Translate this page into:
Mechanical Thrombectomy with Rotarex System in Buerger's Disease
Address for correspondence: Dr. Ozgur Kilickesmez, Department of Diagnostic and Interventional Radiology, Istanbul Education and Research Hospital, Samatya - 34000, Istanbul, Turkey. E-mail: okilickesmez@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report the case of a patient with 2-month history of chronic thromboembolism of the distal superficial femoral and popliteal arteries with diagnostic features of thromboangiitis obliterans disease. The occlusion could not be crossed by antegrade approach and was achieved retrogradely via dorsalis pedis artery puncture followed by mechanical removal of the thrombus with Rotarex system (Straub Medical AG, Wangs, Switzerland). Subsequent ballooon angioplasties achieved exclusion of the thrombus, and straight-line flow established to the foot through the anterior tibial Artery. The present case report demonstrates the success of mechanical thrombectomy in a patient with Buerger's vasculitis.
Keywords
Buerger's disease
mechanical thrombectomy
Rotarex
thromboangiitis obliterans
INTRODUCTION

Thromboangiitis obliterans (TAO), also known as Buerger's disease, is a nonatherosclerotic inflammatory disease of the small-sized and medium-sized arteries and veins of the arms and legs. Pathologically, the condition is distinguished from other forms of vasculitis by a highly cellular, inflammatory intraluminal thrombus with relative sparing of the vessel wall and, more specifically, sparing of the internal elastic lamina.[1] Patients are young heavy smokers who present with distal extremity ischemia, ischemic digit ulcers, or digit gangrene.
There is no definite consensus regarding the treatment of lower extremity involvement. The choices are cessation of smoking and symptomatic medical treatment, sympathectomy, surgical vascularization, or novel experimental therapies aiming to stimulate angiogenesis. Endovascular treatment is another option; however, only a few cases exist in the literature defining only thrombolysis and angioplasty.[234]
Since Buerger's disease is a type of vasculitis, mechanical thrombectomy is not the technique used by interventionalists. Here, we report a case with late onset of Buerger's disease incidentally detected during the angiography performed for thromboembolic occlusion and treated with Rotarex mechanical thrombectomy device. The Rotarex thrombectomy system combines two essential effects, mechanical clot fragmentation and removal of the fragmented material from the vessel under negative pressure, which purports to prevent peripheral embolization.[5] We report the first use of a mechanical thrombectomy device for endovascular revascularization in Buerger's disease.
CASE REPORT
A 44-year-old man experienced sudden onset of pain in the left leg that decreased gradually. He was admitted to the hospital 1 week after an ulceration occurred on the left toe. Examination of the left lower extremity revealed a cold foot that was pale and without palpable pulse. Clinically, he was believed to have a threatened limb, but not irreversible ischemia (class III in the Rutherford classification of acute ischemia). Detailed medical history of the patient also revealed intermittent claudication for the last 2 years. He was a 1.5-pack-a-year smoker for 25 years. Color Doppler ultrasonography revealed occlusion of the distal segment of the left superficial femoral artery and the popliteal artery. There was monophasic dampened flow in both distal leg vessels. Then, revascularization of the presumably chronic thromboembolic occlusion of the the left superficial feromaral artery (SFA) and popliteal artery was planned to be performed in antegrade route via the ipsilateral common femoral artery (CFA). The patient agreed to undergo the procedure. The procedure was explained to the patient, and written informed consent was obtained. The procedure was performed in the angiography suite. The patient was placed under conscious sedoanalgesia with dormicum and fentanyl, and was monitored. After placing a 6F vascular sheath into the femoral artery, heparin was administered at a dose of 5000 IU. An angiogram obtained via the sheath revealed an abrubt thromboembolic occlusion of the distal SFA and the popliteal arteries. The trifucation arteries were occluded and, unexpectedly, the typical “corkscrew collateral” arteries could be seen in the images diagnostic for TAO [Figure 1]. Though we could get through the thrombus, attempts aiming to get access to leg arteries were unsuccessful despite the application of various guidewires and support catheters. Then, a retrograde approach via dorsalis pedis artery was planned and was achieved with ultrasound-guided micropuncture. The occluded part of the vessel was successfully recanalized by navigating a 0.018-inch, V-18 Control (Boston Scientific/Medi-tech, Natick, MA, USA) guidewire through dorsalis pedis artery upward with support from a glide Vertebral (Cordis, Warren, New Jersey, USA) catheter.[6] Subsequent to the catheterization of the true lumen of the SFA, angioplasty of the anterior tibial artery with 2 mm × 10 cm balloons distally and 3 mm × 10 cm balloons proximally (Cook Incorporated, Bloomington, IN, USA) was performed. The popliteal artery occlusion was crossed with balloon angioplasty of the occlusion. The occluded popliteal artery and anterior tibial artery (ATA) opened up well with balloon angioplasty. Following distal recanalization, an SFA roadmap with an antegrade vertebral catheter was obtained. Afterward, a 6 F Rotarex system (Straub Medical AG, Wangs, Switzerland) was navigated over a 0.018-inch guidewire for removal of the thrombi. The Rotarex system was advanced over this guidewire up to a few centimeters above the thrombotic occlusion and then activated. The occlusion was passed slowly. Small forward and backward movements were performed three times and we obtained an angiogram that revealed restoration of the flow except slight irregular residual chronic thrombi attached to the vessel wall. Angioplasty of the SFA was performed with a 0.018-inch wire using a 5 × 40 mm angioplasty balloon (Cook Incorporated). Completion angiogram showed complete exclusion of the thrombus, and straight-line flow established to the foot through the native popliteal artery and ATA [Figure 2]. The total procedure time was 2 h and 10 min. The patient responded very well to the treatment and was fully mobile the following morning. He was discharged in the same week. The ulcer healing began within a few days and took 3 weeks for recovery. A lifelong daily dose of 300 mg Aspirin (acetylsalicylic acid) was recommended for the patient. The patient was seen at the first and third months after treatment. Doppler ultrasound examination performed at the third month showed patency. However, although planned, the patient did not return for the sixth month follow-up investigation.
