Translate this page into:
Gastroesophageal Variceal Filling and Drainage Pathways: An Angiographic Description of Afferent and Efferent Venous Anatomic Patterns
Address for correspondence: Dr. Ron C Gaba, Department of Radiology, Division of Interventional Radiology, University of Illinois Hospital and Health Sciences System, 1740 West Taylor Street, MC 931, Chicago - 60612, Illinois, USA. E-mail: rgaba@uic.edu
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Varices commonly occur in liver cirrhosis patients and are classified as esophageal (EV), gastroesophageal (GEV), or isolated gastric (IGV) varices. These vessels may be supplied and drained by several different afferent and efferent pathways. A working knowledge of variceal anatomy is imperative for Interventional Radiologists performing transjugular intrahepatic portosystemic shunt and embolization/obliteration procedures. This pictorial essay characterizes the angiographic anatomy of varices in terms of type and frequency of venous filling and drainage, showing that different varices have distinct vascular anatomy. EVs typically show left gastric vein filling and “uphill” drainage, and GEVs and IGVs exhibit additional posterior/short gastric vein contribution and “downhill” outflow. An understanding of these variceal filling and drainage pathways can facilitate successful portal decompression and embolization/obliteration procedures.
Keywords
Anatomy
gastroesophageal varices
portal hypertension
transjugular intrahepatic portosystemic shunt

INTRODUCTION
Gastroesophageal varices are the most common form of portosystemic collateral channels that develop in patients with liver cirrhosis[1] and serve as conduits for systemic return of spleno-mesenteric venous blood in the setting of elevated portal venous pressure. These vessels are classified as esophageal (EV), gastroesophageal (GEV), or isolated gastric (IGV) varices, and can be supplied and drained by several afferent and efferent pathways.[2] Feeding veins include the left gastric (LGV), posterior gastric (PGV), and short gastric (SGV) veins, while drainage routes comprise the azygous/hemiazygous and renal venous systems. Hemorrhage from varices occurs in approximately 25% of patients with cirrhosis[34] and has a mortality incidence approximating 30% associated with each event;[3] transjugular intrahepatic portosystemic shunt (TIPS) creation and balloon-occluded antegrade/retrograde transvenous obliteration (BATO/BRTO) serve to effectively address variceal bleeding in cases refractory to first-line medical and endoscopic therapy with banding and/or sclerosis.[56] A working knowledge of variceal anatomy is imperative for the Interventional Radiologists (IRs) performing TIPS and BATO/BRTO procedures, as an understanding of variceal filling and drainage pathways can facilitate successful venography and effective embolization/obliteration during these interventions. This pictorial essay characterizes the angiographic anatomy of varices in terms of type and frequency of venous filling and drainage.
CASES
Cases for this essay were accrued from a registry of 303 patients who underwent 305 technically successful TIPS procedures between November 1999 and January 2015 in the Division of Interventional Radiology at an academic tertiary care medical center. Patients who had endoscopic diagnosis and classification of varices within 6 months of TIPS and who also had satisfactory angiographic imaging were included and they comprised 80 individuals (52 men and 28 women, median age 55 years). All cases manifested liver disease characterized by intrahepatic, sinusoidal causes of portal hypertension, such as alcohol and viral cirrhosis. Varices were categorized as EVs, GEVs, or IGVs by endoscopy; GEVs and IGVs encompassed those variceal patterns described by the Sarin classification.[2] Data on variceal feeding and draining vessels were collected by trained medical student research associates under the direct supervision of an attending IR physician via review of TIPS spleno-portal venograms on the hospital picture archiving and communication system (PACS). Venous drainage was categorized as either “uphill” (e.g. into the azygous/hemiazygous system or inferior vena cava via phrenic veins), “downhill” (e.g. into the renal venous system and then inferior vena cava), or mixed (both “uphill” and “downhill” drainage present). Data were analyzed using descriptive statistics, and comparative assessments were made using the Fisher's exact test.
