Translate this page into:
Satisfaction of Search: Recurrent Wilms Tumor Mimicking Chest Port Granuloma on Chest Film

*Corresponding author: Nikki D. Rousslang, Department of Medical Education, University of Hawaii John A. Burns School of Medicine, 651 Ilalo Street, Honolulu, Hawaii 96813. nikkidr@hawaii.edu
-
Received: ,
Accepted: ,
How to cite this article: Rousslang ND, Rooks E, Delaney K. Satisfaction of search: Recurrent Wilms tumor mimicking chest port granuloma on chest film. J Clin Imaging Sci 2020;10:13.
Abstract
Wilms tumor (nephroblastoma) is the most common renal malignancy of childhood and typically presents as a painless abdominal mass. The high success rates of surgery and chemotherapy make recurrence of Wilms tumor uncommon. We report the case of a 5-year-old girl who underwent radical nephrectomy and chemotherapy for a Wilms tumor, but suffered a relapse of the tumor to the lung. The metastasis was initially detected as a density on chest radiograph that was, coincidentally, in the same location as a recently explanted chest port. The diagnosis of recurrent malignancy was thus obscured by the patient’s history as well as a correlating physical examination finding of a palpable mass at the site of the previously placed chest port. Moreover, the mass was not seen on lateral view, all of which suggested an alternative diagnosis of granulation tissue versus seroma rather than recurrent Wilms tumor. A high degree of clinical suspicion was necessary on the part of the clinician and radiologist to diagnose the relapse.
Keywords
Nephroblastoma
Metastatic Wilms tumor
Satisfaction of search
INTRODUCTION
Wilms tumor has an incidence of approximately 500 cases/year and comprises approximately 5% of childhood malignancies.[1] Stage II Wilms tumor is identified by the presence of favorable histology with extrarenal invasion and carries an excellent prognosis with an 8-year event-free survival of 85%.[2] We report the case of a 5-year-old girl who was diagnosed with a Stage II Wilms tumor, who had successful surgical resection and completed chemotherapy, but suffered a relapse of the tumor to the lung. The diagnosis was complicated by other aspects of the history and physical examination, making the recurrence a significant diagnostic challenge to the radiologist and clinician. This case serves as a reminder of the importance of avoiding satisfaction of search and potential report bias.
CASE REPORT
A previously healthy 4-year-old girl presented to the emergency department with a painless, right-sided abdominal mass that had been enlarging for the past 4 weeks. The patient had no associated symptoms. On examination, there was a large, firm, protruding, non-tender abdominal mass on the right side, extending from midline to flank laterally, and to the level of the umbilicus inferiorly.
Ultrasound of the abdomen revealed a large cystic and solid mass with fluid-fluid levels in the right renal fossa, concerning for Wilms tumor, and a follow-up CT demonstrated a heterogeneously enhancing mass, also consistent with a Wilms tumor [Figure 1]. Radical nephrectomy was performed and revealed extrarenal invasion. Subsequent pathology demonstrated favorable histology and negative margins. The patient then had a chest port placed [Figure 2] and completed standard treatment for Stage II Wilms tumor with 19 weeks of chemotherapy consisting of intravenous vincristine and actinomycin D.
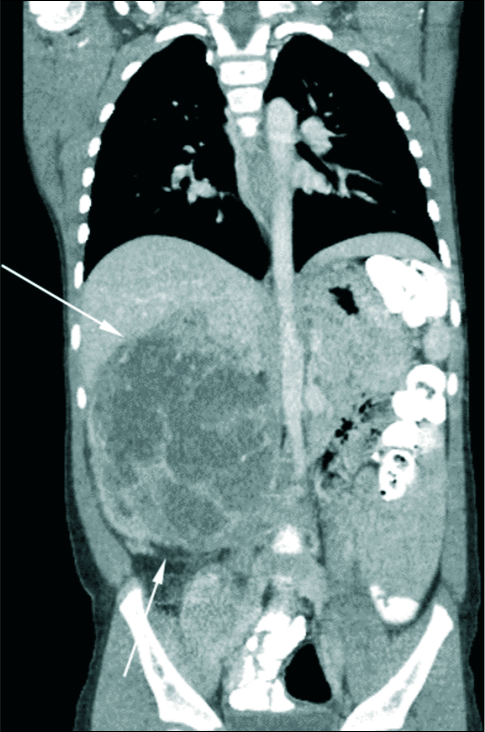
- 4-year-old girl presenting for an asymptomatic abdominal mass. Contrast enhanced coronal computed tomography demonstrates a large, heterogeneously enhancing lesion, with significant mass effect on nearby structures in the abdomen, consistent with a Wilms tumor.
