Translate this page into:
The Fetal Magnetic Resonance Imaging Experience in a Large Community Medical Center
Address for correspondence: Dr. Peter M. Ghobrial, Department of Radiology, Baystate Medical Center, 759 Chestnut St., Springfield, Massachusetts 01199, USA. E-mail: peter.ghobrial@bhs.org
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Fetal magnetic resonance imaging (MRI) continues to prove a useful problem solving tool for diagnostic and management decision making issues encountered in the antenatal period. In this paper, we attempt to review basic fetal MRI protocol considerations and demonstrate key imaging findings through multiple modalities, with pathologic correlation in several cases. A study of five fetal MRI cases, from our institution, were selected in order to highlight both the indications for, and benefits obtained from this advanced imaging technique. Fetal MRI proved useful in each case in better defining fetal anomalies, especially where ultrasound (due to drawbacks such as shadowing by pelvic bones) was unable to be completely diagnostic. The more in-depth study made possible by MRI also helped with formulation of disease prognosis and estimation of survival chances of the fetus. Further, MRI as a diagnostic and prognostic tool has become more ubiquitous across the medical community. This imparts tangible benefit to patients, who are now able to find this service within arm's reach. Whereas previously these patients were obligatorily referred up to 90 miles away from our centre for further medical work-up, now a large percentage can obtain their prenatal imaging and perinatal care locally. In addition, medical education benefits as new types of cases, those with pathology of the antenatal period, are retained for work-up and management in these large community settings. Cases from our institution exemplify these types of pathologies, from fetal chest masses to a syndromic presentation of bilateral renal agenesis.
Keywords
Bifid Nose, Anorectal and Renal anomalies syndrome
community radiology
fetal magnetic resonance imaging
INTRODUCTION