VARICEAL ANATOMIC PATTERNS
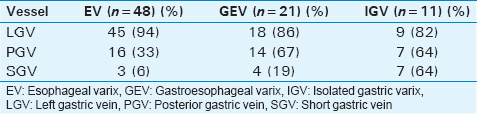
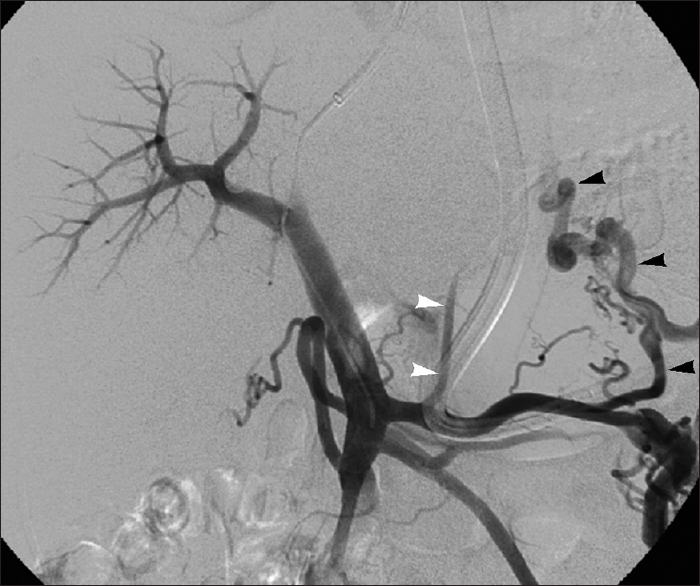
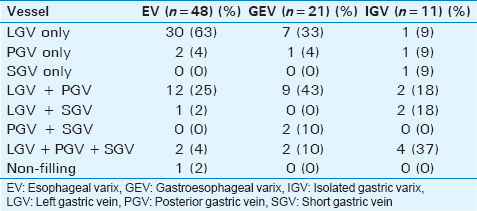
Forty-eight of 80 (60%), 21/80 (26%), and 11/80 (14%) patients had EVs, GEVs, and IGVs, respectively, a distribution consistent with the known preponderance of EVs over gastric varices (GVs) in cirrhotic patients.[789] The incidence of variceal feeding vessels by varix type is shown in Table 1; the distribution of feeding vessel types showed a statistically significant difference between EVs and IGVs (P = 0.002, Fisher's exact test), but not between EVs and GEVs or GEVs and IGVs. EVs were commonly supplied by LGVs [Figure 1], while they were less frequently supplied by PGVs [Figure 2] and rarely by SGVs [Figure 3]. GEVs were usually filled by LGVs and PGVs [Figure 4], but not by SGVs [Figure 5]. IGVs were regularly fed by LGVs, PGVs, and SGVs [Figure 6].

- Classic EV supply in 59-year-old woman with grade 3 EVs. Splenoportal venogram performed during TIPS creation demonstrates EV supply via LGV (arrowheads).
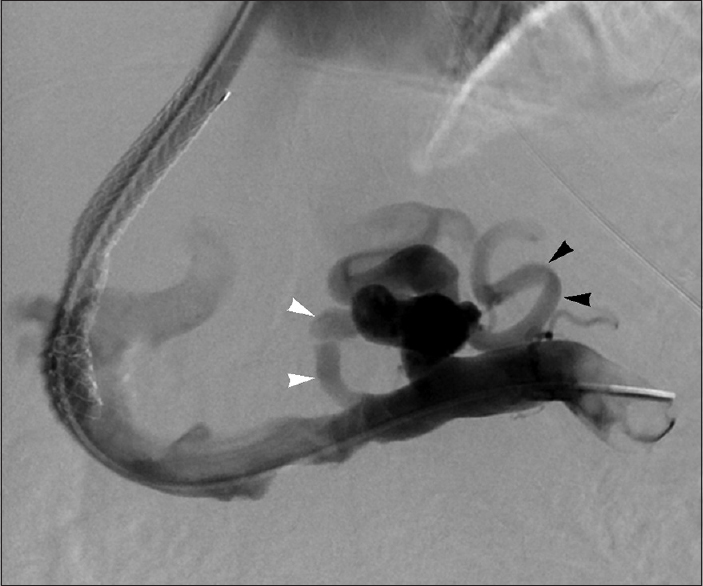
- Atypical EV supply in 66-year-old woman with grade 2 EVs. Splenoportal venogram performed after TIPS creation reveals EV inflow via medial (white arrowheads) and lateral (black arrowheads) PGVs.