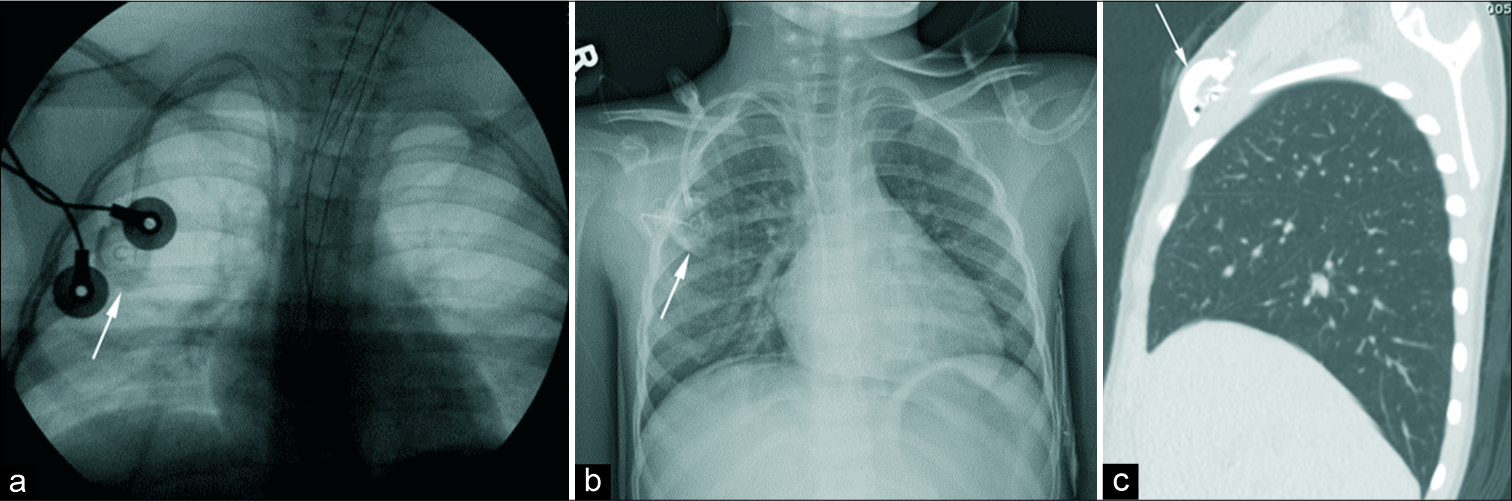
- 4-year-old girl with a history of Wilms tumor status-post excision has flouroscopic imaging (a) and an anteroposterior chest radiograph (b) demonstrating placement of a right-sided chest port. A sagittal computed tomography (c) redemonstrates the placement of the chest port.
Approximately 4 months after completion of therapy, the patient presented to the clinic for a routine surveillance chest radiograph, which showed a 2.7 × 2.3 cm round, radiopaque, right upper lobe density seen in the right upper thorax on the anteroposterior view, not visualized on the lateral view [Figure 3]. The differential diagnosis included a seroma or granuloma that formed following removal of her chest port, a superficial skin lesion, an artifact from the patient’s clothing, or less likely since the mass was not visualized on the lateral view, metastatic disease.
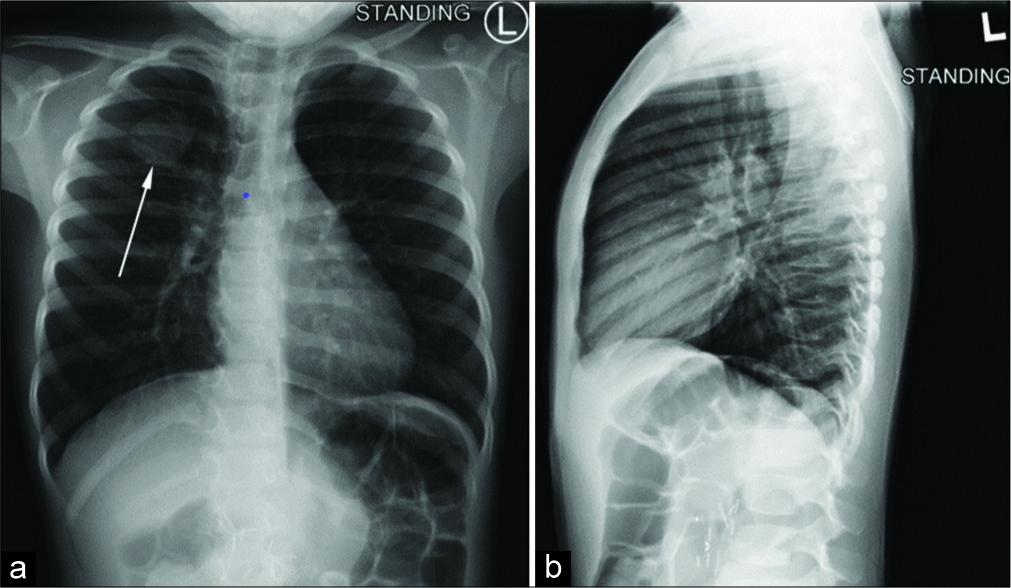
- 5-year-old girl presenting for routine surveillance imaging nine months after surgical resection of a Wilms tumor, followed by chemotherapy. (a) Anterior-posterior plain chest radiography demonstrates an opacity in the right upper region of the chest. (b) The opacity is not present in the sagittal view. The opacity was accompanied by a palpable mass over the right upper chest, and was thought to be scar tissue from a recently explanted chest port over the area.
