Translate this page into:
Paratesticular Solitary Plasmacytoma
Address for correspondence: Dr. Mehmet Ruhi Onur, Department of Imaging Sciences, Research Assistant Professor, University of Rochester School of Medicine, 601 Elmwood Avenue 14642, NY, USA ruhionur@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Primary solid neoplasms of the extratesticular tissues are rare. The reported prevalence rate of paratesticular neoplasms is between 3% and 16% of all patients referred for scrotal ultrasonography. A plasmacytoma is a discrete, solitary mass of malignant monoclonal plasma cells that can arise in any part of the body. In this report, we present a case of a paratesticular solid mass detected in an 80-year-old patient that proved to be primary extraosseous plasmacytoma on surgery, and discuss its sonographic features.
Keywords
Plasmacytoma
paratesticular mass
sonography
INTRODUCTION

Neoplasms arising in the paratesticular region comprise of heterogeneous group of tumors arising from the spermatic cord, epididymis, or vestigial remnants in the scrotum. The majority of paratesticular tumors are benign with the prevalence of malignancy being approximately 3% as opposed to intratesticular masses that are mostly malignant.[1]
A plasmacytoma represents a discrete mass of neoplastic plasma cells identical to plasma cell myeloma but occurs as a localized disease and differs from multiple myeloma with the absence of hypercalcemia, renal insufficiency and anemia, normal skeletal survey, absence of bone marrow plasmacytosis, and serum or urinary para-protein levels being less than 2 g/dl.[2] A plasmacytoma may be medullary (osseous) that occupies bone marrow or extramedullary (extra-osseous). Typical extra-osseous sites of plasmacytoma in the abdominopelvic region include the liver, spleen, and lymph nodes.[3] Occurrence of primary plasmacytoma in the testis and secondary involvement of the testis by relapsing multiple myeloma has been reported.[45]
In this report, we discuss the sonographic features of a primary paratesticular plasmacytoma (PPP) with pathologic correlation and the differential diagnosis of solid paratesticular masses. To our knowledge there is no reported radiologic description of PPP in the literature.
CASE REPORT
An 80-year-old man presented to the hospital with a complaint of a painless scrotal mass. His physical examination revealed a firm, extratesticular scrotal mass. Laboratory tests for alpha fetoprotein (AFP) and beta human chorionic gonadotropin (HCG) were negative.
Ultrasonography was performed with a 12-MHz linear array transducer (Phillips Medical Systems). Gray-scale ultrasound of the scrotum revealed a right side, well-defined paratesticular, solid mass at the superior pole of the testis with spoke wheel appearance [ Figure 1a]. Color flow Doppler examination demonstrated increased vascularity of this mass [Figure Figure 1b]. Epididymis was within normal limits. Pampiniform plexus was displaced superiorly. A differential diagnosis of metastatic lesion and paratesticular sarcoma were considered. Surgery confirmed a firm, well-circumscribed solid mass arising from the paratesticular region near the superior pole of the testis.
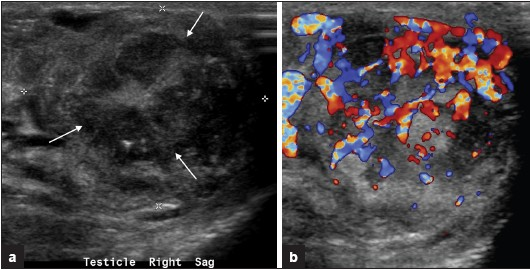
- a) Right paratesticular gray-scale ultrasound of the scrotum in longitudinal plane demonstrates a well-defined solid paratesticular mass with spoke-wheel appearance (arrows). (b) Corresponding color flow Doppler image demonstrates increased internal vascularity.
Enucleation of the paratesticular mass was done with preservation of ipsilateral testis and spermatic cord.
Histopathologic examination of the surgical specimen confirmed the diagnosis of primary plasmacytoma consisting of malignant plasma cells. Amyloid deposition was present along with the neoplastic changes [Figure 2a]. The nuclei of plasma cells were localized peripherally with a typical clock-face pattern Figure 2b
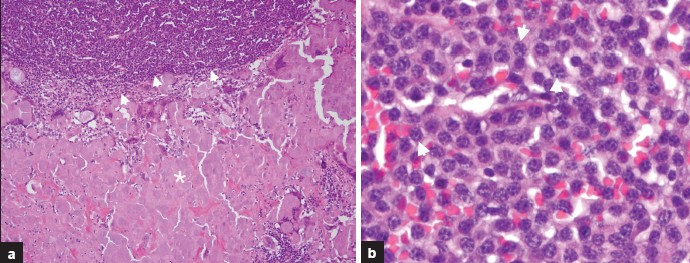
- (a) Hematoxylin and eosin stain (100× original magnification) demonstrates amyloid deposition (asterisk) with tumoral cell infiltration (arrowheads). (b) Hematoxylin and eosin stain (400× original magnification) of the tumoral infiltration area reveals typical clock face pattern nuclei (arrowheads) in plasma cells diagnostic of plasmacytoma.