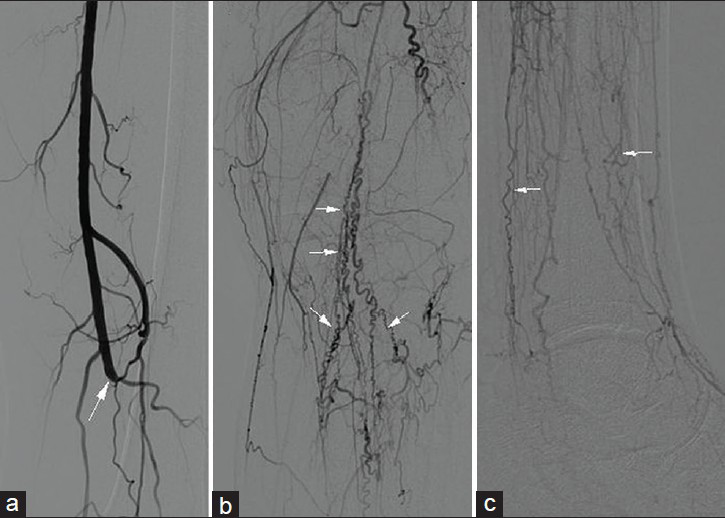
- 44-year old male patient with sudden onset of pain in left leg and ulcer on the toe, diagnosed with Buerger's disease. Baseline digital substraction angiography of (a and b) the popliteal region and (c) leg demonstrates abrubt thromboembolic occlusion of the popliteal artery (large white arrow in a). Typical corkscrew collateral arteries (small white arrows in b and c) and occlusion of the run-off vessels in concordance with Buerger's disease before intervention.
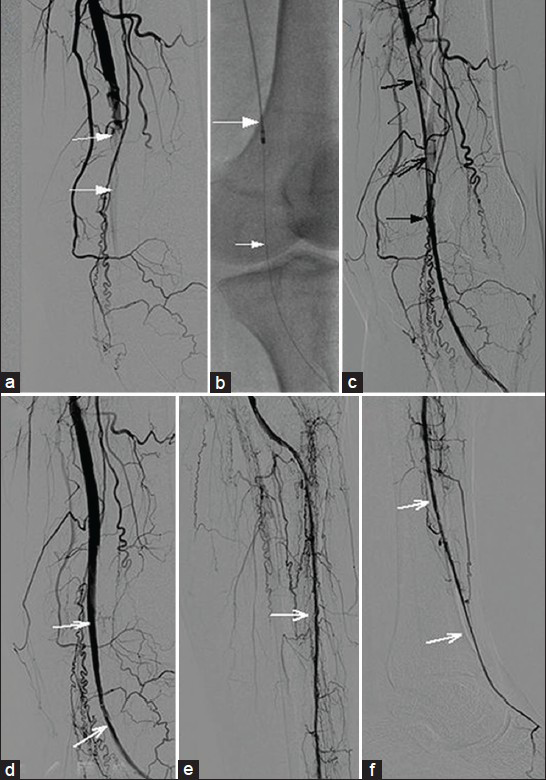
- 44-year-old male patient with sudden onset of pain in left leg and ulcer on the toe, diagnosed with Buerger's disease. Digital substraction angiography of (a–d) the popliteal region and (e and f) leg during mechanical thrombectomy of the distal popliteal artery with Rotarex and reconstruction of flow to the foot. (a) Complete occlusion of the popliteal artery above the knee joint involving the trifurcation and all three lower limb artery origins (white arrows). (b) 6F Rotarex catheter (large white arrow) over the 0.018-inch wire (small white arrow). (c) Partial removal of the thrombus (open black arrows) and recanalization of the popliteal artery (black arrow) after retrograde re-entry to the true lumen following dorsalis pedis access (not shown). (d) Using the rotarex catheter, the clot was destroyed and removed totally. Patent anterior tibial artery is visible (white arrows). (e and f) Flow was reconstructed to the foot via anterior tibial artery (white arrows).
