Translate this page into:
Percutaneous CT-Guided Ablation in the Hepatic Dome: Artificially Induced Pneumothorax for Safe Transpleural Access
Address for correspondence: Dr. Leonardo Guedes Moreira Valle, Department of Interventional Radiology, Hospital Israelita Albert Einstein, Albert Einstein Avenue, 627/701, São Paulo, Brazil. E-mail: leogmv@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Ablative therapies have become a great alternative to surgical treatment of hepatic nodules. Some technical difficulties may negatively influence the effectiveness of this therapy, such as lesions located near the diaphragm. The transthoracic approach is commonly used to access these lesions. However, it is associated with an increased risk of complications, such as pneumothorax, hemothorax, alveolar bleeding, and others. We report a case of a radiofrequency ablation of a lesion in the hepatic dome, where an artificially induced pneumothorax was performed to guarantee a safe and effective access. The air was easily injected by a spinal needle and later aspirated by a single-lumen catheter. Induced pneumothorax shoud be considered in ablation of hepatic dome lesions, mainly when the transhepatic access is not appropriate.
Keywords
Ablation
artificially induced pneumothorax
dome
hepatocellular carcinoma
induced
liver
pneumothorax
radiofrequency ablation
transpleural access

INTRODUCTION
Ablative therapies have become a great alternative to surgical treatment of hepatic nodules. The indication of a minimally invasive therapy for a liver tumor lies in several criteria, highlighting the clinical condition of the patient, the number and size of nodules, and location of the lesions. In relation to this last point, some technical difficulties may negatively influence the effectiveness of this therapy, such as lesions located close to main vessels or biliary ducts, as well as lesions located in the liver periphery, mainly near the diaphragm.
Preferential access to just diaphragmatic lesions is the transhepatic approach. In their absence, transpulmonary access is an alternative. However, crossing the lung base and invasion of the pleural cavity are associated with an increased risk of complications, such as pneumothorax, hemothorax, alveolar bleeding, hemoptysis, tumor seeding, and severe postoperative pain.[1]
We report a case of radiofrequency ablation (RFA) of a lesion in the hepatic dome using an artificially induced pneumothorax to guarantee a safe and effective access.
CASE REPORT
The institutional review board's approval was not required for the present case report. A 60-year-old man presented with a hepatocellular nodule measuring 2.0 cm in the superior portion of segment VIII [Figure 1a]. Due to difficulty of the transhepatic access and knowing the potential risks of transpulmonary access, it was decided to perform an artificially induced pneumothorax.

- 60-year-old man presenting with liver tumor in the hepatic dome underwent MRI/CT of abdomen. (a) Axial MRI scan demonstrates a hepatocellular carcinoma nodule (white arrow) in the hepatic dome. (b) Preinterventional CT image shows the same nodule (white arrow) after contrast media injection.
The procedure was performed under general anesthesia and intercostal block with 1% ropivacaine hydrochloride. The patient was positioned in right oblique decubitus. A dynamic CT was obtained for identification of the target lesion and access planning [Figure 1b]. Then, a 22G spinal needle (Spinocan, B. Braun; Melsungen, Germany) was introduced to the right pleural cavity guided by ultrasound and CT [Figure 2a and b]. Initially, 100 cc of air was injected through a compact sterilized filter (Humid-Vent; Louis Gibeck AB, Upplands Vasby, Sweden), intending to separate the visceral pleura. After that, a 14G × 20 cm single-lumen catheter (Arrow international INC, Teleflex Incorporated, Reading, PA, USA) was introduced by Seldinger technique [Figure 2c]. Another 600 cc of air was injected under continuous clinical monitoring and repeated CT scans. The artificial pneumothorax promoted separation of the lung parenchyma, allowing a transpleural access guided by CT [Figure 2d]. The RFA was performed by a single probe ACTC 2520 (Covidien Ltd., Dublin, Ireland). Upon completion of the ablation, the pneumothorax did not respond completely to aspiration by the single-lumen catheter, so it was decided to insert a 10-F Wayne chest tube connected to a Heimlich valve (Cook, Inc, Bloomington, IN, USA) in the right pleural cavity. The patient was discharged from the hospital the next morning with the chest tube placed, without symptoms. Two days later, he returned and the chest tube was removed successfully.
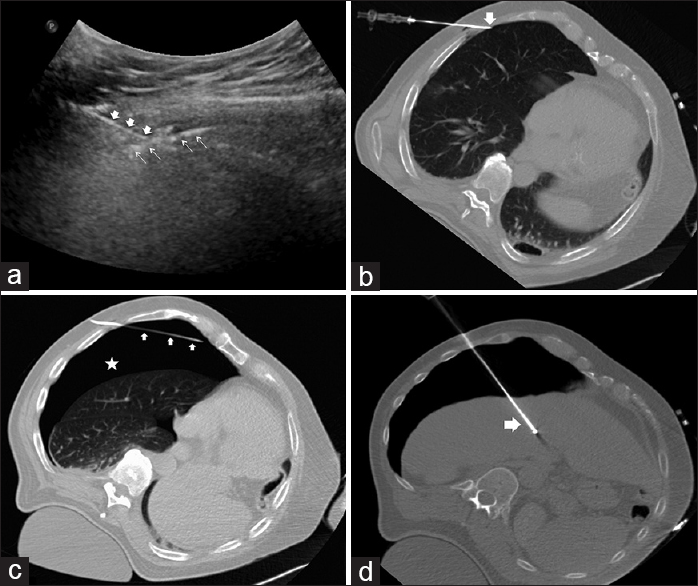
- 60-year-old man presenting with a hepatocellular carcinoma in the hepatic dome. (a) Ultrasound image shows a 22G spinal needle (white solid arrows) crossing the parietal pleura (white thin arrows). (b) CT image confirms the needle position (white solid arrow) within the pleural space. (c) A single-lumen catheter (white solid arrows) was placed in the right pleural cavity, allowing large amount of air injection (white star). (d) Subsequently, a radiofrequency probe (white solid arrow) was introduced into the middle of the lesion to be treated, through a transpleural access.
Control CT image immediately after the procedure did not show complications. The patient did not complain about pain for the next 24 h, and the drain was removed before hospital discharge. Follow-up MRI 2 months later demonstrated complete necrosis of the treated lesion [Figure 3].

