Translate this page into:
Clinical application of medical adhesive in endovascular embolization treatment of peripheral pseudoaneurysm

*Corresponding author: Li-Ping Jiang, Department of Interventional Diagnosis and Treatment, The First Affiliated Hospital of Shihezi University, Shihezi, Xinjiang Province, China. 1044152190@qq.com
-
Received: ,
Accepted: ,
How to cite this article: Jiang L, Wang Q. Clinical application of medical adhesive in endovascular embolization treatment of peripheral pseudoaneurysm. J Clin Imaging Sci. 2024;14:2. doi: 10.25259/JCIS_120_2023
Abstract
Objectives:
This study explores the clinical application value of medical adhesive in endovascular embolization treatment of peripheral pseudoaneurysm.
Material and Methods:
This was a retrospective review on 31 patients with peripheral pseudoaneurysm treated with medical adhesive endovascular embolization at the First Affiliated Hospital of Shihezi University from July 2021 to July 2023. Follow-up for 3–6 months was to observe the clinical efficacy and postoperative complications of medical adhesive embolization treatment.
Results:
A total of 32 pseudoaneurysms were embolized in 31 patients with peripheral pseudoaneurysms. All pseudoaneurysms originated from visceral arteries. Among them, 29 pseudoaneurysms were embolized with medical adhesive alone, and three pseudoaneurysms were embolized with coil-assisted medical adhesive. After endovascular embolization with medical adhesive, all pseudoaneurysms were successfully embolized. Technical success was 100%. All patients experienced cessation of bleeding after endovascular embolization with medical adhesive, and there were no serious post-operative complications. Clinical success was 100%. During the follow-up period, two patients experienced recurrent bleeding but no pseudoaneurysm recurrence was observed.
Conclusion:
Endovascular medical adhesive embolization is a safe and effective method for treating pseudoaneurysm, with high hemostatic efficiency and permanent occlusion of the pseudoaneurysm after embolization, which is worthy of clinical promotion and application.
Keywords
Pseudoaneurysm
Medical adhesive
Visceral artery
Interventional embolization
INTRODUCTION
Pseudoaneurysm is a capsule formed by rupture of an arterial blood vessel that communicates with the arterial blood vessel. It does not have a true vascular wall structure. It can be caused by various reasons such as trauma, infection, and tumor.[1,2] Pseudoaneurysms, especially those originating from visceral arteries such as the chest, abdomen, and pelvic cavity, must be treated urgently once they are formed. The mortality rate of those untreated patients with visceral pseudoaneurysms could be as high as 100%.[3] With the development of vascular intervention technology, endovascular embolization has gradually replaced surgery as the preferred treatment method for visceral pseudoaneurysms.[4,5] Traditional embolic materials include solid embolic materials such as micro coil, gelatin sponge, and embolic microspheres, which have achieved certain clinical efficacy. However, such embolic materials have a certain probability of recurrence of pseudoaneurysm.[3] Permanent liquid embolic agent medical adhesive has the characteristics of good fluidity and permanent embolism and has certain advantages in embolization of difficult to super select pseudoaneurysms to avoid recurrence. At present, there are few related clinical studies.[6,7] This study retrospectively analyzed the clinical data of patients with peripheral pseudoaneurysms treated with vascular medical adhesive embolization in our hospital from July 2021 to June 2023 and analyzed the effectiveness and safety of medical adhesive embolization in the treatment of pseudoaneurysms.
MATERIAL AND METHODS
This was a retrospective collection of clinical data of patients with peripheral pseudoaneurysm treated with medical adhesive endovascular embolization at the First Affiliated Hospital of Shihezi University from July 2021 to June 2023. The inclusion criteria were as follows: (i) patients with abdominal or pelvic bleeding symptoms caused by various reasons; (ii) patients who have undergone emergency angiography to confirm the presence of peripheral pseudoaneurysm and undergo interventional embolization treatment; and (iii) the main embolic material is medical adhesive; the exclusion criteria were as follows: (i) patients who are allergic to iodine contrast agents; (ii) patients who refuse intervention treatment; (iii) patients who have undergone angiography but have not undergone embolization; and (iv) patients with pseudoaneurysm undergoing endovascular isolation treatment with covered stents. All patients met the indications for interventional surgery and signed an informed consent form before surgery.
