Translate this page into:
Percutaneous Transhepatic Cholangioscopy and Stone Extraction in a Patient with Recurrent Cholangitis Following Liver Trauma

*Corresponding author: Lee K. Rousslang, Department of Radiology, Tripler Army Medical Center, Hawaii, USA. lee.k.rousslang.civ@mail.mil
-
Received: ,
Accepted: ,
How to cite this article: Rousslang LK, Faruque O, Kozacek K, Meadows JM. Percutaneous Transhepatic Cholangioscopy and Stone Extraction in a Patient with Recurrent Cholangitis Following Liver Trauma. J Clin Imaging Sci 2021;11:11.
Abstract
Percutaneous transhepatic cholangioscopy (PTCS) is a safe and effective treatment for obstructive biliary stones, when endoscopic retrograde cholangiopancreatography (ERCP) is unsuccessful or unavailable. Once percutaneous access is gained into the biliary tree by an interventional radiologist, the biliary ducts can be directly visualized and any biliary stones can be managed with lithotripsy, mechanical fragmentation, and/or percutaneous extraction. We report a case of a 45-year-old man who sustained a traumatic liver laceration and associated bile duct injury, complicated by bile duct ectasia and intrahepatic biliary stone formation. Despite undergoing a cholecystectomy, multiple ERCPs, and percutaneous transhepatic cholangiogram with drain placement, the underlying problem was not corrected leading to recurrent bouts of gallstone pancreatitis and cholangitis. He was ultimately referred to an interventional radiologist who extracted the impacted intrahepatic biliary stones that were thought to be causing his recurrent infections through cholangioscopy. This is the first case of PTCS with biliary stone extraction in the setting of recurrent biliary obstruction and cholangitis due to traumatic bile duct injury.
Keywords
Hepatolithiasis
Recurrent cholangitis
Biliary endoscopy
Biliary lithotripsy
Choledochoscopy
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is the gold standard treatment for choledocholithiasis and other bile duct pathology, and is used in approximately 90% of such cases.[1] In the hands of an experienced endoscopist, the technical success rate is reported to be between 90% and 95%.[2] Situations where ERCP may not be feasible include obstructing bile duct tumors and patients with altered surgical anatomy such as gastric bypass patients. In these situations, alternative methods of accessing and treating biliary tree pathology are necessary in select patients.[3]
Percutaneous transhepatic cholangioscopy (PTCS) is one approach to manage such patients, typically performed by an interventional radiologist. PTCS has been performed for decades and is a standard procedure for interventional radiologists. Most of the evidence supporting the use of PTCS and lithotripsy is limited to case series and single-center studies.[4-6]
After gaining percutaneous access into the biliary tree, an endoscope can be inserted into the liver to visualize bile ducts through the existing percutaneous tract. If stones are identified, they can be managed through lithotripsy (laser, electrohydraulic, or mechanical), percutaneous extraction, or balloon sweeping of stones into the duodenum.[4] These techniques have been described in the literature as safe and effective treatment options for patients with complex biliary stones not amenable to ERCP.[7]
In refractory cases, hepatic resection has been described for the treatment of hepatolithiasis and may offer the best long-term results, but is much more invasive than ERCP and PTCS, and may only be a viable option if the stones are localized to one segment or lobe.[8] Bilateral partial hepatectomy has also been described, but remains investigational.[9]
CASE REPORT
A 45-year-old man was transferred to our facility for the management of recurrent cholangitis and pancreatitis due to impacted intrahepatic biliary stones. Approximately 15 years prior, the patient sustained a Grade III liver laceration while serving in combat for the US military and was managed nonoperatively.
Approximately 6 years after the initial liver injury, the patient developed right upper quadrant (RUQ) abdominal pain, nausea, and vomiting. A CT of the abdomen revealed intrahepatic ductal dilatation with intrahepatic bile stones in the right hepatic lobe, isolated to Couinaud segment 7 [Figure 1]. He was admitted for ascending cholangitis and gallstone pancreatitis, and underwent an open cholecystectomy with bile duct exploration and t-tube placement.
