clinic with a 3-week history of acute-onset right knee pain. She described a specific event during a dance routine where she landed awkwardly on her extended leg, causing immediate pain on the lateral aspect of her right knee, without any associated swelling or locking. The pain was localized to the lateral aspect of his right knee. (a and b) T2-weighted sagittal and coronal of a right knee. The increased signal intensity of the lateral femoral condyle subchondral bone is characteristic of the bone bruising associated with a pivot shift injury (red arrows). This should help focus attention on the contour of the articular cartilage and subchondral layer. There is a slight depression or loss of the normal round contour of the lateral femoral condyle. This should be noted along with other structures damaged in the pivot shift injury mechanism.
CONCLUSION
It is essential for radiologists to become familiarized with the classic arthroscopic appearance of common knee pathologies so that the MRI reports can be more valuable to the referring orthopedic surgeon regarding preoperative planning and treatment discussions with the patients.
With an improved understanding of the arthroscopic appearance of commonly seen findings on MRI, radiologists will be able to paint orthopedic surgeons a more functional picture of what they should expect to see intraoperatively, enabling the orthopedic surgeon to formulate a more educated preoperative surgical approach to the pathology at hand and potentially improve surgical outcomes.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that they have used artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript or image creations.
Financial support and sponsorship
Nil.
References
- Complications after arthroscopic knee surgery. Am J Sports Med. 2014;42:292-6.
- [CrossRef] [PubMed] [Google Scholar]
- Update on the risks of complications after knee arthroscopy. BMC Musculoskelet Disord. 2018;19:179.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical practice. Anterior cruciate ligament tear. N Engl J Med. 2008;359:2135-42.
- [CrossRef] [PubMed] [Google Scholar]
- Cost effectiveness of anterior cruciate ligament reconstruction in young adults. Clin Orthop Relat Res. 1999;367:272-82.
- [CrossRef] [Google Scholar]
- Epidemiology of anterior cruciate ligmaent Reconstruction: Trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91:2321-28.
- [CrossRef] [PubMed] [Google Scholar]
- A comprehensive review of partial anterior cruciate ligament tears. J Bone Joint Surg Am. 2009;91:198-208.
- [CrossRef] [PubMed] [Google Scholar]
- Insall and Scott surgery of knee (4th ed). Philadelphia, PA: Churchill Livingstone Elsevier; 2006.
- [Google Scholar]
- Current concept of partial anterior cruciate ligament ruptures. Orthop Traumatol Surg Res. 2010;96(8 Suppl):S109-18.
- [CrossRef] [PubMed] [Google Scholar]
- Partial tears of the anterior cruciate ligament. Progression to complete ligament deficiency. J Bone Joint Surg Br. 1989;71:825-33.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of partial tears of the anterior cructiate ligament of the knee: Value of the MR imaging. AJR Am J Roentgenol. 1995;165:893-7.
- [CrossRef] [PubMed] [Google Scholar]
- The phenomenon of “ligmentization”: Anterior cruciate ligament reconstruction with autogenous patellar tendon. J Orthop Res. 1986;4:162-72.
- [CrossRef] [PubMed] [Google Scholar]
- “Empty wall” and “vertical strut” signs of ACL insufficiency. Arthroscopy. 1989;5:137-40.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament injury: MR imaging diagnosis and patterns of injury. Radiographics. 1992;12:901-15.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures. Arthroscopy. 2001;17:445-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthrofibrosis of the knee. J Am Acad Orthop Surg. 2007;15:682-94.
- [CrossRef] [PubMed] [Google Scholar]
- Intra-articular gnanglion cysts of the knee joint: A report of 85 cases and review of the literature. Knee Surg Sports Traumatol Arthosc. 2004;12:123-9.
- [CrossRef] [PubMed] [Google Scholar]
- Ganglion cysts of the anterior cruciate ligament: A case report and review of the literature. Arthroscopy. 1994;10:110-2.
- [CrossRef] [PubMed] [Google Scholar]
- Symptomatic Ganglion cyst within the substance of the anterior cruciate ligament. Arthroscopy. 1995;11:612-5.
- [CrossRef] [PubMed] [Google Scholar]
- Ganglion cysts of the anterior cruciate ligament. Arthroscopy. 1994;10:574-5.
- [CrossRef] [PubMed] [Google Scholar]
- Intraligamentous ganglion cysts of the anterior cruciate ligament: MR findings with clinical and arthroscopic correlations. J Comput Assist Tomogr. 1996;20:80-4.
- [CrossRef] [PubMed] [Google Scholar]
- Arthrofibrosis of the knee. J Am Acad Orthop Surg. 2007;15:682-94.
- [CrossRef] [PubMed] [Google Scholar]
- Localized anterior arthrofibrosis (Cyclops lesion) after reconstruction of the anterior cruciate ligament: MR imaging findings. AJR Am J Roentgenol. 1995;165:383-5.
- [CrossRef] [PubMed] [Google Scholar]
- Cyclops syndrome: Loss of extension following intra-articular anterior cruciate ligament reconstruction. Arthroscopy. 1990;6:171-8.
- [CrossRef] [PubMed] [Google Scholar]
- Current knowledge in the anatomy of the human anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18:1075-84.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament anatomy and function relating to anatomic reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14:982-92.
- [CrossRef] [PubMed] [Google Scholar]
- Intraarticular rupture pattern of the ACL. Clin Orthop Relat Res. 2007;454:48-53.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy of the anterior cruciate ligament with regards to its two bundles. Clin Orthop Relat Res. 2007;454:35-47.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric tibial eminence fractures: Evaluation and management. J Am Acad Orthop. 2010;18:395-405.
- [CrossRef] [PubMed] [Google Scholar]
- Association of parameniscal cysts with underlying meniscal tears as identified on MRI and arthroscopy. Am J Roentgenol. 2011;196:W180-6.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of meniscal cysts. Arthroscopy. 1993;9:591-5.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of cysts of the lateral meniscus. J Bone Joint Surg Br. 1993;75B:299-302.
- [CrossRef] [PubMed] [Google Scholar]
- Pigmented villonodular synovitis in joints. J Surg Oncol. 2011;103:386-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic treatment of pigmented villodular synovitis of the knee. Arthroscopy. 1999;15:613-7.
- [CrossRef] [PubMed] [Google Scholar]
- Synovial chondromatosis of four compartments of the knee: Medial and lateral tibiofemoral spaces, patellofemoral joint and proximal tibiofibular joint. Knee Surg Traumatol Arthrosc. 2007;15:753-5.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of synovial chondromatosis with radiologicpathologic correlation. Radiographics. 2007;27:1465-88.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging of the postoperative meniscus of the knee. Semin Musculoskelet Radiol. 2002;6:35-46.
- [CrossRef] [PubMed] [Google Scholar]
- MR diagnosis of recurrent tear in the knee: Value of intraarticular contrast material. AJR Am J Roentgenol. 1993;161:821-5.
- [CrossRef] [PubMed] [Google Scholar]
- Inferiorly displaced flap tears of the medial meniscus: MR appearance and clinical significance. AJR Am J Roentgenol. 2000;174:161-4.
- [CrossRef] [PubMed] [Google Scholar]
- Meniscal repair for radial tear of the midbody of the lateral meniscus. Am J Sports Med. 2010;38:2472-6.
- [CrossRef] [PubMed] [Google Scholar]
- Different patterns of meniscal tears in acute anterior cruciate ligament (ACL) ruptures and in chrronic ACL-deficient knees: Classification, staging and timing of treatment. Knee Surg Sports Traumatol Arthrosc. 1995;3:130-4.
- [CrossRef] [PubMed] [Google Scholar]







