Translate this page into:
Imaging Findings in Chiari I Malformation with Syringomyelia in a Case of Charcot Shoulder
Address for correspondence: Dr. Shantanu Kumar, Department of Orthopaedic Surgery, Lucknow, Uttar Pradesh, India E-mail: kshantanu82@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Neuropathic arthropathy of the shoulder is reported in only 5% of cases. Here, we report a rare case of neuropathic arthropathy of the shoulder, secondary to Chiari malformation Type I with associated syringomyelia, that remained undetected for four years. A 38-year-old female presented to our Department with a swelling over the right shoulder that had persisted for four years. X-ray of the joint showed destruction of the head of the right humerus, with typical blunt amputated appearance of the bone and increased joint space. Magnetic resonance imaging showed destruction and lateral dislocation of the head of the humerus. Large amount of fluid collection was seen in and around the right shoulder joint. Neuropathic osteoarthropathy can be defined as bone and joint changes that occurs secondary to loss of sensation. In our case, neuropathic shoulder joint was secondary to syringomyelia associated with Chiari I malformation.
Keywords
Charcot
Chiari malformation
shoulder
syringomyelia
INTRODUCTION

Neuropathic joints, often called Charcot joints, are a chronic form of degenerative arthropathy caused by a loss of sensation in the joint such that the joint is severely damaged and disrupted. Typical imaging features include joint destruction, disorganization, and effusion with osseous debris. Resorption of the ends of tubular bones and neuropathic fractures are also associated findings. Charcot joints are more commonly seen in the lower limb. Previously, Tabes dorsalis was a common cause, affecting the hip and knee joints; however, this is much rarer these days. The more common cause in the present times is diabetic neuropathy, which involves ankle and foot joints. In the upper limb the classical cause is syringomyelia. Neuropathic arthropathy of the shoulder is reported in only 5% of cases.[1] Here we report a rare case of neuropathic arthropathy of shoulder, secondary to Arnold-Chiari Type I malformation with associated syringomyelia, that was undetected for four years.
CASE REPORT
A 38-year-old female with a swelling over the right shoulder was referred to the Department of Orthopaedics. The swelling had been present for four years and was attributed to be the result of a fall. On examination, shoulder movements were restricted. Swelling was firm to hard, non-tender, associated with mild pain, with normal temperature, and diminished sensation. The patient had no history of diabetes mellitus or any other long standing disease. The patient had been treated with massage and manipulation of the shoulder by a local doctor in the village.
Radiograph done four years ago after the trauma revealed dislocation of the shoulder. The patient had no other X-rays with her. In the meanwhile, she had been treated with massage and physiotherapy continuously for a period of two years in her village, as advised by a local doctor. The symptoms got aggravated and she was referred to the medical college for further management. A repeat X-ray was done that showed destruction of the head of the right humerus leading to its typical blunt amputated appearance and increased joint space [Figure 1]. The proximal right humerus and glenoid cavity were sclerosed and the proximal humerus was subluxated superiorly. Multiple bony fragments were seen in the soft tissues around the right shoulder joint with displacement of adjacent fat planes.

- Radiograph of the right shoulder AP view showing destruction of the head of the humerus giving rise to its blunted amputated appearance and increased joint space. The proximal right humerus and glenoid cavity are sclerosed and the proximal humerus is subluxated superiorly. Multiple bony fragments are seen in the soft tissues around the right shoulder joint.
Magnetic resonance imaging (MRI) showed destruction and lateral dislocation of the head of the humerus [Figure 2]. Residual humerus was subluxated superiorly with sharp margins. A large quantity of fluid collection was seen in and around the right shoulder joint. Bony fragments and debris were seen within the collection. Tear and atrophy of muscles around the shoulder joint, namely the supraspinatous, infraspinatous, and subsapularis muscles were seen. Glenoid cavity was shallow and showed destructive changes.