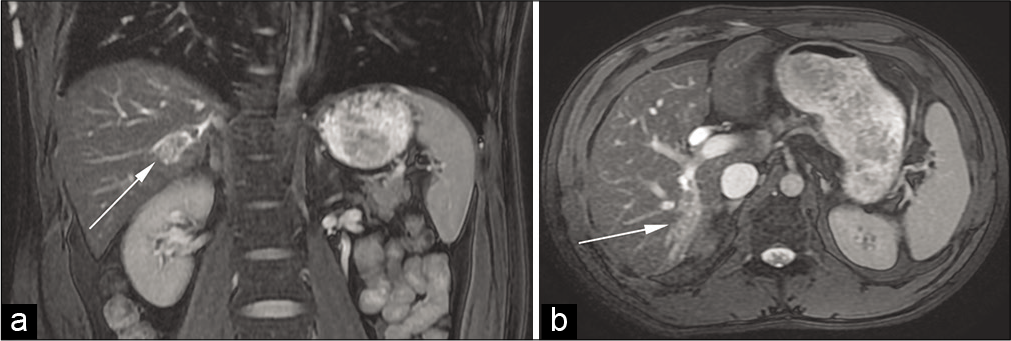
- A 37-year-old man with a remote history of a liver laceration presented with the right upper quadrant abdominal pain, nausea, and vomiting. Coronal (a) and axial (b) fluid-sensitive MR images demonstrate bile duct dilatation in the right lobe of the liver (arrows).
His recovery was uneventful until 2 years later, when he presented with RUQ abdominal pain and nausea, and was found to have choledocholithiasis and intrahepatic bile duct stones on CT. He was treated with an ERCP with stone extraction and sphincterotomy that cleared the common bile duct (CBD) stones. There was no report of intrahepatic stones identified or treated. A post-procedural magnetic resonance cholangiopancreatography was performed and reported no obvious obstructive stones remaining in the CBD.
Four years later, he presented again with RUQ pain and was diagnosed with recurrent ascending cholangitis and gallstone pancreatitis, and underwent repeat ERCP with stone extraction. Symptoms recurred 2 years later, and the patient underwent percutaneous transhepatic biliary drain (PTBD) placement by an interventional radiologist. Attempts to extract the stones at that time through percutaneous access using fluoroscopic guidance were unsuccessful.
Follow-up MRI of the abdomen after PTBD placement demonstrated diffuse biliary duct dilation with recurrent intrahepatic stone formation in the right posterior liver and in the CBD, complicated by acute pancreatitis [Figure 2]. He was transferred to our tertiary care center for further evaluation by gastroenterology and interventional radiology (IR).