- 60-year-old man presenting with a hepatocellular carcinoma in the hepatic dome underwent percutaneous radiofrequency ablation. Follow-up (a) axial and (b) coronal MRI scans 2 months after the procedure demonstrated complete necrosis of the lesion (white solid arrows).
DISCUSSION
Ablation of liver tumor is generally guided by ultrasonography (US) because of its advantages such as real-time imaging and absence of ionizing radiation, though for lesions in the hepatic dome, bowel interposition or pneumothorax could complicate needle visualization. Therefore, CT is an excellent method for guidance, with great visualization of the lesion and adjacent organs along the proposed route. The CT-guided transpulmonary approach proved to be effective, however, with high incidence of complications such as major lung bleeding or pleural dissemination.[123]
To transpose the access difficulties, other techniques had been described, such as induction of saline solution[3] or pneumothorax.[1] Injection of liquid or air in the pleural cavity decreases the incidence of complications because there is no damage to visceral pleura and lung parenchyma. Despite the fact that intrathoracic saline solution can grant a great window for US guidance, ionic agents act as electrical conductor and may cause distant damages in non-target organs.[14] Thus, a nonionic agent such as 5% glucose solution is more appropriate. An artificially induced pneumothorax, in turn, does not act as an electrical conductor or suffer from heat sink effect. In the present case, we demonstrated a safe and efficient RFA in the hepatic dome, performed according to the procedure outlined by de Baère et al.[1] Other authors have also shown its utility for lung and kidney ablations.[56] For such applications, the air could be easily injected as well as aspirated by a spinal needle or catheter.
Percutaneous RFA of hepatocellular carcinoma has shown low complications rates, ranging from 0.9% to 5.0%. The most common complications are peritoneal hemorrhage, bile duct injury, abscess, and intestinal perforation.[7] Concerning the induced pneumothorax, we did not observe complications resulting from this technique. Some complications such as thoracic or shoulder pain, diaphragmatic paralysis, and tension pneumothorax may occur.[68] Another potential complication is tumor seeding, particularly with subcapsular hepatocellular carcinomas. Therefore, it is recommended that multiple needle insertions into the tumor is avoided. Furthermore, a track ablation could be performed carefully along the liver and the abdominal cavity.[9]
CONCLUSION
Induced pneumothorax should be considered during ablation of hepatic dome lesions, mainly when the transhepatic access is not appropriate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/63/170732
REFERENCES
- Artificially induced pneumothorax for percutaneous transthoracic radiofrequency ablation of tumors in the hepatic dome: Initial experience. Radiology. 2005;236:666-70.
- [Google Scholar]
- Computed tomography-guided transpulmonary radiofrequency ablation for hepatocellular carcinoma located in hepatic dome. World J Gastroenterol. 2006;12:608-11.
- [Google Scholar]
- Percutaneous radiofrequency ablation therapy after intrathoracic saline solution infusion for liver tumor in the hepatic dome. J Vasc Interv Radiol. 2002;13:313-5.
- [Google Scholar]
- Radio-frequency thermal ablation with NaCl solution injection: Effect of electrical conductivity on tissue heating and coagulatio-phantom and porcine liver study. Radiology. 2001;219:157-65.
- [Google Scholar]
- Technique for creation of artificial pneumothorax for pain relief during radiofrequency ablation of peripheral lung tumors: Report of seven cases. J Vasc Interv Radiol. 2011;22:503-6.
- [Google Scholar]
- Percutaneous transthoracic radiofrequency ablation of renal tumors using an iatrogenic pneumothorax. AJR Am J Roentgenol. 2005;185:86-8.
- [Google Scholar]
- Percutaneous ablation of hepatocellular carcinoma: Current status. J Vasc Interv Radiol. 2010;21(Suppl):S204-13.
- [Google Scholar]
- Minimizing diaphragmatic injury during radiofrequency ablation: Efficazy of intraabdominal carbon dioxide insuflation. AJR Am J Roentgenol. 2004;183:197-200.
- [Google Scholar]
- Needle tract seeding after radiofrequency ablation of hepatic tumors. J Vasc Interv Radiol. 2005;16:485-91.
- [Google Scholar]