Procedural technique
The patient was placed in a supine position, routinely disinfected and draped. After local anesthesia, an improved Seldinger technique was used to perform right femoral artery puncture (if the right femoral artery area is not suitable as the puncture point due to wounds or catheterization, left femoral artery puncture can be performed), and a 5F arterial sheath (KDL-YX-016-01, Shanghai Kangdeli Medical Equipment Co., Ltd) could be inserted. Select a suitable catheter for routine arteriography to clarify the bleeding site, pseudotumor morphology and structure, and the compensation of the host artery and its collateral branches. Inject medical adhesive (α-N-butyl cyanoacrylate, Beijing Kangpaite Medical Equipment Co., Ltd) into the cavity of the pseudoaneurysm using microcatheter (MC-PE27131, with guide wire, Talmo Medical Products Shanghai Co., Ltd) super-selective embolization therapy [Figure 1]. Those pseudoaneurysms that were located at the distal end of artery could not be super-selective through microcatheters, could be super-selective through microcatheters to the distal end of the parent artery of the pseudoaneurysm, and embolized with medical adhesive who have been assessed by digital subtraction angiography (DSA) that embolization of the parent artery will not cause target organ ischemia or significant functional damage [Figures 2 and 3]. Mix medical adhesive and iodine oil (Iodized poppy seed oil fatty acid ethyl ester, 480 mg I/mL, Jiabei Medical Equipment Shanghai Co., Ltd) in a ratio of 1:2~1:6, and rinse the microcatheter with 3–5 mL of 5% glucose injection before embolization to avoid sticking. When there were important blood vessels that are difficult to avoid with microcatheters, protective embolization can be performed on the important blood vessels using coils (MWCE-18-14-6-NESTER, 14 cm × 4/6 mm, Cook Company, USA), and then after medical adhesive flew into a pseudoaneurysm, complete embolization could be achieved [Figure 4]. Then perform DSA again to clarify the effect of vascular embolism.
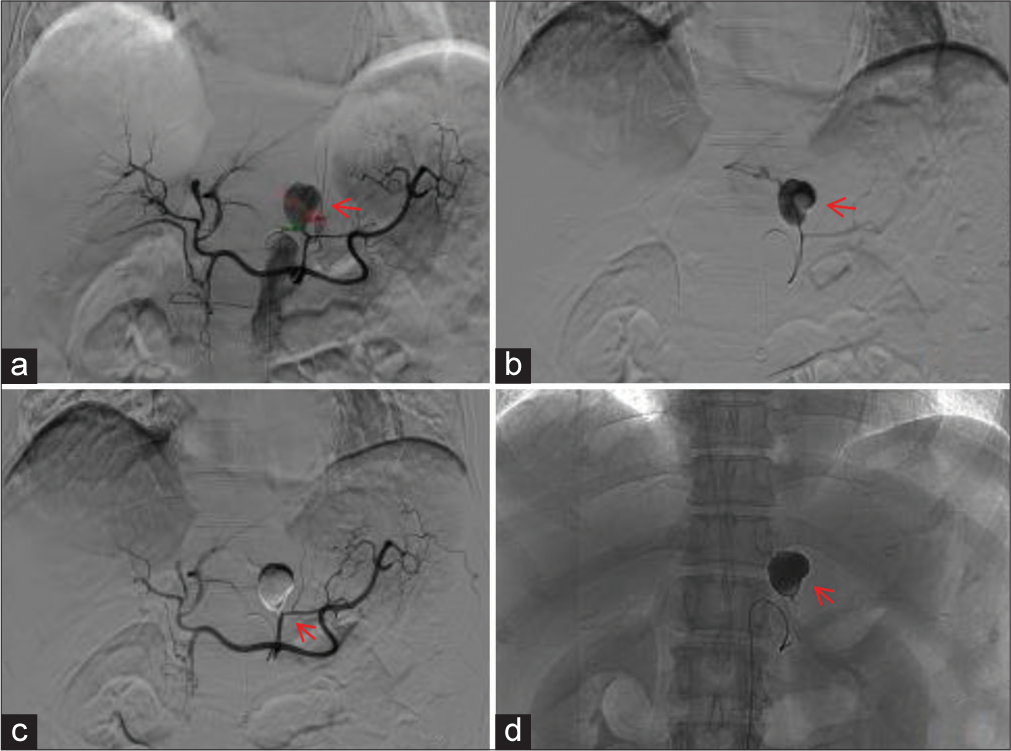
- A 64 year old female developed a pseudoaneurysm at the left gastric artery and underwent medical adhesive embolization treatment by super-selective insertion of a microcatheter into the pseudoaneurysm cavity. (a) Abdominal trunk angiography. The red arrow showed a bag-like protrusion of the proximal branch of the left gastric artery; (b) microcatheter was placed in the left gastric artery pseudoaneurysm. The red arrow showed the pseudoaneurysm ruptured and the contrast agent overflowed; (c and d) recheck the angiography. The red arrow of sub figure c showed the main trunk of the left gastric artery and other normal branches were preserved, and the red arrow of sub figure d showed the medical adhesive inside the tumor cavity was perfectly cast.