- Uncommon EV supply in 68-year-old man with grade 3 EVs. Splenoportal venogram performed during TIPS creation shows EV filling via large SGV (black arrowheads) and small LGV (white arrowheads).

- Typical GEV supply in 56-year-old man with type 1 GEVs. Portal venogram performed after TIPS creation depicts GEV supply from LGV (white arrowheads) and PGV (black arrowheads).

- Unusual GEV supply. 52-year-old man with type 1 GEVs. Splenoportal venogram performed during TIPS creation illustrates GEV inflow from PGV (black arrowheads) and SGV (white arrowheads).
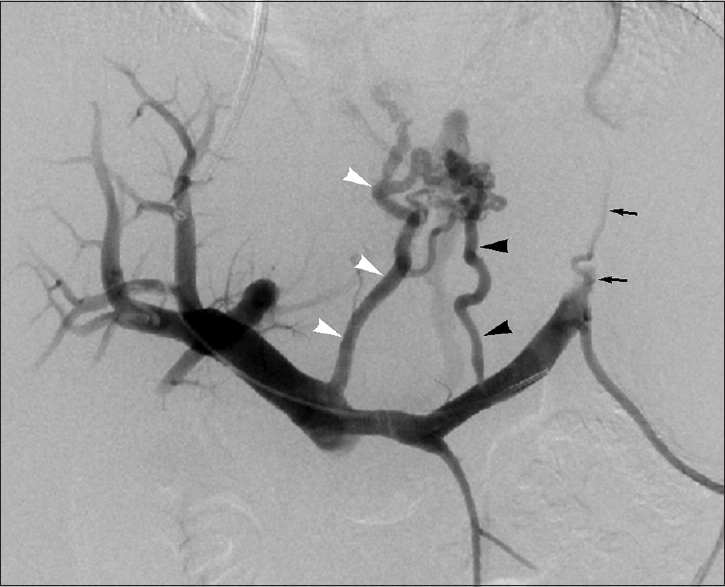
- Standard IGV supply in 56-year-old woman with type 1 IGVs. Splenoportal venogram performed during TIPS creation displays IGV filling via LGV (white arrowheads), PGV (black arrowheads), and SGV (arrows).
The patterns of variceal feeding vessels by varix type are shown in Table 2. The most common pattern of EV filling was by LGV alone (63%) followed by LGV and PGV (25%). The usual pattern of GEV inflow was from LGV and PGV (43%) or LGV alone (33%). The most frequent pattern of IGV supply was by LGV, PGV, and SGV (37%), followed by LGV and PGV (18%) or LGV and SGV (18%).
