Translate this page into:
Imaging Acute Appendicitis: State of the Art
Address for correspondence: Prof. Diana Gaitini, Unit of Ultrasound, Department of Medical Imaging, Rambam Medical Center, Ha’aliya 8, POB 9602, Haifa, Israel. E-mail: d_gaitini@rambam.health.gov.il
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The goal of this review is to present the state of the art in imaging tests for the diagnosis of acute appendicitis. Relevant publications regarding performance and advantages/disadvantages of imaging modalities for the diagnosis of appendicitis in different clinical situations were reviewed. Articles were extracted from a computerized database (MEDLINE) with the following activated limits: Humans, English, core clinical journals, and published in the last five years. Reference lists of relevant studies were checked manually to identify additional, related articles. Ultrasound (US) examination should be the first imaging test performed, particularly among the pediatric and young adult populations, who represent the main targets for appendicitis, as well as in pregnant patients. A positive US examination for appendicitis or an alternative diagnosis of possible gastrointestinal or urological origin, or a negative US, either showing a normal appendix or presenting low clinical suspicion of appendicitis, should lead to a final diagnosis. A negative or indeterminate examination with a strong clinical suspicion of appendicitis should be followed by a computed tomography (CT) scan or alternatively, a magnetic resonanace imaging (MRI) scan in a pregnant patient. A second US examination in a patient with persistent symptoms, especially if the first one was performed by a less experienced imaging professional, is a valid alternative to a CT.
Keywords
Abdominal imaging
appendicitis
compression ultrasound
multidetector computed tomography
magnetic resonance imaging
INTRODUCTION

Acute appendicitis is the most common diagnosis suspected in patients presenting in emergency rooms with acute abdominal pain, and is the most common indication for an urgent abdominal intervention. Yet, it is difficult to diagnose based solely on the patient's medical history, physical examination, and laboratory findings. Gastrointestinal and urogenital disorders are appendicitis-mimicking conditions. In a pregnant patient, appendicitis is the most common cause of surgery-requiring abdominal pain. Both delayed and unnecessary interventions may lead to adverse fetus outcomes.[1–3]
A mean negative appendectomy rate of 26% (16–47%) have been reported when the diagnosis is based only on clinical and laboratory findings, dropping to 6–10% when imaging is performed.[45] Therefore, the use of imaging modalities is critical to confirm the diagnosis, when facing a clinical suspicion of appendicitis.
Currently, there is no uniform protocol regarding the use of imaging tests, with some centers starting with ultrasound (US) and others with computed tomography (CT), according to their availability and local experience. Hence, there is a need for guidelines regarding the optimal patient-tailored imaging modality to begin with, and an algorithm for determining further imaging procedures.
Meta-analyses of CT and US in the diagnosis of appendicitis were published by researchers from the University of Amsterdam, based on articles published between January 1994 and February 2006,[6] and from the University of Toronto, based on publications from 1986 to 2004.[7]
In the present review, data from relevant articles on appendicitis imaging published from February 2006 to March 2011 was retrieved from a computerized database (MEDLINE).
The aim of this review is to analyze the diagnostic capabilities of US, CT, and MRI in patients suspected of suffering from acute appendicitis, based on articles published in the last five years.
Gray-scale graded compression and color Doppler ultrasound examination
High-resolution linear array transducers with harmonics and compound capabilities in modern US systems allow optimal definition of the structures at the right lower quadrant. In obese patients, a convex array lower frequency transducer may be needed to achieve better penetration. Bowel wall and peristalsis, Iliopsoas muscle, iliac vessels, mesenteric fat, and mesenteric lymph nodes are clearly defined.
The normal appendix can be visualized from the base of the cecum as a blind-ended, gut-pattern aperistaltic tubular structure, with a wall thickness of 2 mm or less and a 6–7 mm or less diameter [Figure 1].[8]