- A 54-year-old male developed a pseudoaneurysm that were located at the distal end of the right hepatic artery could not be super-selective through microcatheters after undergoing liver radiofrequency ablation treatment. (a and b) Hepatic artery angiography. The red arrows in the sub-figures a and b showed the pseudoaneurysm of the distal branch of the right hepatic artery; (c) microcatheter were super-selected in the distal branch of the right hepatic artery. The red arrow showed the medical adhesive were injected into the supply artery of pseudoaneurysm through microcatheter; (d) Upon re-examination of the angiography, the red arrow showed that the pseudoaneurysm cavity was cast with medical adhesive, and the pseudoaneurysm and its supplying artery were occluded.

- A 55-year-old woman developed a pseudoaneurysm that were located at the distal end of the lower pole branch of the left renal artery could not be super-selective through microcatheters; (a) Renal artery angiography. The red arrow showed a pseudoaneurysm shadow at the distal end of the lower pole branch of the left renal artery; (b) The red arrow showed that the microcatheter could not but super-selected into the distal branch of the lower pole branch of the left renal artery; (c and d) on reexamination of the angiography. The red arrow of sub-figure c and d showed that the pseudoaneurysm disappeared and the supplying artery was occluded.

- A 52-year-old female patient with cervical cancer suffered from rupture of a pseudoaneurysm in the right internal genital artery, resulting in massive vaginal bleeding. (a) Angiography showed a bag-like protrusion (the red arrow) of the distal branch of the right internal genital artery; (b) microcatheter could not but super-selected into the proximal segment of internal genital artery. The red arrow showed the pseudoaneurysm rupture and contrast agent leakage; (c) the red arrow showed that medical adhesive was injected into the pseudoaneurysm cavity through a microcatheter, which relies on its own fluidity to fill the aneurysm cavity; and (d) on re-examination of the angiography, the red arrow showed that pseudoaneurysm disappeared and the supplying artery was occluded.
Technical success was defined as complete embolization of the tumor body and its parent artery, with the disappearance of bleeding signs. Clinical success was defined as the gradual disappearance of symptoms such as bleeding after intervention and the stabilization of vital signs and hemoglobin. Embolism-related complications include pain at the embolic site, fever, ectopic embolism, liver, and kidney function damage. All patients were followed up for at least 3 months after surgery to monitor for any further bleeding.