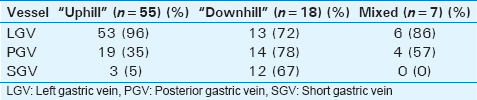
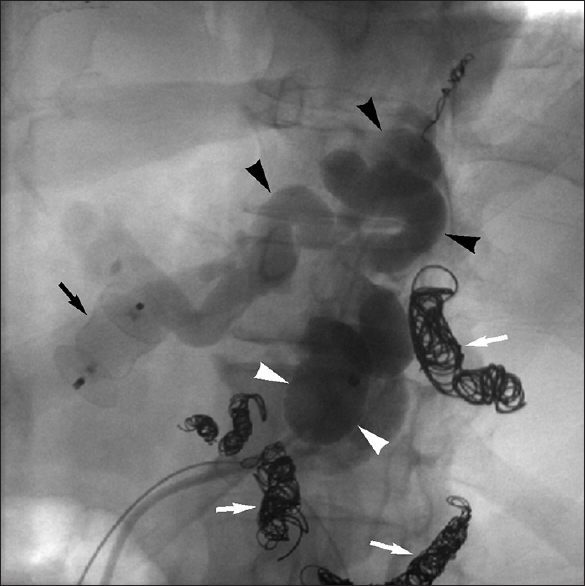
Regarding drainage, most EVs (37/48, 77%) had “uphill” outflow into the azygous system [Figure 7], while most IGVs (9/11, 82%) drained “downhill” into left renal shunts [Figure 8]; GEVs had “mixed” drainage (11/21, 52% “uphill”; 8/21, 38% “downhill”; and 2/21, 10% “uphill” and “downhill”) [Figure 9]. “Downhill” or mixed EV drainage [Figure 10] and “uphill” IGV outflow [Figure 11] were uncommon. The relationship between variceal feeding vessels and drainage pattern type is presented in Table 3, which indicates an association between the presence of PGV and/or SGV variceal supply and “downhill” variceal outflow. To this end, the distribution of feeding vessel types showed a statistically significant difference between “uphill” and “downhill” draining varices (P < 0.001, Fisher's exact test), but not between “downhill” and mixed or “uphill” and mixed drainage types.
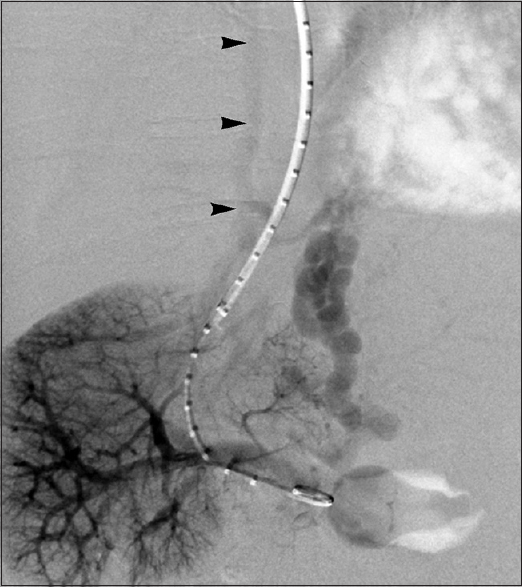
- Conventional EV drainage in 59-year-old man with grade 3 EVs. Delayed portal venogram performed during TIPS creation demonstrates EV outflow via azygous venous system (arrowheads).

- Mixed GEV drainage in 51-year-old man with type 1 GEVs. Delayed portal venogram performed during TIPS creation reveals GEV outflow via azygous venous system (white arrowheads) and left gastrorenal shunt (black arrowheads).
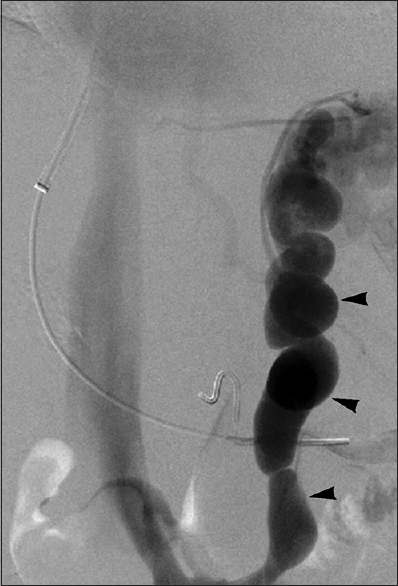
- Archetypal IGV drainage in 53-year-old woman with type 1 IGVs. Delayed splenoportal venogram performed during TIPS creation shows IGV drainage via large left gastrorenal shunt (arrowheads).

- Atypical EV drainage in 59-year-old man with grade 2 EVs. Splenoportal venogram performed during TIPS creation depicts outflow via left gastrorenal shunt (arrowheads).