- A 31-year-old-female with right lower quadrant abdominal pain for two days. Normal appendix on US. (a) Long-axis view. (b) Short axis view. A blind-ended, gut-pattern tubular structure (arrows), with 2 mm wall thickness and 4.5 mm lumen width (cursors) is seen anterior to the right common iliac vessels on gray-scale US graded compression. Normal appendix seen in this US negative exam ruled out appendicitis. No further imaging was performed.
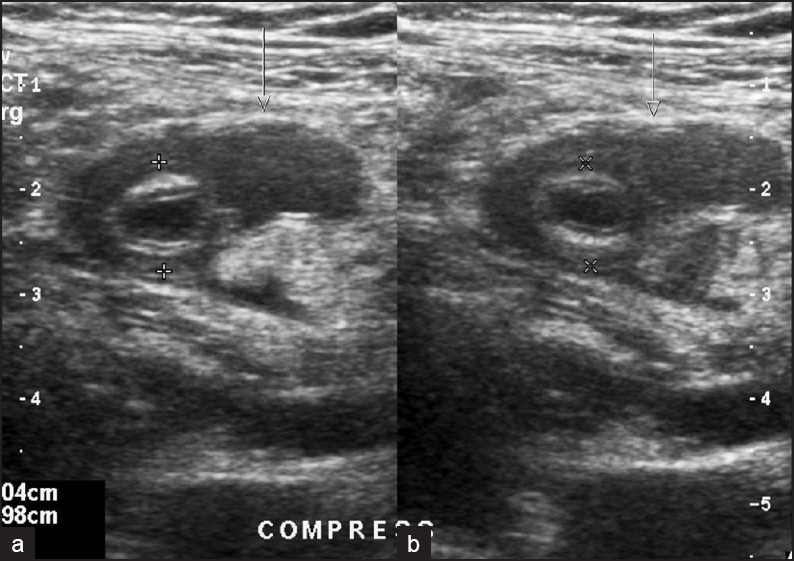
The inflamed appendix is visualized as an incompressible, blind-ended, gut-pattern fluid-filled tubular structure, with a thickened wall, and a diameter greater than 6–7 mm. Applying graded compression with the transducer, differentiation between normal displaceable loops and the fixed inflamed appendix can be achieved.[9]
Color and power Doppler may aid in the diagnosis by showing a hyperemic wall [Figure 2]. Manual compression of the lumbar fossa improves visualization of appendicitis, in particular when it is retrocecal.[10] Visualization of the whole appendix is needed to detect if inflammation is localized just at the end of the appendix, known as “tip” appendicitis. When there is clinical suspicion of appendicitis, the presence of a fecalith in the appendix confirms the diagnosis [Figure 3].[11] Additional findings are pelvic or inter loop peritoneal fluid and hyperechoic inflamed mesenteric fat surrounding the appendix [Figure 4]. Perforated appendicitis may be seen as an abscess in the right lower quadrant [Figure 5]. The inflamed appendix is sometimes hidden by the peri-appendicular abscess. Abscesses may be drained under US guidance [Figure 6]. Appendicitis-mimicking conditions of gastrointestinal and urogenital origin may be revealed on US images of the right lower quadrant [Figure 7].

- A 25- year-old-male with right lower quadrant pains and leukocytosis. Acute appendicitis on US. (a) Gray-scale longitudinal compression US. An incompressible, blind-ended, gut-pattern fluid-filled tubular structure, with thickened wall and diameter greater than 7 mm is seen in the right lower quadrant (arrows). (b) Power Doppler US. A hyperemic wall is demonstrated (arrows). Following diagnosis of acute appendicitis on US examination, patient proceeded to surgery, without further imaging tests.

- A 28-year-old-female with pelvic pains and fever. Tip appendicitis and appendicolith on US. (a) Long axis view of the appendix. A normal proximal appendix, 4.8 mm width followed by enlarged, 12.7 mm width fluid-filled distal appendix is seen on compression US. A hyperechogenic focus with posterior acoustic shadow compatible with a fecalith is seen in the appendix lumen, proximally to the enlarged blinded end. Tip appendicitis with appendicolith was diagnosed and confirmed on surgery. (b) Short axis view of the appendix, showing the normal proximal appendix and the inflamed distal part (measurements), the last containing an appendicolith.