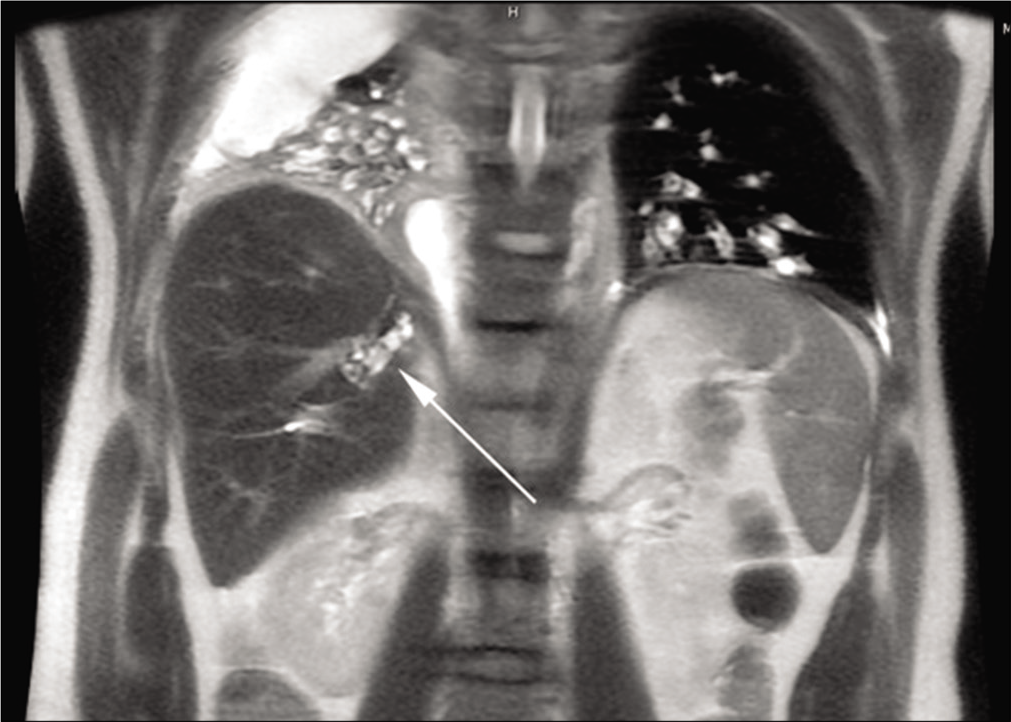
- A 45-year-old man with recurrent right upper quadrant abdominal pain. Coronal magnetic resonance cholangiopancreatography demonstrates retained intrahepatic stones (arrow) in the right posterior liver.
Repeat ERCPs were first attempted that were successful in removing multiple stones from the CBD through mechanical lithotripsy and basket retrieval [Figure 3]. However, the intrahepatic stones were not identified at endoscopy. After a multidisciplinary discussion, the patient was referred to IR for percutaneous transhepatic choledochoscopy. Following the induction of general anesthesia, a cholangiogram was performed through the patient’s existing percutaneous access demonstrating an enlarged biliary duct in segment 7 containing multiple filling defects consistent with impacted stones. This duct was not accessible through ERCP due to its peripheral location, variant biliary anatomy, and presence of the indwelling biliary drain.
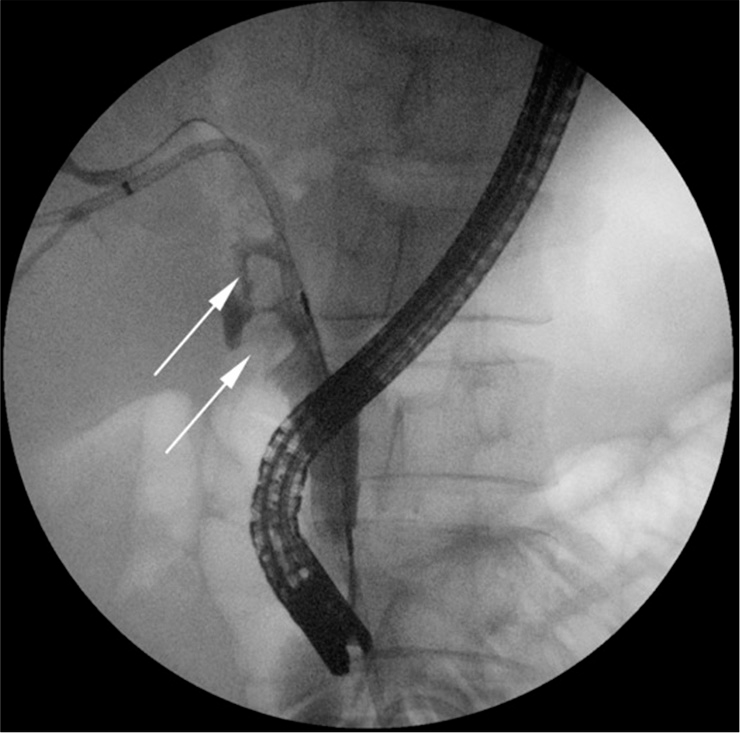
- A 45-year-old man with recurrent ascending cholangitis. Endoscopic retrograde cholangiopancreatography demonstrates multiple filling defects in the common bile duct (arrows), but the isolated segment of intrahepatic stones could not be localized.