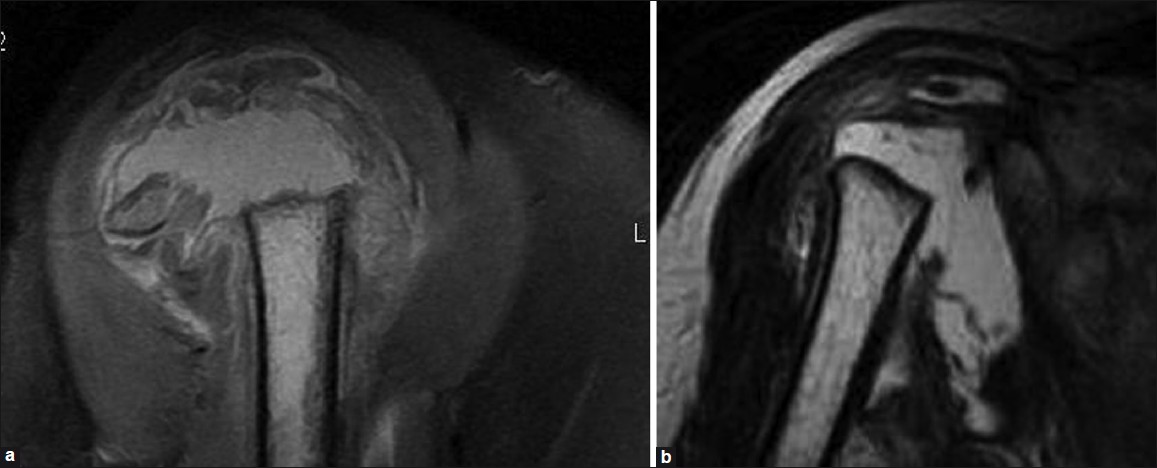
- MRI of right shoulder. (a) Sagittal proton density fat suppressed image showing destruction of the head of the humerus with sharp margins and large amount of joint effusion. (b) Coronal T2 weighted image showing superior subluxation of the head of the humerus with multiple bony fragments. Destruction of surrounding muscles is also noted.
MRI of cervico-dorsal spine showed syrinx formation with herniation of cerebellar tonsils (6mm) into foramen of magnum leading to foraminal stenosis consistent with the diagnosis of Chiari malformation Type I [Figure 3].
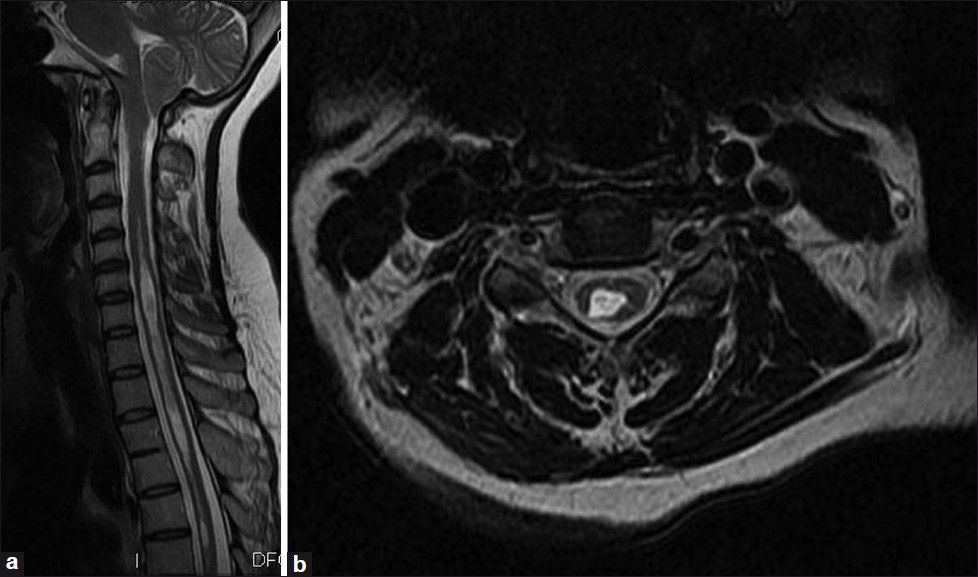
- MRI of cervico-dorsal spine. (a) Sagittal T2 weighted image showing herniation of cerebellar tonsils with syrinx in visualized spinal cord. (b) Axial T2 weighted image showing syrinx formation in spinal cord.