RESULTS
A total of 31 patients were included in this study, including 19 males and 12 females, aged 41–84 years, with an average age of (f standard deviation) 62.9 ± 6.7 years. All patients showed symptoms of acute bleeding, including 14 cases of gastrointestinal bleeding: two cases after secondary intestinal surgery, four cases had a recent history of intracranial surgery, six cases had a history of ulcers, and two cases had unknown causes of bleeding; ten cases of hematuria: six cases were secondary to percutaneous kidney surgery, three cases had a history of kidney or bladder tumors, and one case had an unknown cause of hematuria; five cases of abdominal and pelvic bleeding: one case secondary to liver radiofrequency ablation, and four cases secondary to abdominal and pelvic infections; one case of bronchiectasis and hemoptysis; and one case of cervical cancer with vaginal bleeding. A total of 32 pseudoaneurysms were found in 31 patients undergoing angiography. One patient with hemoptysis found two pseudoaneurysms, one originating from the proximal left intercostal artery and one originating from the distal left bronchial artery. The diameter is 0.3~5.7 cm, with an average diameter of 1.4 ± 1.1 cm. All pseudoaneurysms were successfully embolized, of which 29 were treated with medical adhesive alone, and three were treated with coil assisted medical adhesive. After embolization, all pseudoaneurysms and their parent arteries were occluded, and no contrast agent entered the pseudoaneurysm cavity. The technical success rate was 100%. After 31 patients underwent endovascular medical adhesive embolization treatment, their vital signs remained stable and active bleeding stopped. Among them, 14 cases of gastrointestinal vascular pseudoaneurysm had negative bloody stools 3 days after embolization; eight cases of renal artery pseudoaneurysm and two cases of bladder artery pseudoaneurysm underwent embolization, and their urine color turned clear 24 h later; one case of hepatic artery pseudoaneurysm and four cases of splenic artery pseudoaneurysm showed a slow increase in hemoglobin and other indicators after embolization for 3 days; one case of bronchial artery and two intercostal artery pseudoaneurysms underwent embolization, and the symptoms of hemoptysis disappeared 2 days later; and one case of uterine artery pseudoaneurysm experienced disappearance of vaginal bleeding symptoms 24 h after embolization, with a clinical success rate of 100%. During postoperative follow-up, ten patients presented with post-embolism syndrome such as fever and pain at the embolic site, with an incidence rate of 32.2%. All patients did not experience severe ectopic embolism complications such as cerebral infarction, paraplegia, or organ ischemic necrosis. During the 3-month follow-up period, one patient with vaginal bleeding from a uterine artery pseudoaneurysm experienced vaginal bleeding again 2 months later. After undergoing interventional embolization again, vaginal bleeding stopped and no pseudoaneurysm reopened. A patient with hemoptysis caused by bronchial artery pseudoaneurysm experienced symptoms of hemoptysis again after 4 months. After undergoing interventional embolization again, hemoptysis stopped and no pseudoaneurysm reopened.
DISCUSSION
Clinically, aneurysms include true aneurysms and pseudoaneurysms. In the past, it was a rare but life-threatening disease, with an incidence of 0.1~2%.[8] In recent years, the incidence rate of peripheral pseudoaneurysms is on the rise. The increase of various pathogenic factors, including trauma, inflammatory infection, tumors, and various iatrogenic operations that can cause rupture of arterial walls and form pseudoaneurysms, lead the incidence of pseudoaneurysms become no longer so rare.[9,10] Among them, the development of iatrogenic procedures, including surgery, biopsy, vascular intubation, and various invasive examinations, such as choledochoscopy and nephroscope, is the primary factor for the increase of incidence rate of peripheral pseudoaneurysm.[11] Pseudoaneurysms show a higher risk of rupture than true aneurysms, with an untreated mortality rate of up to 100% once ruptured.[3,5,8] Therefore, once a pseudoaneurysm is discovered, it should be treated immediately.