The radiologist also recommended a physical examination of the patient’s right upper chest and commented that if the mass was superficial and palpable, a sonographic evaluation could be considered.
Physical examination was notable for scar tissue from the previous chest port, and based on the previous radiologist recommendations, an ultrasound was ordered revealing a hypoechoic, anterior subcutaneous chest wall mass measuring 1.5 × 0.5 × 1.2 cm that likely represented scar granuloma formation beneath previously removed chest port [Figure 4]. After great debate, because the ultrasound lesion did not correlate with the size of the mass on chest radiograph, a limited chest CT was recommended.
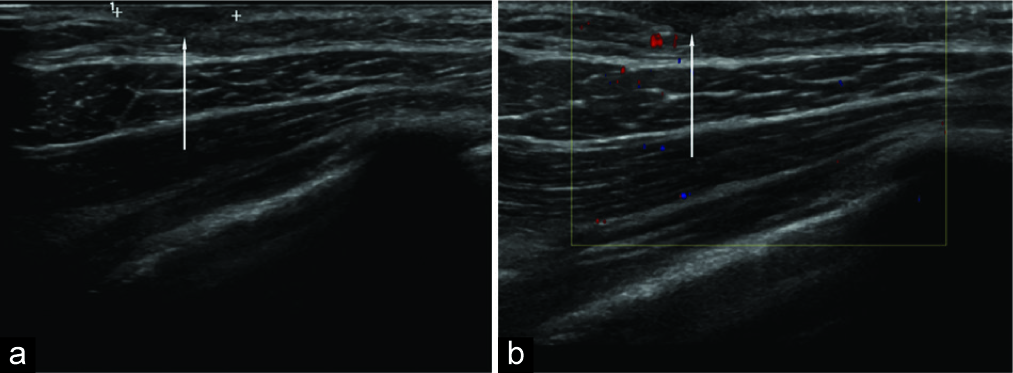
- 5-year-old girl with a history of Wilms tumor status-post excision and chemotherapy presents for follow up of an opacity seen on chest radiograph. Superficial axial sonography of the right upper chest wall demonstrates a hypoechoic, subcutaneous mass. The size of the mass, however, did not correlate to the opacity on the surveillance chest radiograph.
The corresponding chest CT revealed a 2.5 cm right upper lobe mass abutting the right posterior chest wall, concerning for relapse of Wilms tumor with hilar adenopathy [Figure 5].
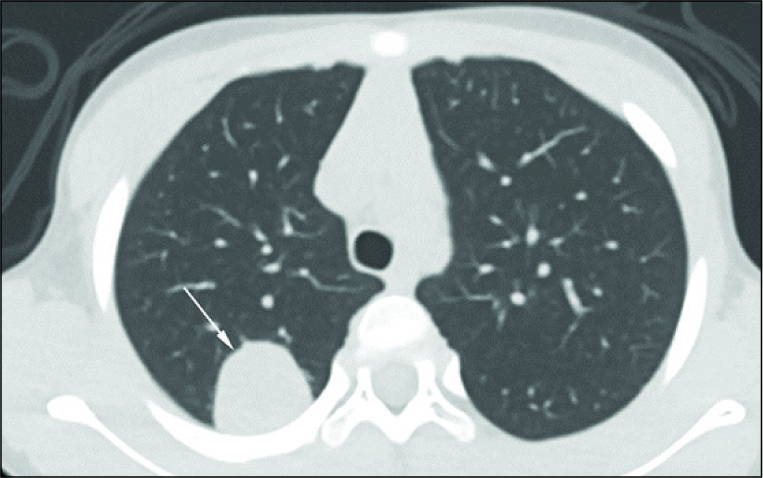
- 5-year-old girl with a history of Wilms tumor, and mass seen on surveillance chest radiograph. Contrast enhanced axial CT of the chest of demonstrates an enhancing lesion in the right posterior lung, consistent with metastatic Wilms tumor.