Treatment consisted of non-steroidal anti-inflammatory medication, passive motion exercises, and a protective sling. The patient with syringomyelia may experience sensory loss that prevents normal guarding, resulting in repetitive trauma and eventual joint destruction. Further the patient was referred to a neurosurgeon, who also preferred conservative treatment as the patient was not having any major neurological symptoms. Patient education is equally important to minimize the stress and inadverent trauma.
DISCUSSION
Neuropathic joint arthropathy, otherwise known as the Charcot joint was initially described by Mitchell in 1831 and later named after Jean-Martin Charcot in 1868.[23]
Neuropathic osteoarthropathy can be defined as bone and joint changes that occurs secondary to loss of sensation and that accompanies a variety of disorders. The Charcot joint is characterized by slow progression over many years (but rapid progression occurring over months has also been described).[4]
Common causes of neuropathic arthropathy include diabetes, use of steroids, alcoholism, trauma, infection, amyloidosis, pernicious anaemia, syphilis, syringomyelia, spina bifida, myelomeningocele, and leprosy. In diabetic neuropathy, common sites of involvement are the metatarsophalangeal, tarsometatarsal, and intertarsal joints. In syringomyelia, neuropathic changes are relatively more common in the shoulder joint, followed by the elbow and wrist.[5] The lower extremities can also be affected in syringomyelia. Changes in the spine are most characteristic in the cervical region. The joints of the lower extremity are commonly affected in patients with Tabes dorsalis.
Although for long there has been, recognition of the association between syringomyelia and neuropathic arthropathy,[26] the pathogenesis has remained controversial. Charcot and Mitchell[6] believed the underlying mechanism to result from damage to the CNS trophic centres that controlled bone and joint nutrition. This concept became known as the “French theory”. Volkmann and Virchow violently disputed this concept and espoused the “German theory”. Postulating that the neuropathic joint resulted from the accumulation of years of subclinical trauma that went unnoticed by the individual because of an insensate joint.[2] In 1981, Brower and Aliman[2] studied 91 patients with neuropathic joint arthropathy; 32% had joint pain without any known neurologic disease. Four of their patients were bedridden when neuropathic arthropathy developed. They argued that the absence of weight bearing capacity and repeated joint trauma in these immobilized patients disputed a traumatic etiopathogenesis for neuropathic arthropathy and postulated a neurovascular mechanism (first espoused by Leriche in 1927).[2] According to this, a neurally mediated vascular reflex secondary to impairment of sympathetic vascular modulation leads to increased bone blood flow. Concomitant with this increased blood flow is increased active reabsorption of bone by osteoclasts, with fracture and joint damage occurring as a secondary epiphenomenon, depending on the degree of weight bearing and sensory impairment affecting the involved joint.
Neuropathic arthropathy comprises of both hypertrophic and atrophic patterns which can be discerned radiologically.[7] The classically described hypertrophic joint is manifested radiologically as joint destruction and fragmentation, osseus sclerosis, and osteophyte formation. The six D's of neuropathic joint include distension of joint, increased density, debris, destruction of articular surface, dislocation, and disorganization of joint.[8] Periarticular bone fragments are as characteristic of neuropathic joints as is the propensity to rapid disintegration. Osteophytes formed in the setting of neuropathic arthropathy may differ from those of osteoarthritis on the basis of early production of ill-defined and rounded margins and later attainment of enormous size.
Atrophic form of neuroarthropathy has an appearance of osseous resorption that often gives the impression of surgical amputation. Joint disorganization and large persistent bloody joint effusion are features of both atrophic and hypertrophic types of neuroarthropathy.