The treatment of pseudoaneurysm includes surgical procedures and minimally invasive interventional therapy. With the development of endovascular technology, its advantages of precise efficacy, short hospital stay, and low mortality rate have led to percutaneous endovascular embolization gradually replacing surgery as the preferred treatment option for peripheral pseudoaneurysms.[8,12] Commonly used embolization materials include spring coils, gelatin sponges, and polyvinyl alcohol (PVA) particles. Recanalization different embolic agents have their own advantages and disadvantages.[2,5,10]
Coils are permanent solid embolic agents made of platinum. There are many soft fibrous hairs attached to it, which can promote the formation of blood clots.[3] Its advantage lies in having different sizes for embolizing blood vessels of different diameters. Second, there are various techniques available for direct sac packing or stent-assisted coiling techniques.[13] However, there are also many disadvantages in the application of coils in the embolization of peripheral pseudoaneurysms: (i) Peripheral pseudoaneurysms are mostly located in the 3rd and 4th grade branches of bleeding vessels, making it difficult for coils to perform super selective embolization. Non-selective embolization can increase the level of embolization and cause excessive organ function damage; (ii) secondly, coil embolization mainly relies on thrombus formation, which increases the possibility of pseudoaneurysm recanalization for pseudoaneurysms with rich blood flow perfusion or poor coagulation function in the body; and (iii) for the pseudoaneurysms which located in the 1st and 2nd grade branches of bleeding vessels, endovascular embolization with a coil may cause the pseudoaneurysm cavity to expand and increase the risk of rupture and bleeding.[3,14]
Gelatin sponge belongs to the mid-term embolic agent. Gelatin sponge particles or debris are mixed with iodine contrast agent to form gelatin sponge slurry, which is used to quickly block bleeding in a short period of time. Its advantage lies in the gradual absorption of gelatin sponge over time, avoiding permanent damage to embolic organs. Its main drawbacks are non-target embolism and vascular recanalization.[3,14]
PVA particles are granular embolic agents formed through production and screening, with sizes ranging from 100 μm to 1100 μm. Its mechanism of action is to block intravascular blood flow and induce inflammation in the vessel wall. PVA particles are usually used in combination with spring coils in the embolization of peripheral pseudoaneurysms. PVA particles are used to embolize distal blood vessels and block collateral blood supply. Its advantage lies in causing permanent embolism and allowing for repeated embolization of the same site. Its disadvantage lies in the blockage of the catheter caused by particle aggregation and the need to pay attention to the risks of particle reflux and non-target embolism during embolization.[14]
These materials have many limitations in the application of peripheral pseudoaneurysm embolization. Hence, a more ideal embolization material is needed to improve the success rate of peripheral pseudoaneurysm embolization and reduce the probability of pseudoaneurysm embolization recanalization.
The chemical name of medical adhesive in this research is α-N-butyl cyanoacrylate, used in surgical debridement and hernia repair. It is a denser permanent liquid embolic agent that rapidly polymerizes when exposed to trace amounts of anionic substances, such as human blood, body fluids, tissue fluids, or organic amines.[15] It tightly embeds and solidifies with the contacted tissue, forming a hard knot, and has good adhesion effect. Medical adhesive has the advantages of good imaging, adjustable coagulation time, and extremely low recanalization rate in the process of embolization treatment.[9] Therefore, this study applied medical adhesive endovascular embolization to treat 31 patients with peripheral pseudoaneurysm, to explore its clinical application value in the endovascular treatment of peripheral pseudoaneurysm.