A 10 French peel-away sheath was placed through the tract into the liver, without need for dilation, through which a 9.5 French LithoVue Single-use Digital Flexible Ureteroscope (Boston Scientific, Marlborough, MA) with a two-way deflection scope was advanced into the intrahepatic biliary tree without insufflation [Figure 4]. The abnormal branch in segment 7 was quickly identified containing numerous stones. A 2.4 French Zero Tip Nitinol Retrieval Basket (Boston Scientific, Marlborough, MA) was used to extract the stones percutaneously [Figure 5]. Several additional stone fragments were swept into the duodenum with a compliant balloon catheter. Stones larger than the 2.4 French basket were not encountered. If present, they would have been fragmented using laser lithotripsy. If the basket was stuck with a stone, the stone would have been abandoned and left in the biliary system, with the biliary drain left in place. At the completion of the procedure, an internal-external biliary drain was left in place. Only a single session was performed. The patient was admitted to the hospital post-operatively, where his cholangitis resolved on broad-spectrum antibiotics, before being discharged home on post-operative day 8 with no further antibiotics as an outpatient.
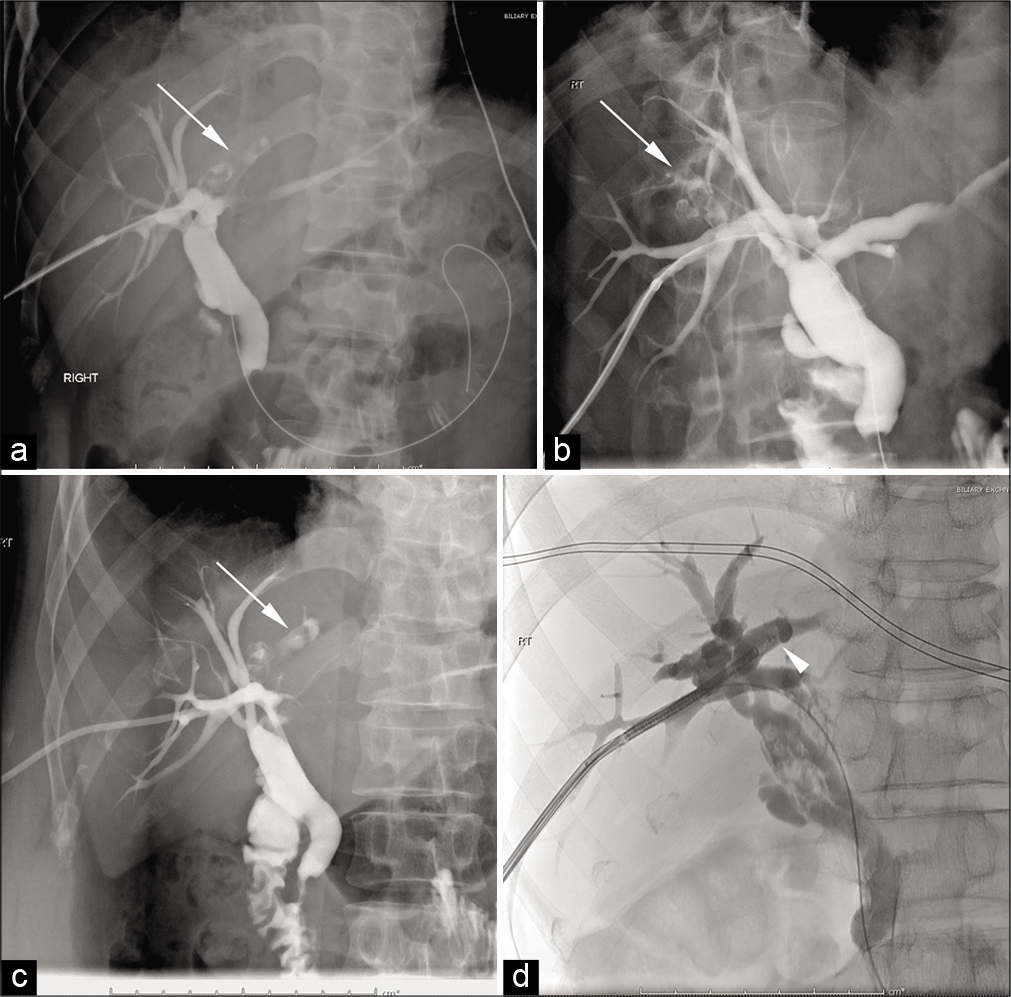
- A 45-year-old man with recurrent ascending cholangitis secondary to intrahepatic biliary stones that were not identified at endoscopic retrograde cholangiopancreatography. Intraprocedural fluoroscopic cholangiogram (a-d) demonstrates intrahepatic biliary stones (arrows). A flexible ureteroscope (arrowhead in d) is seen entering into the right hepatic duct.
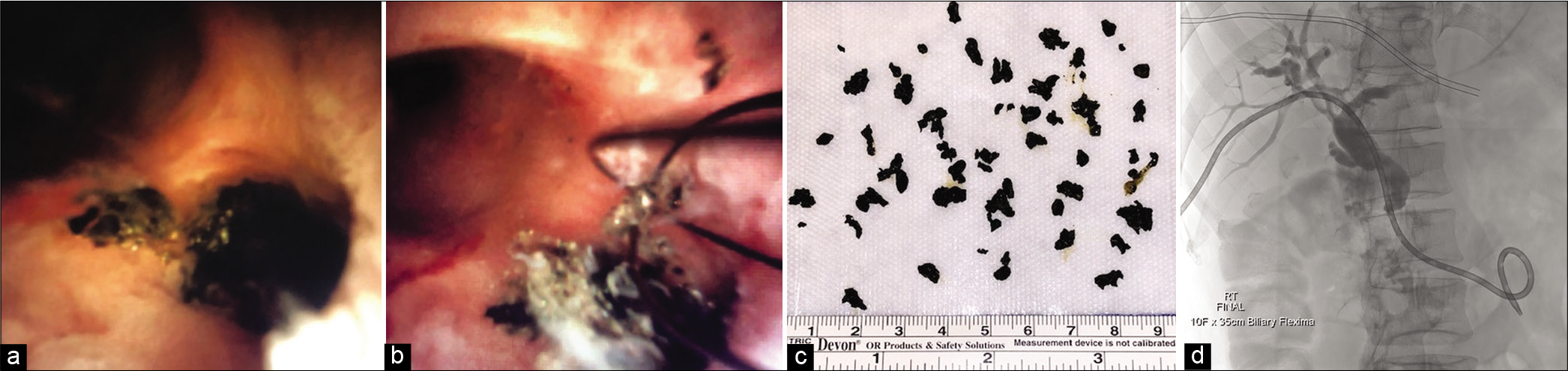
- A 45-year-old man with recurrent ascending cholangitis secondary to intrahepatic biliary stones that were not identified at endoscopic retrograde cholangiopancreatography. Endoscopic images reveal the impacted biliary stones (a), with subsequent percutaneous extraction of the stones (b and c). Percutaneous cholangiogram after stone retrieval (d) demonstrates clearing of the filling defects.
The percutaneous biliary drain was removed 6 months later. The patient has remained asymptomatic at the time of this manuscript nearly 2 years later.