- Uncommon IGV drainage in 51-year-old woman with type 2 IGVs. Left gastric venogram performed after TIPS creation illustrates outflow via azygous venous system (arrowheads).
DISCUSSION
Familiarity and understanding of variceal vascular anatomy has important implications for the technical approach to variceal hemorrhage therapy and is thus essential information for IRs involved in the management of cirrhotic patients with portal hypertension. This pictorial essay illustrates both typical and atypical variceal feeding and drainage pathways, and the incidence and patterns of variceal filling and drainage depicted herein are in line with earlier reports.[10] In a 75 patient cohort described by Chikamori et al., the EVs were supplied by the LGV, PGV, and SGV in 100%, 25%, and 11% of cases, respectively, while the IGVs were filled via the LGV, PGV, and SGV in 70%, 70%, and 25% of the cases, respectively.[10] EV outflow was “uphill” in 100% of cases, while IGV outflow was “uphill” in 15% of cases and “downhill” in 85%.[10] While studying variceal anatomy via portal venography in 230 patients, Watanabe et al., found that GVs are more commonly supplied by PGVs and SGVs, and more frequently drain via “downhill” gastrorenal shunts.[11] In a recent review of the computed tomography (CT) anatomy of gastric variceal drainage routes, Kiyosue et al., also noted “downhill” drainage of IGVs in most (80–85%) cases.[12] The findings of the current series indicate that EVs have the most simple vascular supply patterns, while GEVs and IGVs have progressively more complex feeding vessel configurations. Moreover, the data presented indicate that LGVs almost universally contribute to all variceal types, while PGVs more commonly supply varices with gastric components and SGVs most frequently feed IGVs. This information may be used as a guide by IRs on the likely vascular anatomy when pursuing embolization or obliteration.
Successful identification of variceal filling and drainage conduits is based on the performance of thorough splenoportography during TIPS procedures, which is critical to avoid neglect of patent varices through inadequate venographic technique. Catheter position at the splenic hilum during venography optimizes the likelihood of opacifying all variceal feeders, while omission of diligent splenoportography during TIPS cases may result in lack of identification of vessels supplying varices (especially gastric) that may later contribute to rebleeding. Attentive consideration should thus be given to splenoportal venographic technique during TIPS procedures.
Antegrade variceal occlusion involves coil embolization of or obliteration from afferent variceal feeders, while retrograde variceal therapy typically comprises balloon-occluded obliteration. Given the predominant isolated supply by the LGV, most EVs can successfully be treated with single-vessel coil embolization via antegrade access [Figure 12]. For this reason, and because these vessels lack efferent limbs that may be easily catheterized, most EVs are treated from an antegrade approach. GEVs can similarly be treated from antegrade access, although PGV occlusion is also frequently necessary [Figure 13]. Retrograde obliteration of GEVs may be pursued in the half of cases in which “downhill” drainage is present. Given the frequent supply by LGVs, PGVs, and SGVs, antegrade therapy of IGVs may require complex embolotherapy of multiple vessels [Figure 14]. However, because IGVs may be relatively more difficult to treat via portal decompression and embolization as compared to other varices,[5] IGVs are commonly treated in a retrograde fashion via gastrorenal outflow pathways [Figure 15].

- LGV embolization for treatment of grade 3 EVs in 35-year-old woman. Portal venogram (a) performed during TIPS creation displays EV supply via LGV (arrowheads). Left gastric venogram (b) performed after coil embolization shows complete occlusion of LGV (arrowhead).

- LGV and PGV embolization for treatment of type 2 GEVs in 51-year-old man. Splenoportal venogram (a) performed during TIPS creation displays GEV supply via LGV (white arrowheads) and PGV (black arrowheads). Splenoportal venogram (b) performed after coil embolization demonstrates complete occlusion of LGV (white arrowhead) and PGV (black arrowhead).