DISCUSSION
Paratesticular tissues are histogenetically derived from a variety of epithelial, mesothelial, and mesenchymal elements and consist of epididymis, spermatic cord, and vestigial remnants. Primary solid neoplasms of the extratesticular tissues are rare, although their reported prevalence varies between 3% and 16% of all patients referred for scrotal ultrasonography.[6]
A plasmacytoma is a discrete, solitary mass of malignant monoclonal plasma cells that can arise in any part of the body. Primary extramedullary plasmacytomas comprise only 4% of all plasma cell malignancies and most often occur in the upper aerodigestive tract.[7] Testicular and paratesticular plasmacytomas are extremely rare. In general plasmacytomas on gray-scale ultrasound have variable echotexture with ill-defined margins and increased vascularity on color flow Doppler evaluation.[4] Testicular plasmacytomas results in enlargement of the testis and ultrasound examination reveals intratesticular ill-defined predominantly hyperechoic masses with hypoechoic areas and linear flame-shaped hypervascularity. This hypervascularity seen in intratesticular plasmacytoma has very close resemblance to testicular lymphoma.[4] Extramedullary plasmacytomas may demonstrate soft tissue attenuation with homogeneous contrast enhancement on computed tomography (CT).[3] Magnetic resonance imaging demonstrates solid tumor that is isointense on T1-weighted and iso- to hyperintense relative to muscle on T2-weighted images with marked enhancement after intravenous contrast administration.[7] A mild heterogeneous F-18 fluoro-d-glucose uptake in a retroperitoneal primary plasmacytoma has been reported on positron emission tomography.[7] Large plasmacytomas may show areas of necrosis and usually present with destruction, infiltration, or encasement of adjacent structures.
Differential diagnosis of benign paratesticular masses includes adenomatoid tumor, lipoma, leiomyoma, fibrous pseudotumor, and sclerosing lipogranuloma. Paratesticular malignant masses to be considered in the differential diagnosis include sarcomas, malignant fibrous histiocytoma, lymphoma, and metastases.
Adenomatoid tumor is the most common epididymal tumor and accounts for approximately 30% of all paratesticular neoplasms, second only to lipoma.[1] Adenomatoid tumors may rarely arise from the testicular tunica and testis and, on rare occasions, occur in the spermatic cord.[8] Majority of adenomatoid tumors are isoechoic relative to the adjacent epididymis and hypovascular on color flow Doppler examination.[18] Leiomyomas have variable ultrasound appearance, depending on whether it is predominantly solid or cystic, and may contain calcifications. Lipomas have a homogeneous hyperechoic appearance on ultrasound. Fibrous pseudotumor appears hypoechoic on ultrasound examination. Fifty percent have an associated hydrocele or hematocele, with 30% having a prior history of trauma or epididymo-orchitis. Sclerosing lipogranuloma are usually associated with foreign body reaction and appear hypoechoic on ultrasound. Solitary fibrous tumors of paratesticular origin are well-defined solid masses and have rich tumor vascularity similar to plasmacytoma.[8]
Rhabdomyosarcoma is the commonest malignant paratesticular tumor in scrotum (40%) that most commonly occurs in children. On ultrasound examination rhabdomyosarcomas have variable echogenicity on gray-scale US secondary to associated hemorrhage and necrosis. Color Doppler ultrasound shows increased flow and low resistance. Ultrasound examination of liposarcomas demonstrates predominantly hyperechoic appearance, although echogenicity may vary. Leiomyosarcomas are typically located in the scrotal part of the spermatic cord and have similar appearance to that of liposarcomas.[8]
Extratesticular metastases have very non-specific appearance and originate from testicular, renal, prostate, and gastrointestinal tumors. Metastatic melanoma, anal carcinoma, and squamous cell lung carcinoma have also been reported.[9]
The paratesticular mass we have described had a very distinct spoke-wheel appearance on gray-scale ultrasound with increased vascularity on color flow Doppler evaluation. This entity has never ever been reported in the imaging literature. Our patient was investigated for the presence of systemic myeloma and no evidence was found.
In conclusion, radiologists should consider extratesticular plasmacytoma in the differential diagnosis of solid and hypervascular paratesticular tumors in an adult since up to 14% of patients may convert to multiple myeloma on follow up.[10]
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/52/86667
REFERENCES
- From the archives of the AFIP: Extratesticular scrotal masses. Radiographics. 2003;23:215-40.
- [Google Scholar]
- Primary extramedullary plasmacytoma in retroperitoneum: CT and integrated PET/CT findings. Eur J Radiol. 2007;62:57-61.
- [Google Scholar]
- Extramedullary plasmacytoma of the pancreas as an uncommon cause of obstructive jaundice: A case report. J Med Case Reports. 2009;3:8785.
- [Google Scholar]
- Plasmacytoma of the testis in a patient with previous multiple myeloma: Is the testis a sanctuary site. J Clin Oncol. 2010;28:456-8.
- [Google Scholar]
- Atlas of tumor pathology, fasc 25, ser 3. Armed Forces Institute of Pathology: Washington DC; 1999. p. :235-366.
- [Google Scholar]
- Extramedullary plasmacytoma involving perirenal space accompanied by extramedullary hematopoiesis and amyloid deposition. Jpn J Radiol. 2010;28:309-13.
- [Google Scholar]
- Multimodality imaging of paratesticular neoplasms and their rare mimics. Radiographics. 2003;23:1461-76.
- [Google Scholar]
- Sonographic appearance of scrotal wall metastases from lung adenocarcinoma. Am J Roentgenol. 2002;179:1647-8.
- [Google Scholar]
- Extramedullary plasmacytoma.Tumor occurrence and therapeutic concepts. Cancer. 1999;85:2305-14.
- [Google Scholar]