- A 21-year-old-male with right pelvic pain and fever. Mesenteric fat thickening surrounding acute appendicitis on US. Hyperechoic thickened mesenteric fat (arrows) surrounding 9.5 mm inflamed appendix (cursors) is seen on compression US.
- A 10- year-old- female with abdominal pain for three days and rebound in right lower quadrant. Perforated appendicitis on US. Dual gray scale compression US image (right plot before compression; left plot during compression) showing an uncompressible distended appendix (cursors) surrounded by a fluid collection (arrows).

- A 45- year-old-female with fever and abdominal pains, 10 days after laparoscopic appendectomy. Right lower abdomen abscess, drained under US guidance. (a) Contrast enhanced MDCT showing a retrocecal collection displacing the ascending colon (arrows). (b) US of the right lower quadrant demonstrated fluid collection (long arrows) and in the bottom, an echogenic structure with posterior acoustic shadowing (short arrows), compatible with a dropped appendicolith. (c) A 7F pig tail catheter (arrow at the tip) is introduced in the collection under US guidance. (d) The catheter is shown in the partially drained collection (arrow).

- A six-year-old-female with pain in right lower abdomen and pelvis. Alternative diagnosis to appendicitis: ureteral stone and hydronephrosis on US. (a) Longitudinal US scan of the pelvis showing a hyperechoic linear structure with a “twinkle” artifact on color Doppler compatible with a stone, in the right ureter at the uretero vesical junction. Hydroureter is seen proximal to the stone. (b) Transverse scan of the lumbar fossa showing mild hydronephrosis.
Multidetector computed tomography
Several approaches for using CT to diagnose appendicitis were described. They were distinguished by factors including the use of oral or rectal contrast administration of either positive, neutral, or water contrast agents and whether non-contrast or contrast exams after intravenous injection were performed. They also varied in the anatomical extension of the scan, some including the entire abdomen and pelvis and others focusing on the anatomical area, from the level of the xyphoid to the ramus pubis. Modern protocols generally use helical and multidetector CT (MDCT).
The normal appendix is visualized as a blind-ended tubular structure exiting from the cecum, filled with contrast media or gas [Figure 8].[12] The normal diameter ranges between 6 and 10 mm, although more than 7 mm is generally considered as pathological.

- A 10-year-old-male with persistent right lower quadrant abdominal pain and fever, after two negative US exams for appendicitis. Normal appendix on CT. A retrocecal subhepatic blind-ended gas filled tubular structure of normal wall thickness and normal diameter is seen (large arrow). Mesenteric fat infiltration is seen anterior to the cecum (small arrow).
The inflamed appendix is seen as a blind-ended tubular structure exiting from the cecum, without contrast or air filling, more than 7 mm in diameter [Figure 9]. The presence of contrast or air from gas-forming organisms in the proximal part of the lumen does not exclude appendicitis. Additional findings such as the presence of an appendicolith, interloop peritoneal fluid, cecal wall thickening, and periappendicular fat stranding are especially useful in an indeterminate appendix [Figure 10].[13] Administration of intravenous contrast media, as a bolus injection of 80-100 cc non-ionic contrast media, allows evaluation of the appendix wall enhancement, which can be useful in borderline cases.

- A three-year-old-male with abdominal pains and rebound in right lower abdomen. Acute appendicitis on CT, misdiagnosed on US. (a) Gray scale US performed by the resident on-duty showed a structure interpreted as mimicking intussusception in the subhepatic area (arrows). Due to the patient's clinical condition and indeterminate US diagnosis, a CT was performed. (b) Contrast enhanced coronal oblique reformatted MDCT showing a widened fluid filled tubular structure, without intraluminal air, of oral contrast media (arrows), surrounded by infiltrated mesenteric fat, compatible with acute appendicitis.