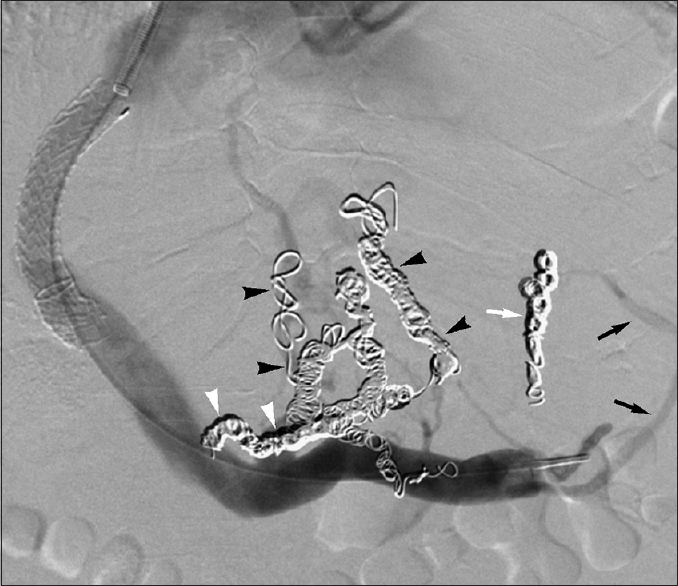
- LGV, PGV, and SGV embolization for treatment of type 1 IGVs in 38-year-old man. Splenoportal venogram performed after TIPS creation and multi-vessel embolization of LGV (white arrowheads), PGVs (black arrowheads), and SGV (white arrow) reveals predominant variceal occlusion, although persistent SGV feeder is present (black arrows).
- Balloon-occluded retrograde venogram performed during balloon-occluded retrograde obliteration of type 1 IGVs in 53-year-old man depicts occlusion balloon (white arrowheads) in left gastrorenal shunt and retrograde filling of gastric varices (black arrowheads). Note previously embolized LGV (black arrow), as well as PGVs and SGV (white arrows).
CONCLUSION
Different types of varices, including EVs, GEVs, and IGVs, have distinct vascular anatomy, with EVs typically showing LGV filling and “uphill” drainage, and GEVs and IGVs exhibiting additional PGV and SGV contribution and “downhill” outflow. An understanding of these variceal filling and drainage pathways can facilitate successful venography and variceal embolization/obliteration during TIPS and BATO/BRTO procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/61/170730
REFERENCES
- Gastric varices: Profile, classification, and management. Am J Gastroenterol. 1989;84:1244-9.
- [Google Scholar]
- North Italian Endoscopic Club for the Study and Treatment of Esophageal Varices. Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter study. N Engl J Med. 1988;319:983-9.
- [Google Scholar]
- Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922-38.
- [Google Scholar]
- American Association for the Study of Liver Diseases. The Role of Transjugular Intrahepatic Portosystemic Shunt (TIPS) in the Management of Portal Hypertension: Update 2009. Hepatology. 2010;51:306.
- [Google Scholar]
- Balloon-occluded Retrograde Transvenous Obliteration (BRTO): Technical results and outcomes. Semin Intervent Radiol. 2011;28:333-8.
- [Google Scholar]
- Variceal and other portal hypertension related bleeding. Best Pract Res Clin Gastroenterol. 2013;27:649-64.
- [Google Scholar]
- Risk factors for hemorrhage from gastric fundal varices. Hepatology. 1997;25:307-12.
- [Google Scholar]
- Prevalence, classification and natural history of gastric varices: A long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343-9.
- [Google Scholar]
- Correlation between endoscopic and angiographic findings in patients with esophageal and isolated gastric varices. Dig Surg. 2001;18:176-81.
- [Google Scholar]
- Portal hemodynamics in patients with gastric varices. A study in 230 patients with esophageal and/or gastric varices using portal vein catheterization. Gastroenterology. 1988;95:434-40.
- [Google Scholar]
- Multidetector CT anatomy of drainage routes of gastric varices: A pictorial review. Radiographics. 2013;33:87-100.
- [Google Scholar]