The treatment principle for endovascular embolization of pseudoaneurysm is to completely and permanently block the blood supply to the pseudoaneurysm, while preserving the normal blood flow of other visceral blood supply arteries as much as possible. In this study, 31 patients with peripheral pseudoaneurysms were treated with medical adhesive to embolize a total of 32 pseudoaneurysms. Among them, 29 pseudoaneurysms were treated with medical adhesive alone, and three pseudoaneurysms were treated with coil assisted medical adhesive. Among them, two pseudoaneurysms were renal pseudoaneurysms, one was wide necked pseudoaneurysm, and one was complicated with renal vein fistula, embolize the outflow end of the carrier artery of a pseudoaneurysm with a spring coil, and then fill the pseudoaneurysm cavity with medical adhesive; another case was a pseudoaneurysm of the bladder artery. Due to the tortuous opening and stenosis of the parent artery, the microcatheter was unable to be super-selected. After the ipsilateral superior gluteal artery was protected with a spring coil, the pseudoaneurysm was embolized with 1:6 low concentration medical adhesive. After the embolization of 32 pseudoaneurysms, angiography was performed again. The pseudoaneurysm and its parent artery were occluded, and no contrast agent entered the tumor cavity. The technical success rate was 100%. The success rate of endovascular embolization therapy for visceral pseudoaneurysm in the previous studies was 84.2~100%, which is consistent with the results of this study.[10] The results of this study are consistent with them. After post-operative follow-up, all patients had stable vital signs and stopped active bleeding, with a clinical success rate of 100%. Xu et al.,[16] and Van Holsbeeck et al.,[17] used commonly used embolic agents such as spring coils, gelatin sponges, and PVA particles to embolize 17 cases and nine cases of peripheral pseudoaneurysms, respectively. The technical success rates were 94.1% and 100%, and the clinical success rates were 94.1% and 100%, respectively. The technical success rate of using medical adhesive plugs to plug peripheral pseudoaneurysms in this study is basically consistent. For some end stage peripheral pseudoaneurysms with small diameter of the parent artery, the microcatheter cannot be super-selected to the pseudoaneurysm cavity due to rupture and bleeding. The coil cannot fill the pseudoaneurysm cavity and completely block the blood flow of the pseudoaneurysm. The flowability of the medical adhesive effectively solves this problem. Choosing a low concentration medical adhesive with a ratio of 1:4 or 1:6 can slow down its aggregation rate, allowing it to flow to grade 3–4 vascular branches and better fill the pseudoaneurysm cavity. This can improve the technical success rate of endovascular embolization therapy for pseudoaneurysms to a certain extent. In the study of 20 cases of visceral pseudoaneurysms treated with coils by Parildar et al.,[18] two cases of visceral pseudoaneurysms were treated with medical adhesive due to the inability of microcatheters to be super-selective. After embolization, the patient immediately stopped bleeding. Park et al.,[19] used medical adhesive embolization to treat 26 patients with postpartum active bleeding, of which 15 showed uterine artery pseudoaneurysm. The technical and clinical success rates were 100% and 92.3%, respectively. Therefore, endovascular medical adhesive embolization is a very effective method for treating peripheral pseudoaneurysms.
All patients did not experience severe ectopic embolism complications such as cerebral infarction, paraplegia, or organ ischemic necrosis during follow-up after medical adhesive embolization. Only ten patients presented with post-embolism syndrome such as fever and pain at the embolic site, with an incidence rate of 32.2%, which is consistent with the 9–38% incidence of post-embolism syndrome in the previous studies. After symptomatic treatment, all patients improved.[11] In the studies of Song et al.,[20] and Borghese et al.,[21] on the treatment of visceral pseudoaneurysms with medical adhesive embolization, there were no serious complications such as ectopic embolization. Therefore, endovascular embolization with medical adhesive is a safe and effective method for treating peripheral pseudoaneurysms.
After vascular intervention embolization for peripheral pseudoaneurysm, as long as the embolization is complete, good therapeutic effects can be achieved, and the probability of recanalization and rupture bleeding is extremely low.
The selection of embolization materials is an important influencing factor for pseudoaneurysm recurrence. During the 3-month follow-up period in this study, one patient with vaginal bleeding caused by uterine artery pseudoaneurysm experienced vaginal bleeding again 2 months later, and the bleeding stopped after secondary interventional embolization; a patient with bronchial artery pseudoaneurysm and hemoptysis developed hemoptysis symptoms again after 4 months, and hemoptysis stopped after secondary interventional embolization. These two patients were not found to have re-canalized pseudoaneurysm after re-examination and angiography. In the study of 48 cases of visceral aneurysms and pseudoaneurysms treated with endovascular coil embolization by Tulsyan et al.,[8] one patient with hepatic artery pseudoaneurysm experienced pseudoaneurysm re-canalization 2 weeks after embolization. The reason was that the coil shifted into the pseudoaneurysm cavity, causing the pseudoaneurysm to expand. Therefore, the patient underwent secondary embolization.
CONCLUSION
Endovascular medical adhesive embolization is a safe and effective method for treating peripheral pseudoaneurysms, with high hemostatic efficiency and permanent occlusion of the pseudoaneurysm after embolization, which is worthy of clinical promotion and application.