Fetal Magnetic Resonance Imaging (MRI) is an important problem solving and decision making tool utilized in the work-up of antenatal pathology identified on screening obstetric ultrasonography. Pathology in question can be better defined in many instances; additional pathology may also be identified which was not seen initially, thus aiding better management and decision making.[1] When it was first used in early 1980's, application of this modality had been limited to a narrow scope of practice, with use primarily restricted to the domain of large academic centers. However, in the recent 25 years, advances in MRI technology have allowed for expansion of the list of indications for fetal imaging. Coupled with the growing access to MR scanners throughout communities, fetal MRI evaluation is increasingly available to more patients, especially those who depend on smaller, community medical centers.[1] Fetal imaging can be done closer to patient's homes and families without the need for referral to larger urban centers.
Graduate Medical Education programs’ also benefit from this growing availability of MRI. With the retention of cases involving fetal pathologies in the community setting, resident physicians in radiology, obstetrics and gynecology, pediatrics, surgery, anesthesia, and pathology are gaining valuable experience, which previously was only enjoyed by residents at university centers. This pictorial essay is the outcome of the benefits of such patient retention. The following cases demonstrate the spectrum of pathology we have encountered in the short time since starting our fetal MR program in 2006. Correlative imaging from other modalities, in addition to gross pathology in many instances, supports the breadth of such educational opportunity.
DISCUSSION
The advent of ultrafast sequences has allowed for the expansion of fetal imaging indications since its first use in 1983, from investigation of primarily maternal obstetric concerns (i.e. placental pathology), to routine evaluation of fetal anomalies when additional information is needed to supplement or clarify findings detected with obstetric ultrasonography. Although the most common indication for fetal MR remains assessment of central nervous system (CNS) anomalies, fetal MRI also plays an important role in evaluating anomalies of the fetal chest and abdomen.[12] It is important to point out that fetal MRI studies are best performed in conjunction with obstetric ultrasonogram.[3] The cost-effectiveness, wide availability, efficacy, and safety maintains ultrasound as an ideal screening examination for the second trimester fetus.[4] At present, there is no indication for fetal MRI as a replacement for the screening second trimester anatomic survey. Indications to perform fetal MRI often result from incomplete ultrasound assessment and/or due to disadvantages inherent to evaluation by ultrasonography, especially where shadowing from fetal bony structures is concerned. Such modality limitations may necessitate adjunctive MRI evaluation in complex cases to confirm or complete ultrasound-findings (CNS Syndromes), to guide management of pregnancy, or to plan intrauterine interventions (e.g. diaphragmatic hernia repair), delivery, and postnatal care.
Ultrafast single slice acquisition in MRI minimizes fetal motion artifact, improving the image quality while eliminating the need for fetal-maternal sedation.[3] Fetal MRI at our institution is performed on either a Siemens Espree or Symphony MRI Scanner (Siemens Medical Solutions USA, Malvern, PA) at 1.5 Tesla. Sequences are monitored in real time by the radiologist at the scanner, and manipulated to determine optimal imaging planes during the scan, as fetal orientation is unpredictable and often changes during acquisitions.[1] T2 weighted half-fourier acquisition single-shot turbo spin-echo (HASTE,TR/TE 1500/60 ms, 4mm slice thickness) sequences are obtained in the axial, coronal, and sagittal planes with respect to the fetus. This sequence is primarily suited for assessment of fetal anatomy and pathology. Also, an ultrafast T1 weighted gradient echo sequence (T1 VIBE, TR/TE 4.4/2.5 ms, 4mm slice thickness) is obtained in the axial plane for potential identification of certain stages of hemorrhage, calcification, meconium, or fat.
The American College of Radiology (ACR) White Paper on MR Safety stipulates that MR examinations can be conducted at any point during gestation. However, the information to be obtained should be of such pertinence to maternal/fetal care, that waiting until after pregnancy would be inappropriate and that other non-ionizing imaging modalities would not provide such information.[5] It is preferable to wait until at least gestational week 20 in order to minimize the difficulties created by the small size and excessive motion of the fetus at this stage. Further, there is currently no role for intravenous gadolinium contrast administration in MRI evaluation of the fetus. Gadolinium chelates have been shown to cross the placenta; they appear in the fetal bladder and are thus reabsorbed from the amniotic fluid by fetal swallowing, effectively extending the circulation half-life.[6] The effects of gadolinium chelates on the developing fetus have not been assessed, making the risk for toxicity related sequelae (i.e. nephrogenic systemic fibrosis (NSF)) undefined.[16]
Case 1: 24-year-old female after 19 weeks of gestation
The patient was referred for Fetal MR after screening ultrasound showed anhydramnios, a single umbilical artery and non-visualization of the kidneys and urinary bladder [Figure 1a–c]. Because the lack of amniotic fluid limited the acoustic window for fetal US, MRI was requested to confirm suspected renal agenesis. Fetal MRI was performed two weeks later at 21 weeks of gestation and confirmed the findings [Figure 2a–b]. Labor was induced at 21 weeks on confirmation of bilateral renal agenesis. At gross autopsy [Figures 3–6], the constellation of multiple malformations suggested a case of Bifid Nose, Anorectal, and Renal anomalies (BNAR) Syndrome. BNAR Syndrome is an autosomal recessive syndrome, initially described in a consanguineous union of Egyptian cousins in the United Arab Emirates.[78] Four children were born to this union with similar constellation of features. Given a lack of history of consanguinity in our case, consideration is given for a spontaneous occurrence of this rare syndrome.

- In case 1 of the study, screening prenatal ultrasound evaluation performed at 19 weeks gestation shows (a) anhydramnios on four quadrant survey of the gestational sac (RU, right upper; LU, left upper; RL, right lower; LL, left lower). (b) The aorta (arrow) is seen at the level of the renal arteries on power Doppler interrogation, though neither renal arteries nor kidneys are seen in the area of the renal fossae (arrowheads). (c) A single uterine artery (SUA) (arrow) and absence of the bladder noted on pelvic grayscale and power Doppler evaluation

- In case 1 of the study, (a, b) T2 HASTE MRI images of the fetus confirm anhydramnios and nonvisualization of kidneys or urinary bladder.