DISCUSSION
Endovascular treatment is well established for ischemic legs, whether embolic or chronic occlusions. Thrombolysis, clot aspiration, mechanical thrombectomy, and revascularization techniques like balloon angioplasty or stenting for chronic occlusions are the accepted techniques worldwide.[5] However, endovascular treatment for TAO is not well known. Bypass surgery may be considered in selected patients with severe ischemia and suitable distal target vessels. However, for most patients, TAO surgery is difficult since bypasses must be very distal and patency is poor.[7]
Hodgson et al., reported the first case of TAO with acute ischemia treated by angioplasty and thrombolysis.[4] Then, Graziani et al., published a paper demonstrating the effectiveness of an extensive endovascular treatment.[5] They could manage treatment successfully in 19 of 20 limbs, achieving technical success in 95%. No mortality or complication related to the procedure was observed. During a mean follow-up of 23 months (standard error: ±4.05), amputation-free survival with no need of major amputation in any case and sustained clinical improvement were achieved in 16 of the 19 limbs (84.2%) successfully treated, resulting in a 100% limb salvage rate (19/19). Another case report also demonstrated a successful revascularization by angioplasty of the posterior tibial and plantar artery stenoses.[2] In the present case, we were unaware of the patient's TAO disease, though we could manage to cross trombotic occlusion it was not possible to reenter the distal true lumen of the crural arteries. Then, as a secondary option, dorsalis pedis artery was punctured and retrograde cross was successful. Approximately 20% of patients with complex crural occlusions cannot be treated using the conventional antegrade approach. After revascularization failure, 40–50% of these patients will lose their leg within 6 months and up to 20% will die.[8]
The Rotarex mechanical thrombectomy catheter used in the present case consists of two cylinders with side slits. The inner cylinder is fixed to the catheter shaft and the outer cylinder to a rotating spiral driven by an electric motor at 40–60,000 revolutions per minute. The rotation at this speed causes negative pressure and the occlusion material is sucked into the aspiration slits where it is macerated and then aspirated. Aspiration material is transported up the catheter by the rotating spiral into an aspiration bag. Stanek et al., reported that the Rotarex system enables fast and efficient treatment of peripheral arterial thromboembolic occlusions.[9] It is reported to be a safe tool for the treatment of acute, subacute, or even chronic peripheral arterial thromboembolic occlusions. It can be used for short or long occlusions with equal success, provided the obstruction is not heavily calcified and a guidewire has been safely passed through the obstruction. To the best of our knowledge, this is the first report of mechanical thrombectomy performed successfully in a vasculitic occlusion.
CONCLUSION
Although not frequent, TAO may be diagnosed as an underlying factor in patients with thromboembolic occlusions. Mechanical thrombectomy may be kept in mind in selected patients with TAO. However, this technique should be assessed in a large series prior to drawing a conclusion regarding the success of this technique.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/14/152609
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Endovascular treatment is a hope for patient with Buerger's disease and foot ulcer: Case report. Int J Low Extrem Wounds. 2012;11:165-8.
- [Google Scholar]
- Clinical outcome after extended endovascular recanalization in Buerger's disease in 20 consecutive cases. Ann Vasc Surg. 2012;26:387-95.
- [Google Scholar]
- Thrombolysis and angioplasty for acute lower limb ischemia in Buerger's disease. Cardiovasc Intervent Radiol. 1994;17:333-5.
- [Google Scholar]
- Mechanical thrombectomy in acute and subacute leg ischemia. Acta Chir Belg. 2003;103:548-54.
- [Google Scholar]
- US-guided retrograde tibial artery puncture for recanalization of complex infrainguinal arterial occlusions. Diagn Interv Radiol. 2013;19:134-40.
- [Google Scholar]
- A review on thromboangiitis obliterans pathophysiology: Thrombosis and angiitis, which is to blame? Vascular. 2011;19:141-53.
- [Google Scholar]
- Percutaneous aspiration thrombectomy in the treatment of lower extremity thromboembolic occlusions. Diagn Interv Radiol. 2010;16:79-83.
- [Google Scholar]
- Mechanical thrombectomy using the Rotarex catheter-safe and effective method in the treatment of peripheral arterial thromboembolic occlusions. Vasa. 2010;39:334-40.
- [Google Scholar]