Ethical approval
Since it is a retrospective study, the Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as the patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Interventional radiology in the diagnosis, management, and follow-up of pseudoaneurysms. Cardiovasc Intervent Radiol. 2009;32:2-18.
- [CrossRef] [PubMed] [Google Scholar]
- Interventional radiology in the management of visceral artery pseudoaneurysms: A review of techniques and embolic materials. Korean J Radiol. 2016;17:351-63.
- [CrossRef] [PubMed] [Google Scholar]
- Pseudoaneurysm: A review. Curr Treat Options Cardiovasc Med. 2008;10:173-83.
- [CrossRef] [PubMed] [Google Scholar]
- Review of visceral aneurysms and pseudoaneurysms. J Comput Assist Tomogr. 2015;39:1-6.
- [CrossRef] [Google Scholar]
- Transcatheter arterial embolization for massive hemobilia with N-butyl cyanoacrylate (NBCA) Glubran 2. Acta Radiol. 2022;63:360-7.
- [CrossRef] [PubMed] [Google Scholar]
- Transcatheter arterial embolization using n-butyl cyanoacrylate-Lipiodol mixture and metallic coils in a patient with biliary hemorrhage after removing a bile duct metallic stent: A case description. Quant Imaging Med Surg. 2022;12:4704-7.
- [CrossRef] [PubMed] [Google Scholar]
- The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg. 2007;45:276-83.
- [CrossRef] [PubMed] [Google Scholar]
- N-butyl cyanoacrylate embolization of a traumatic pseudoaneurysm and arteriovenous fistula of the middle meningeal artery. Radiol Case Rep. 2020;15:321-5.
- [CrossRef] [PubMed] [Google Scholar]
- Systematic review and single-center experience for endovascular management of visceral and renal artery aneurysms. J Vasc Interv Radiol. 2016;27:1630-41.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review and meta-analysis of the management of visceral artery aneurysms. J Vasc Surg. 2020;72:40S-45S.
- [CrossRef] [PubMed] [Google Scholar]
- The role of interventional radiology in the management of abdominal visceral artery aneurysms. Cardiovasc Intervent Radiol. 2012;35:234-43.
- [CrossRef] [PubMed] [Google Scholar]
- Application of interventional embolization in the treatment of iatrogenic pseudoaneurysms. Exp Ther Med. 2020;20:248.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular embolization: Review of currently available embolization agents. Curr Probl Diagn Radiol. 2014;43:35-53.
- [CrossRef] [PubMed] [Google Scholar]
- Nidal embolization of brain arteriovenous malformations: Rates of cure, partial embolization, and clinical outcome. J Neurosurg. 2012;117:65-77.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical efficacy of coil embolization in treating pseudoaneurysm post-Whipple operation. Exp Ther Med. 2020;20:37.
- [CrossRef] [PubMed] [Google Scholar]
- Coil embolization of true, common and proper, hepatic artery aneurysms: Technique, safety and outcome. Cardiovasc Intervent Radiol. 2023;46:480-7.
- [CrossRef] [PubMed] [Google Scholar]
- Embolization of visceral pseudoaneurysms with platinum coils and N-butyl cyanoacrylate. Abdom Imaging. 2003;28:36-40.
- [CrossRef] [PubMed] [Google Scholar]
- Postpartum hemorrhage from extravasation or pseudoaneurysm: Efficacy of transcatheter arterial embolization using N-butyl cyanoacrylate and comparison with gelatin sponge particle. J Vasc Interv Radiol. 2015;26:154-61.
- [CrossRef] [PubMed] [Google Scholar]
- Transcatheter N-butyl cyanoacrylate embolization of pseudoaneurysms. J Vasc Interv Radiol. 2010;21:1508-11.
- [CrossRef] [PubMed] [Google Scholar]
- The minimally invasive treatment of visceral artery pseudoaneurysms: A retrospective observational single centre cohort study on glue embolization. Vasc Endovascular Surg. 2021;55:831-7.
- [CrossRef] [PubMed] [Google Scholar]