- In case 1 of the study, the abdominal cavity is open with spleen and colon moved aside to display empty renal fossae (arrows)

- In case 1 of the study, the face demonstrates a depressed nasal bridge with bifid tip (arrow).

- In case 1 of the study, ambiguous external genitalia are seen with a prominent genital tubercle (arrow), a smooth perineum, and no evidence of vulvar or scrotal structures. Imperforate anus is also noted.

- In case 1 of the study, the large bowel contains a blind ending colonic duplication (arrow).
Case 2: 31-year-old female after 18 weeks of gestation
Screening ultrasonogram demonstrated findings consistent with Congenital Diaphragmatic Hernia (CDH). The stomach was seen within the left hemithorax posterior to the heart, displacing the heart into the right thorax. [Figure 7a–b]. Fetal MR, performed 10 days later, was ordered to assist with prognostication and treatment planning for the perinatal period. MRI confirmed the abnormal gastric position in the chest with rightward cardiac displacement [Figure 8a–b]. However, of greater importance on the MRI was the finding of liver herniation into the left chest [Figure 8c]. As a result of a congenital defect in diaphragmatic closure, varied severity of lung hypoplasia can be seen, dependent upon the extent of abdominal content herniation into the thoracic cavity. As in this case, Fetal MRI can compliment ultrasound findings, differentiate herniated small and large bowel loops from other cystic lung masses, and add additional information important in predicting outcome of infants born with CDH. As with ultrasound, abnormally low lung-to-head ratio correlates with worse outcome. Fetal lung volumes measured by MR have also been shown helpful in predicting survival. Identification of liver herniation through the diaphragmatic defect and the delineation of other anatomic anomalies in addition to CDH also portend worse prognosis.[9]
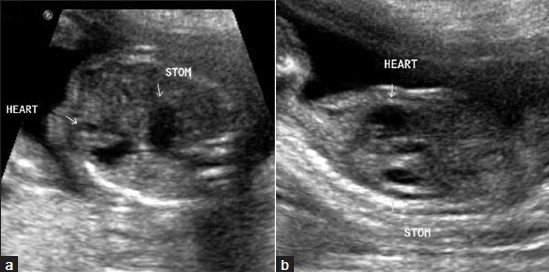
- In case 2 of the study, prenatal ultrasonographic screening exam from 18 weeks gestation demonstrates the stomach at the same level as the heart within the chest both (a) axially and (b) sagittally with respect to the fetus (STOM, stomach). Rightward cardiac displacement is emphasized on the axial image.

- In case 2 of the study, T2 HASTE MRI evaluation of the fetus shows (a) fluid filled loops of bowel in the left chest (arrow). Most importantly, (b) liver herniation into the chest is demonstrated (arrow), an important prognosticator for the fetus. (c) Sagittal image with respect to the fetus more clearly shows stomach (arrowhead) at the same level as the heart (arrow).
Case 3: 25-year-old female after 24 weeks of gestation
An echogenic right lower lobe mass was identified on ultrasonographic survey [Figure 9a–b]. MRI [Figure 10a–b] showed a corresponding solid-appearing high signal mass on T2 weighted imaging. The MRI is of particular help in this case in demonstrating a feeding systemic vessel to the mass [Figure 10c] which helps to narrow the differential diagnosis, making pulmonary sequestration the primary consideration. Pulmonary sequestration is the second-most common antenatal lung mass detected after congenital pulmonary airway malformation (CPAM).[10] There can be difficulty identifying the feeding vessel on ultrasonography alone, which can make diagnosis problematic (both CPAM and pulmonary sequestration can appear as hyperechoic lower lobe masses). Even when a feeding vessel is identified, hybrid sequestration-CPAM lesions do exist which can only be delineated pathologically.[10] Our patient was asymptomatic at birth (neonatal chest radiograph demonstrates the right lower lobe mass [Figure 11], and was ultimately lost to follow-up thereafter.