DISCUSSION
PTCS is well recognized as a safe and effective treatment for obstructing biliary stones that are not amenable to ERCP or surgical resection and is appealing because of the widespread availability of ureteroscopes in IR services. The combination of these two techniques provides an excellent alternative to traditional treatment modalities in select cases. Treatment success is defined as the clearance of all intraductal stones, with reported success rates for PTCS between 76.8% and 97% in a number of case series.[10-13] Stone recurrence is reported at 15.8–28%,[14,15] with one case series reporting a recurrence rate of 40% after 10-year follow-up.[10]
Complication rates of PTCS have been reported in the literature as approximately 4–8%.[13,16] As noted by Ponchon et al., mechanical fragmentation of the bile stones with a choledochoscope may result in lower complication rates then electrohydraulic or shock wave lithotripsy because it does not expose the bile duct wall to potentially harmful trauma or shock waves.[4]
CONCLUSION
PTCS with stone retrieval is a safe and effective method for evaluating the biliary tree and extracting obstructing intrahepatic biliary stones. For persistent, symptomatic, focal, high intrahepatic stone disease in an anatomically complex patient, ERCP may be inadequate and either PTCS or segmental liver resection should be considered.
Acknowledgements
The views expressed in this manuscript are those of the authors, and do not reflect the official policy or position of the Department of the Army, Department of Defense, or the United States Government. The authors have no financial, personal, or other vested interests in the information contained within this document.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Endoscopic and percutaneous treatment of difficult bile duct stones. Endoscopy. 2003;35:S31-4.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of endoscopic sphincterotomy and their prevention. N Engl J Med. 1996;335:961.
- [CrossRef] [PubMed] [Google Scholar]
- The management of treatment-resistant biliary calculi using percutaneous endourologic techniques. Can J Surg. 2009;52:407-12.
- [Google Scholar]
- Methods, indications and results of percutaneous choledochoscopy: A series of 161 procedures. Ann Surg. 1996;1:26-36.
- [CrossRef] [PubMed] [Google Scholar]
- SpyGlass percutaneous transhepatic cholangioscopy-guided lithotripsy of a large intrahepatic stone. Endoscopy. 2017;49:E292-3.
- [CrossRef] [PubMed] [Google Scholar]
- Cholangioscopy-guided electrohydraulic lithotripsy of large bile duct stones through a percutaneous access device. Endoscopy. 2018;50:E111-2.
- [CrossRef] [PubMed] [Google Scholar]
- Updated guideline on the management of common bile duct stones (CBDS) Gut. 2017;66:765-82.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of treatments for hepatolithiasis: Hepatic resection versus cholangioscopic lithotomy. J Am Coll Surg. 1999;189:177-82.
- [CrossRef] [Google Scholar]
- Hepatectomy for bilateral primary hepatolithiasis: A cohort study. Ann Surg. 2010;251:84.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous trans-hepatic cholangioscopic lithotomy for hepatolithiasis: long-term results. Gastrointest Endosc. 1995;42:1-5.
- [CrossRef] [Google Scholar]
- Percutaneous transhepatic choledochoscopic removal of intrahepatic stones. Br J Surg. 2003;90:1409-15.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous choledochoscopic biliary tract stone removal: Experience in 645 consecutive patients. Eur J Radiol. 1993;17:184-90.
- [CrossRef] [Google Scholar]
- Percutaneous biliary drainage: Complications of 118 consecutive catheterizations. Radiology. 1986;158:199-202.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of hepatolithiasis: Improvement of result by a systematic approach. Surgery. 1991;109:474-80.
- [Google Scholar]
- Percutaneous transhepatic lithotripsy using a choledochoscope: Long-term follow-up in I4 patients. AJR Am J Roentgenol. 1998;171:1387-9.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of percutaneous transhepatic cholangioscopy-related complications and the risk factors for those complications. Endoscopy. 2007;39:731-6.
- [CrossRef] [PubMed] [Google Scholar]