Hans Chiari first described Chiari Type I malformations as elongation of the tonsils and medial divisions of the inferior lobules of the cerebellum into cone-shaped projections that accompany the medulla oblongata into the spinal canal.[9] Its incidence has been found to be between 0.56%[6] - 0.77%[10] on MRI studies, and 0.62% in brain dissection studies.[11]
The radiological criteria for Chiari malformation in pre MRI era were based on myelography. MRI has now become the investigation of choice for evaluating such cases. Mikulis et al,[12] found that the cerebellar tonsils ascend with increasing age and suggested the following criteria for ectopia: First decade, 6 mm below the foramen magnum; second to third decades, 5 mm; fourth to eighth decades, 4 mm; and ninth decade, 3 mm below the foramen magnum. Narrowing or complete effacement of the CSF spaces of the foramen magnum and cisterna magna were documented in all symptomatic patients. In the above case with only 6mm tonsillar herniation, effacement of CSF cisterns and syringomyelia was responsible for emergence of symptoms.
Newer imaging techniques like cine phase contrast MRI have been introduced to diagnose CSF flow obstruction in patients with Chiari malformation. It was first reported in 1991 by Tominaga et al.[13] CSF flow analysis through foramen magnum helps distinguish symptomatic Chiari I from asymptomatic cerebellar ectopia and helps predict response to surgical decompression. In Chiari patients, cine phase-contrast MRI detected the abnormal pulsatile motion of the cerebellar tonsils, which produced a selective obstruction of CSF flow from the cranial cavity to the spine. The amplitude of the tonsillar pulsation and the severity of the arachnoid space reduction were associated with the symptoms.
In our case, neuropathic shoulder joint was secondary to syringomyelia associated with Arnold -Chiari malformation. This is a less common entity, reported in only 5% cases; it has been described in fewer than 60 patients worldwide.[1] Syrinxes interrupt the decussating fibers of the lateral spinothalamic tracts that mediate pain and temperature sense.[1415]
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/46/85173
REFERENCES
- Shoulder arthropathy (Charcot joint) and syringomyelia: Report of two patients. 2005. Eur J Orthop Sur Traumatol. 15:37-41. [http://www.springerlink.com/content/?k=Mazlout+O%2c+Larnaout+A%2c+El+Mufti+T%2c+et+al.+Shoulder+arthropathy+%28Charcot+joint%29+and+syringomyelia%3a+Report+of+two+patients.+Eur+J+Orthop+Sur+Traumatol+2005%3b15%3a37-41]
- [Google Scholar]
- Pathogenesis of the neuropathic joint: Neurotraumatic versus neurovascular. Radiology. 1981;139:349-54.
- [Google Scholar]
- Neuropathic joint disease (Charcot joints) In: McCarty DJ, ed. Arthritis and allied conditions: A textbook of rheumatology (11th ed). Boston: Lea and Feibiger; 1989. p. :1255-9.
- [Google Scholar]
- Neuropathic arthropathy of the shoulder, a case report. Orthopedics. 1988;11:301-4.
- [Google Scholar]
- Charcot shoulder caused by Chiari type I malformation with syringomyelia with six-year follow-up. Wien Klin Wochenschr 2011
- [Google Scholar]
- Neuropathic arthropathy as a complication of post-traumatic syringomyelia. Br J Radiol. 1987;60:702-4.
- [Google Scholar]
- Radiological quiz - musculoskeletal. 2005. Indian J Imaging. 15:287-9. [http://www.ijri.org/article.asp?issn=0971-3026;year=2005;volume=15;issue=2;spage=287;epage=289;aulast=Gothi]
- [Google Scholar]
- Neuropathic arthropathy progressing with multiple joint involvement in the upper extremity due to syringomyelia and type I Arnold-Chiari malformation. Rhematol Int. 2010;30:979-83.
- [Google Scholar]
- Chiari I malformations: Clinical and radiologic reappraisal. Radiology. 1992;183:347-53.
- [Google Scholar]
- Asymptomatic Chiari Type I malformations identified on magnetic resonance imaging. J Neurosurg. 2000;92:920-6.
- [Google Scholar]
- Variance of the position of the cerebellar tonsils with age: Preliminary report. Radiology. 1992;183:725-8.
- [Google Scholar]
- Transoral decompression evaluated by cine-mode magnetic resonance imaging: A case of basilar impression accompanied by Chiari malformation. Neurosurgery. 1991;28:883-5.
- [Google Scholar]