- In case 3 of the study, prenatal obstetric ultrasonogram at 24 weeks gestational age demonstrates an echogenic, lobular intrathoracic mass in the area of the right lower lobe (between calipers) both (a) axially and (b) sagittally with respect to the fetus.

- In case 3 of the study, T2 HASTE MRI images of the fetus, both (a) axial and (b) sagittal with respect to the fetus, show a T2 hyperintense, solid mass in the same right lower lobe location (arrowheads). (c) Linear low signal structure on the coronal oblique image (arrow) suggests a feeding vessel.

- In case 3 of the study, neonatal radiograph confirms solid mass (arrowheads) in the right lower lobe region medially.
Case 4: 21-year-old female after 30 weeks of gestation
A very large avascular complex cystic and solid mass was demonstrated in the upper abdomen on the prenatal ultrasonogram [Figure 12a–c]. The mass was thought to arise from the liver, although a massively dilated intestinal segment was also considered. The patient was referred for Fetal MR to confirm organ of origin [Figure 13a–d]. MRI confirmed that the complex cystic mass appeared to arise from the left lobe of the liver. Small and large bowel were displaced, but remained normal in caliber [Figure 13d]. Neonatal Kidney, Ureter and Bladder (KUB) imaging [Figure 14a–b] emphasized the marked distention of the abdomen by the mass, while neonatal ultrasonogram confirmed the presence of a complex cystic mass with fluid-debris levels [Figure 15a–b]. Respiratory distress caused by both, mass effect on the diaphragm and congestive heart failure, necessitated early delivery and, later, neonatal surgery. Gross specimen [Figure 16a–b] shows an encapsulated, hemorrhagic mass which correlates very well with imaging; the diagnosis is infantile hemangioendothelioma (also known as infantile hepatic hemangioma).[11] This is the most common benign hepatic tumor found in this age group; approximately 50% are solitary lesions, as in this case.[11] While overall survival is high (approaching at least 90%), complications are seen very often in instances of solitary/focal lesions with most deaths occurring secondary to congestive heart failure (as in our case).[11] Given the imaging appearance of the mass, the differential diagnosis includes mesenchymal hamartoma, hemangioblastoma, and metastasis (such as from neuroblastoma).[1112]

- In case 4 of the study, (a) prenatal ultrasonogram at 30 weeks gestation shows a large, heterogeneously hypoechoic, septated liver mass (asterisk). (b) There is questionable internal vascularity on color Doppler interrogation. (c) Considerable mass effect is exerted on the fetal IVC and aorta, which are deviated leftward (arrowheads).

- In case 4 of the study, (a, b) Sagittal and coronal T2 HASTE and (c, d) axial T2 HASTE and T1 VIBE sequences show the largely homogenous, T1 hypointense, T2 iso- to hyperintense liver mass (asterisk). Internal flow-voids were not identified. Marked upward mass effect was seen under the diaphragm (a, arrowheads) on the sagittal image (a, H, heart; L, lungs). T1 weighted sequence (d) demonstrates a lack of high signal intensity within the mass; high signal in the left side of the fetal abdomen (d, arrowheads) represents meconium filled bowel loops.

- In case 4 of the study, (a) Frontal and (b) lateral abdominal radiographs performed on the first day of life highlight the gross distention caused by the gasless abdominal mass.

- In case 4 of the study, (a) Postnatal ultrasonographic evaluation of the mass (asterisk) in the newborn again shows its complex, solid and cystic nature without significant internal vascularity, on (b) power Doppler interrogation. Also, note fluid-debris levels within the mass (15a).