- A 47-year-old-male with a history of inflammatory bowel disease, presenting with abdominal pain and fever. Acute appendicitis with mesenteric stranding on CT. (a) A blind-ended tubular structure exiting from the cecum, without intraluminal oral contrast media or air, 12 mm in diameter, is seen (large arrow). Mesenteric fat stranding (short arrow) is seen in the proximity of the inflamed appendix. (b) Mesenteric fat edema and reactive lymph nodes are seen in a scan proximal to (a). CT followed a US exam positive for appendicitis, to rule-out signs of active Crohn's disease.
Alternative diagnosis of right lower quadrant pain may be achieved using CT, to determine if it is of gastrointestinal origin, such as mesenteric adenitis, intussusception, terminal ileitis, diverticulitis, epiploic appendagitis, and typhlitis, or of urogenital origin, such as ureteral stone and urinary tract infection, tubo ovarian abscess, ovarian torsion, ectopic pregnancy, hemorrhagic ovarian cyst or corpus luteum remnants [Figures 11 and 12].

- Same patient as in Figure 9. Bowel inflammatory disease on CT in a patient with acute appendicitis. Cecum and terminal ileum with thickened walls (arrows) and adjacent peritoneal fluid (F) confirm Crohn's disease. An appendicolith (lateral right arrow) is seen at the base of the inflamed appendix, (shown in Figure 9).
Magnetic resonance imaging
MRI is an alternative method to CT for pregnant patients, offering high soft tissue contrast without ionizing radiation. The imaging protocol for MRI evaluation of acute appendicitis in the pregnant population includes T1- and T2- weighted images, and has been extensively described in the literature.[1415]
The normal appendix is seen as a tubular structure exiting from the cecum, greater than 7 mm in diameter, filled with air or contrast media [Figure 13].

- A 37- year-old-pregnant patient with lower abdominal pain and fever. Normal appendix on MRI. A normal sized appendix with air into the lumen is seen in the right lower quadrant in this axial T1 weighted with fat suppression image. A previously performed US was negative for appendicitis, but the normal appendix could not be demonstrated.
Acute appendicitis is seen as an enlarged appendix, greater than 7 mm in diameter, and void of air or contrast media. Signs of peri-appendicular inflammation, seen as band-like areas of high signal intensity on T2-weighted images, single-shot fast spin-echo images or fat saturation images, or the presence of an appendicolith, visualized as an intraluminal low signal intensity focus, confirm the diagnosis, especially in the borderline widened appendix [Figure 14].[16–20] According to the American College of Radiology guidelines for safe MRI practices, contrast agents should not be routinely administered to pregnant patients.[21] Routine use of gadolinium-based contrast agents in pregnancy is not approved.

- A 28-year-old-female of 26 weeks pregnancy, presenting with lower abdominal pain and fever. US exam failed to show the appendix. (a) Coronal T2 weighted image showing an enlarged (10 mm in diameter) fluid filled appendix surrounded by a band-like area of high signal intensity (arrow) compatible with appendicitis with periappendicular inflammation. (b) Axial T2 weighted with fat suppression. The inflamed appendix is seen as a tubular fluid filled structure (arrow) in the right lower quadrant, behind the pregnant uterus. On surgery, an inflamed appendix surrounded by purulent fluid was found.
MRI is also useful in identifying alternative sources of right lower quadrant pain in patients suspected of acute appendicitis [Figure 15].