A CT-guided lung biopsy was performed, and corresponding tissue pathology demonstrated a poorly differentiated immature neoplasm, consistent with metastatic Wilms tumor. Pediatric oncology recommended therapy with whole lung radiation and intravenous chemotherapy with vincristine, doxorubicin, etoposide, and cyclophosphamide, which the patient is currently receiving.
DISCUSSION
Wilms tumor is the most common renal malignancy of children with approximately 500 cases diagnosed annually, at a median age of 38 months.[1,3] Histology is either favorable or unfavorable, with unfavorable being defined by the presence of anaplasia, characterized by multipolar polypoid mitotic figures, and marked nuclear enlargement with hyperchromasia.[4] Anaplasia is the most important predictor of adverse outcomes (relapse and death) in Wilms tumor, as evidenced by 90% 2-year survival with cases of favorable histology and 54% survival with unfavorable histology.[5] The disease stage is another important prognostic indicator and is shown in Table 1. Our patient had extracapsular invasion indicative of Stage II tumor.
| Stage description |
|---|
|
CT of Wilms tumors typically demonstrates a spherical mass that is iso- or hypoattenuating compared to the surrounding renal parenchyma, and hyperattenuating compared to lung parenchyma.[6,7] Because Wilms tumor is usually large at presentation (11 cm on average), determining if there is an invasion of adjacent structures can be difficult.[6,7] On MRI, Wilms tumor is typically heterogeneous and T1 iso- or hypointense with decreased enhancement post-gadolinium, whereas T2 imaging is variable but typically iso- or hyperintense.[6,7]
Although Stage II Wilms tumor with favorable histology has an 8-year event-free survival rate of 85.0%, this case demonstrates the importance of following up all pulmonary nodules found on chest radiographs in children.[2] In this case, there was an alternative explanation for the opacity seen on chest radiograph (the palpable granulation tissue underlying the scar from the recently removed chest port). Given the proximity in time from the chest port removal and the finding on chest radiograph, it would have been reasonable for the radiologist and clinician to attribute the mass to the palpable chest port granuloma. High clinical suspicion of recurrence, however, prompted an ultrasound evaluation of the region that determined that the mass was not attributable to scar granuloma from the chest port. CT revealed metastatic disease, confirmed by CT-guided lung biopsy. Thanks to the early detection of the recurrence, the patient is now undergoing treatment with chemotherapy and radiation, with an overall 4-year event-free survival rate of 67.8% based on Wilms tumor relapse to the lungs only, and previous treatment with vincristine and actinomycin D.[8]
CONCLUSION
Recurrent Wilms tumor is an uncommon entity, and if obscured by history and physical examination, can present a significant diagnostic challenge to the clinician and radiologist. This case serves as a reminder of the importance of following up on all pulmonary nodules seen on pediatric chest radiographs, to avoid potential satisfaction of search and report bias.
Acknowledgments
The views expressed in this manuscript are those of the authors and do not reflect the official policy or position of the Department of the Army, Department of Defense, or the United States Government. The authors have no financial, personal, or other vested interests in the information contained within this document.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Epidemiology of Wilms tumor. Med Pediatr Oncol. 1993;21:172-81.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of patients with Stage II/ favorable histology Wilms tumor with and without local tumor spill: A report from the national Wilms tumor study group. Pediatr Blood Cancer. 2014;61:134-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anaplasia in unilateral Wilms' tumor: A report from the national Wilms' tumor study pathology center. Hum Pathol. 1988;19:1199-209.
- [CrossRef] [Google Scholar]
- The treatment of Wilms' tumor: Results of the second national Wilms' tumor study. Cancer. 1981;47:2302-11.
- [CrossRef] [Google Scholar]
- Urogenital tumours in childhood. Cancer Imaging. 2011;11(Spec No A):S48-64.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric renal masses: Wilms tumor and beyond. Radiographics. 2000;20:1585-603.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of Wilms tumor relapsing after initial treatment with vincristine and actinomycin D: A report from the national Wilms tumor study group. Pediatr Blood Cancer. 2007;48:493-9.
- [CrossRef] [PubMed] [Google Scholar]