- In case 4 of the study, Infantile hemangioendothelioma. (a) The left hepatic lobe was resected; (b) cross-section of the mass reveals red-brown, congested material, grossly consistent with blood clot.
Case 5: 20-year-old female after 20 weeks of gestation
Screening obstetric ultrasonogram demonstrated a mixed cystic and solid mass over the dorsal aspect of the sacrum with suggestion of some internal vascularity [Figure 17a–c]. On the subsequent fetal MRI examination [Figure 18a–c], the mass is not only better characterized, but is clearly defined as entirely extra-pelvic. Gross pathology correlates well with imaging appearance [Figure 19]; the diagnosis is sacrococcygeal teratoma (SCT). The morbidity and mortality of SCT are determined largely by its intrapelvic/intraabdominal extent.[13] MRI helps in eliminating uncertainty from the ultrasound caused by acoustic shadowing due to fetal pelvic bones. Mass content is also of prognostic importance and is better delineated on MR. Both, a greater degree of pelvic involvement and the presence of a solid component correlate with increased risk of hemorrhage and fetal hydrops.[13] These factors can also impact the method of fetal delivery chosen, as well as the surgical approach for resection.[13]

- (a) In case 5 of the study, screening obstetric ultrasound exam performed at 20 weeks of gestation shows a mass in the area of the sacrococcygeal region (arrow), (b) Magnified image of the mass demonstrates solid (arrow) and cystic components (arrowhead). (c) After power Doppler interrogation, internal vascularity of the solid component is appreciable (arrow).

- In case 5 of the study, (a) axial, (b) coronal, and (c) coronal oblique T2 HASTE fetal MRI images emphasize the cystic and solid nature of the mass (arrowheads a-b), its sacrococcygeal location, and (most importantly) its lack of intrapelvic involvement. In (c) especially, the urinary bladder (arrow) is clearly separate from the more caudally located mass (arrowhead).

- In case 5 of the study, sacrococcygeal teratoma was seen. Cross section of the solid and cystic mass demonstrates tan-pink, firm excrescences which microscopically contain focal immature neural elements.
CONCLUSION
Fetal MRI is an important diagnostic compliment to prenatal ultrasound, not only for better characterization of fetal anatomy and pathology, but also identification of key aspects of a fetus’ condition unseen by ultrasound, which often helps prognostication. The fetus, expectant mothers, and graduate medical education programs’, all benefit as these examinations become more widely available in community medical settings.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/29/81772
REFERENCES
- Fetal MRI: A Developing Technique for the Developing Patient. AJR Am J Roentgenol. 2004;182:243-52.
- [Google Scholar]
- American College of Radiology whitepaper on MR safety. AJR Am J Roentgenol. 2002;178:1335-47.
- [Google Scholar]
- The use of iodinated and gadolinium contrast media during pregnancy and lactation. Eur Radiol. 2005;15:1234-40.
- [Google Scholar]
- An autosomal recessive syndrome of nasal anomalies associated with renal and anorectal malformations. Clin Dysmorphol. 2002;11:33-8.
- [Google Scholar]
- FREM 1 mutations cause bifid nose, renal agenesis, and anorectal malformations syndrome. Am J Hum Genet. 2009;85:414-8.
- [Google Scholar]
- Congenital Chest Malformations: A Multimodality Approach with Emphasis on Fetal MR Imaging. Radiographics. 2010;30:383-95.
- [Google Scholar]
- Congenital Lung Abnormalities: Embryologic Features, Prenatal Diagnosis, and Postnatal Radiologic-Pathologic Correlation. Radiographics. 2010;30:1721-38.
- [Google Scholar]
- Pediatric Liver Masses: Radiologic-Pathologic Correlation Part 1.Benign Tumors. Radiographics. 2010;30:801-26.
- [Google Scholar]
- Vascular Abnormalities of the Liver. In: Slovis TL, ed. Caffey's Pediatric Diagnostic Imaging (11th ed). Philadelphia: Mosby; 2008. p. :1900-4.
- [Google Scholar]
- MR imaging of Fetal Sacrococcygeal Teratoma: Diagnosis and Assessment. AJR Am J Roentgenol. 2002;178:179-83.
- [Google Scholar]