- A 13- year-old-male with a history of Crohn's disease, presenting with right lower abdominal pain. Terminal ileitis on MRI. Axial T2 weighted image after diluted oral contrast media administration, showing the thickened-wall terminal ileum (long arrows) compatible with Crohn's disease. A normal retrocecal appendix is seen (short arrow).
Ultrasound, computed tomography, and magnetic resonance imaging performance in the diagnosis of acute appendicitis
In two previous review studies, US and CT performance for the diagnosis of acute appendicitis were compared.[67] van Randen et al selected six studies performed in adults from 1994 to 2005.[6] The mean sensitivities for CT and graded compression US were 91% and 78% respectively. The respective mean specificities for CT and graded compression US were 90% and 83%. In a head-to-head comparison, CT offered a better test performance than graded compression US in diagnosing appendicitis. Therefore, CT is recommended in patients suspected of acute appendicitis. However, taking into consideration the drawbacks of radiation exposure in young, female and slender patients, graded compression US is recommended as the primary diagnostic test in these patients. Based on 26 studies in children and 31 studies in adults from 1988 to 2004, Doria et al found the pooled sensitivity and specificity for US in the diagnosis of appendicitis in children to be 88% and 94% respectively, and for CT studies, 94% and 95% respectively. The pooled sensitivity and specificity for US studies in the diagnosis of appendicitis in adults were 83% and 93% respectively, and for CT studies, 94% and 94% respectively. CT had a significantly higher sensitivity than US in both children and adults. However, the drawbacks of radiation exposure associated with CT should be considered, especially in children.[7] Methodological shortcomings in both of these studies, however, could influence reported diagnostic test accuracy.
In our present review, we selected studies performed from February 2006 to March 2011 comparing graded compression US and CT performance, using surgery or clinical follow-up as the standard reference. The results are presented in Table 1.
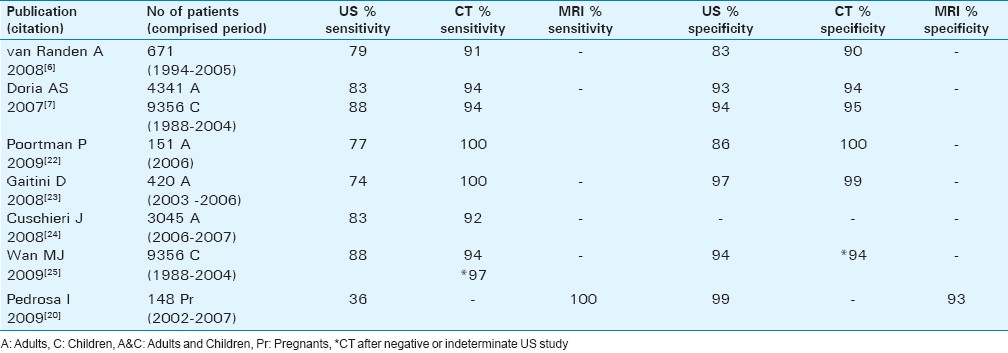
Poortman et al developed an imaging diagnostic pathway using US as the primary test.[22] Contrast-enhanced MDCT was complementary to a negative or inconclusive US study. Of a total population of 151 adult patients suspected of appendicitis, 79 patients diagnosed by US as positive for appendicitis were directed to appendectomy and 72 negative or inconclusive patients diagnosed by US proceeded to MDCT. Appendicitis was diagnosed by CT in 21 patients. An alternative diagnosis was made in 12 patients and no source of abdominal pain was found in 39 patients. In this study, the sensitivity and specificity for CT were 100%, and for US, 77% and 86% respectively. The described strategy yielded a negative appendectomy rate of 8%. Although less accurate than CT, US can be used as a primary diagnostic modality avoiding the disadvantages of CT.
Gaitini et al conducted a retrospective study to evaluate the diagnostic accuracy of color Doppler US and contrast-enhanced MDCT in 420 adult patients referred from the emergency room with clinical suspicion of appendicitis.[23] All the patients underwent graded compression US and color Doppler of the right lower quadrant. CT was performed in 132 patients due to inconclusive sonographic findings or a discrepancy between clinical and sonographic diagnoses. Sonography and CT correctly diagnosed acute appendicitis in 66 of 75 patients and in 38 of 39 patients, respectively, and correctly ruled out acute appendicitis in 312 of 326 and in 92 of 92 patients. Sonography was inconclusive in 17 of 418 cases and CT, in one of 132 cases. Sonography and CT allowed alternative diagnoses in 82 and 42 patients, respectively. The sensitivity and specificity of US were 74% and 97% respectively, with a 93% negative predictive value, while CT had a sensitivity and specificity of 100 %and 99% respectively, with a 100% negative predictive value . The positive predictive value and accuracy for sonography were 88% and 92% and for CT, 97% and 99%. Due to its high negative predictive value (93%), US should be used as the first imaging test in adult patients for the diagnosis of appendicitis and triage of acute abdominal pain, reserving CT as a complementary study for selected cases.
Cuschieri et al, of the Surgical Care and Outcomes Assessment Program (SCOAP) collaborative group evaluated the relationship between negative appendectomies (NA) and negative CT/US over a two year period (2006–2007).[24] The number of patients who underwent urgent appendectomies was 3540. The percentage of patients who underwent imaging as part of their diagnosis was 86%. Agreement between imaging and pathology findings was 92.3% for CT and 82.4% for US. There was a significant increase in the use of CT/US and decrease in NA over the study period (P < .0001). Variation between hospitals was linked closely to CT/US accuracy, suggesting that CT/US accuracy should be considered a measure of quality in the care of patients with presumed appendicitis.
US is widely used for the diagnosis of appendicitis in pediatric patients due to concerns regarding risks from exposure to ionizing radiation. In a recent paper, Wan et al analyzed cost-effectiveness of US versus CT in young children based on a decision analytic model using costs, utilities and probabilities.[25] US was the least costly but least effective strategy. US followed by CT was the most costly but most effective strategy. The most cost-effective method was to start with a US study and follow negative US studies with a CT examination. This strategy is in concordance with the previously published study of Garcia Pena et al.[26]
Pregnant patients present a special population, and clinical and laboratory findings lack specificity for the diagnosis of appendicitis in pregnancy. An unnecessary laparotomy increases the risk of pre-term contractions, while delay in the treatment of appendicitis leading to perforation increases fetal mortality to 6–37%.[45] Pedrosa et al investigated the role of MRI in 148 pregnant patients suspected of appendicitis in lowering the negative laparotomy rate (NLR) and the perforation rate (PR).[20] US was performed before MRI in 140 patients. An oral contrast media was administrated to facilitate identification of the appendix in MRI examinations. US had a low sensitivity (36%) but an excellent specificity (99%). The sensitivity and specificity of MRI were 100% and 99% respectively. Among the patients with a negative diagnosis for appendicitis, the normal appendix could be visualized on US in less than 2% (2 of 126) of cases and on MR in 87% (116 of 134) of cases (P < .0001). The use of MR imaging yields favorable combinations of NLR and PR compared with values previously reported in the literature. With MR imaging, the radiation exposure associated with CT examinations is avoided.
Ultrasound, computed tomography and magnetic resonance imaging: Advantages and disadvantages
A comparison of methods for imaging appendicitis is presented in Table 2.

The main advantage of US over CT is the lack of ionizing radiation, which is most important in the pediatric and young adult populations, among which appendicitis occurs more frequently, and who are most vulnerable to radiation's detrimental effects.[27–31]
In the pediatric population, US also obviates the need for sedation or general anesthesia. US may be considered as an extension of the physical examination: patients can point to the region of tenderness and graded compression US may elicit a rebound with an increased sensation of pain. Contrast media ingestion, with a consequent delay in surgery, or contrast injection, carrying risks of allergic reaction and nephrotoxicity, are not required for US examinations. US may not only diagnose an abscess or phlegmon in perforated appendicitis but can also guide percutaneous drainage. Several alternative conditions, especially in the female pelvis, may be diagnosed on US examination.[2–4]
The main disadvantage of US is its operator dependence. US success depends on the knowledge, skill, and patience of the examiner.[3233] US has a lower sensitivity compared to CT for the diagnosis of appendicitis.[6722–2433] However, with a high prevalence of the disease and a strict protocol, a sensitivity and specificity of 98.5% and 98.2% respectively was achieved for the US diagnosis of appendicitis in children.[31] The inability of US to properly scan a gas distended bowel or an obese patient, and lack of demonstration of a normal appendix, especially when retrocecal or deeply situated in the pelvis, may lead to indeterminate or false negative exams. In pregnant patients, identification of the appendix using compression US is more difficult to achieve.[4520]
The main advantage of CT for the diagnosis of appendicitis is its high sensitivity and specificity [Table 1].[32–34] Marked advancements in CT technology over the last decade have led to excellent image quality.
The main disadvantage of CT is the radiation exposure, especially important in the radiosensitive pediatric and young adult appendicitis-suspected population.[3536] Allergic reaction and nephrotoxicity risks of iodinated contrast media injection, delay in the diagnosis and therapy due to time invested in ingestion of contrast media, higher cost and lower availability, particularly in small or peripheral centers, are further disadvantages of CT. Operator dependence related to CT protocols and radiologist skills for correct performance and interpretation are also limitations of CT exams.[33]
The main advantage of MRI in pregnant patients is in avoiding radiation exposure to the fetus. MRI is less operator-dependent than US, lacks exposure to intravenous iodinated contrast media, and may afford alternative diagnoses, such as ovarian torsion or renal obstruction.[2037–39]
MRI disadvantages reside in a longer examination time, limitations related to claustrophobia and metal devices, low availability, and higher cost.
Ultrasound, computed tomography or magnetic resonance imaging for the diagnosis of acute appendicitis?
Guidelines for the diagnosis of appendicitis are needed, related to choosing which is the optimal patient-tailored imaging modality to begin with, and an algorithm for further imaging procedures, if required. According to the present review, imaging of a patient of any age suspected of appendicitis should start with a graded compression US examination. A positive, good-quality US when there is a strong clinical suspicion is enough to proceed to surgery. A negative US exam for appendicitis, where the normal appendix is clearly visualized, or alternatively, when the appendix is not seen but the clinical suspicion for appendicitis is low, may end the investigation, leading to patient discharge or follow-up. Furthermore, if an alternative diagnosis for the clinical presentation is reached, treatment of the alternative condition will be followed. A negative or indeterminate US exam in a non-pregnant adult with a high clinical suspicion of appendicitis must be followed by CT. In pregnant patients, a negative US with a high suspicion for appendicitis should lead to an MRI examination.[38–40] [Figure 16]. In the pediatric patient, a second US examination, especially when the first was performed by a less experienced professional, may render definitive results, while avoiding CT radiation risks.

- Imaging strategy for the diagnosis of acute appendicitis. Imaging should start by graded compression US. A positive US is enough to proceed to surgery or percutaneous drainage of a peri-appendicular abscess A negative US showing the normal appendix may end the investigation and lead to patient discharge. An indeterminate US, whether neither the normal nor the inflamed appendix is seen may lead to follow up or a repeated US if the clinical suspicion is low. CT or MRI in pregnant must be performed when the clinical suspicion is high. An alternative condition should be treated accordingly.
This approach seems to offer excellent accuracy, with reported sensitivities of 94% to 99% and specificities of 94% to 95%.[732]
CONCLUSION
Imaging is increasingly important in the diagnosis and management of appendicitis, avoiding unnecessary interventions and delay in treatment that may lead to perforation. US and CT are not competitive but complimentary modalities. US may be accepted as sufficiently accurate for clinical decision making. US findings must be considered in conjunction with the clinical evaluation. If these guidelines are followed, the number of CT examinations performed will be considerably reduced. Clinical guidelines defining the use of each particular imaging modality allow uniformity, a targeted approach for different patient populations, and cost-effectiveness of medical services.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/49/85778
REFERENCES
- Appendix. In: Townsend CM Jr, Mattox KL, Evers BM, eds. Sabiston Textbook of Surgery (17th ed). New York NY: Saunders; 2004. p. :1381-95.
- [Google Scholar]
- Mimics of appendicitis: Alternative nonsurgical diagnoses with sonography and CT. AJR Am J Roentenol. 2006;186:1103-12.
- [Google Scholar]
- Imaging in appendicitis: A review with special emphasis on the treatment of women. Obstet Gynecol. 2003;102:1404-9.
- [Google Scholar]
- Acute appendicitis: Meta-analysis of diagnostic performance of CT and graded compression US related to prevalence of disease. Radiology. 2008;249:97-106.
- [Google Scholar]
- US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology. 2006;241:83-94.
- [Google Scholar]
- Sonographic appearance of the normal appendix in adults. J Ultrasound Med. 2007;27:37-43.
- [Google Scholar]
- Acute appendicitis: US evaluation using graded compression. Radiology. 1986;158:355-60.
- [Google Scholar]
- Graded compression sonography with adjuvant use of a posterior manual compression technique in the sonographic diagnosis of acute appendicitis. AJR Am J Roentenol. 2002;178:863-8.
- [Google Scholar]
- Periappendiceal hyperechoic structure on sonography: A sign of severe appendicitis. J Ultrasound Med. 2005;24:323-32.
- [Google Scholar]
- Incidence of visualization of the normal appendix on different MRI sequences. Emerg Radiol. 2006;12:223-6.
- [Google Scholar]
- Localization of the appendix at MR imaging during pregnancy: Utility of the cecal tilt angle. Radiology. 2008;249:134-41.
- [Google Scholar]
- Diagnosis of acute appendicitis during pregnancy: A systematic review. Obstet Gynecol Surv. 2009;64:481-8.
- [Google Scholar]
- MR imaging evaluation of acute appendicitis in pregnancy. Radiology. 2006;238:891-9.
- [Google Scholar]
- Right-lower-quadrant pain and suspected appendicitis in pregnant women: Evaluation with MR imaging—initial experience. Radiology. 2005;234:445-51.
- [Google Scholar]
- MR imaging of acute right lower quadrant pain in pregnant and nonpregnant patients. RadioGraphics. 2007;27:721-43. discussion on 743-53
- [Google Scholar]
- Pregnant patients suspected of having acute appendicitis: Effect of MR imaging on negative laparotomy rate and appendiceal perforation rate. Radiology. 2009;250:749-57.
- [Google Scholar]
- ACR guidance document for safe MR practices: 2007. AJR Am J Roentenol. 2007;188:1447-74.
- [Google Scholar]
- Improving diagnosis of acute appendicitis: Results of a diagnostic pathway with standard use of ultrasonography followed by selective use of CT. J Am Coll Surg. 2009;208:434-41.
- [Google Scholar]
- Diagnosing acute appendicitis in adults: Accuracy of color Doppler sonography and MDCT compared with surgery and clinical follow-up. AJR Am J Roentenol. 2008;190:1300-6.
- [Google Scholar]
- The SCOAP Collaborative.Negative appendectomy and imaging accuracy in the Washington State surgical care and outcomes assessment program. Ann Surg. 2008;248:557-63.
- [Google Scholar]
- Acute appendicitis in young children: Cost-effectiveness of US versus CT in diagnosis-a Markov decision analytic model. Radiology. 2009;250:378-86.
- [Google Scholar]
- Ultrasonography and limited computed tomography in the diagnosis and management of appendicitis in children. JAMA. 1999;282:1041-6.
- [Google Scholar]
- Appendicitis in children: One radiologist's perspective. Pediatric Radiol. 2007;37:1-3.
- [Google Scholar]
- The role of imaging in children with suspected appendicitis: The UK perspective. Pediatr Radiol. 2007;37:5-9.
- [Google Scholar]
- Clinical approach to a child with abdominal pain who might have appendicitis. Pediatr Radiol. 2007;37:11-4.
- [Google Scholar]
- Accuracy of noncompressive sonography of children with appendicitis according to the potential positions of the appendix. AJR Am J Roentenol. 2000;175:1387-92.
- [Google Scholar]
- CT and US in the diagnosis of appendicitis: An argument for CT. Radiology. 2010;255:3-7.
- [Google Scholar]
- Effect of CT on false positive diagnosis of appendicitis and perforation. N Engl J Med. 2008;358:972-3.
- [Google Scholar]
- Computed tomography: An increasing source of radiation exposure. N Engl J Med. 2007;357:2277-84.
- [Google Scholar]
- Radiation dose to the fetus from body MDCT during early gestation. AJR Am J Roentenol. 2006;186:871-6.
- [Google Scholar]
- Imaging strategies for right lower quadrant pain in pregnancy. AJR Am J Roentenol. 2011;196:4-12.
- [Google Scholar]
- Right-lower-quadrant pain and suspected appendicitis in pregnant women: Evaluation with MR imaging-initial experience. Radiology. 2005;234:445-51.
- [Google Scholar]
- Acute appendicitis: MR imaging and sonographic correlation. AJR Am J Roentgenol. 1997;168:669-74.
- [Google Scholar]







