Translate this page into:
A Rare Case of Primary osteosarcoma of urinary bladder
Address for correspondence: Dr. Aditi Jain, B 101, M.S. Palazzo, 491, Jakkur Main Road, Yelahanka Hobli, Bangalore- 560 064, India. E-mail: aditijain11@hotmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Extraskeletal osteosarcoma is a malignant mesenchymal soft tissue tumor without attachment to the bone, and is able to produce osteoid or cartilaginous matrix. This entity accounts for 1% of all soft tissue sarcomas. Thus far, less than 35 cases of bladder osteosarcomas have been reported in the literature. These tumors are associated with very poor prognosis. We report a case of primary osteosarcoma of the urinary bladder presenting with intermittent hematuria, dysuria, and right flank pain. Contrast-enhanced computed tomography scan of the abdomen, pelvis, and chest revealed a bladder mass and pulmonary metastases with specks of calcification.
Keywords
Extraskeletal osteosarcoma
urinary bladder primary osteosarcoma
mesenchymal tumors
INTRODUCTION

- Dr. Jagdeesh KS
Extraskeletal osteosarcomas are rare mesenchymal tumors that are difficult to differentiate from osteogenic sarcomas. They are characterized by production of osseous matrix that is not attached to the bone or the periosteum. Of these, mesenchymal tumors of the urinary bladder account for 0.04%.[1] The most common sites of occurrence are the lower extremity (47%), the upper extremity (20%), and the retroperitoneum,[23] with bladder accounting for about 35 cases reported so far.
CASE REPORT
A 36-year-old male presented with a 2-month history of intermittent hematuria, dysuria, and flank pain. He had undergone cystolithotomy 20 years earlier for the treatment of bladder calculi. He also had a history of recurrent urinary tract infection and intermittent hematuria. Double J stenting was performed on the right side in a previous cystoscopy examination. Cystoscopy in our institution revealed growth in the urinary bladder, which was biopsied and the sample sent for histopathology evaluation.
A plain radiograph of the kidney and urinary bladder showed faint specks of calcification in the region of the bladder on the left side with Double J stent on the right side [Figure 1]. Ultrasound showed irregular polypoidal bladder growth with multiple foci of calcification involving the vesicoureteric junctions (VUJ) on both sides. Bilateral hydrouretronephrosis was severe on the right side and moderate on the left side [Figure 2].
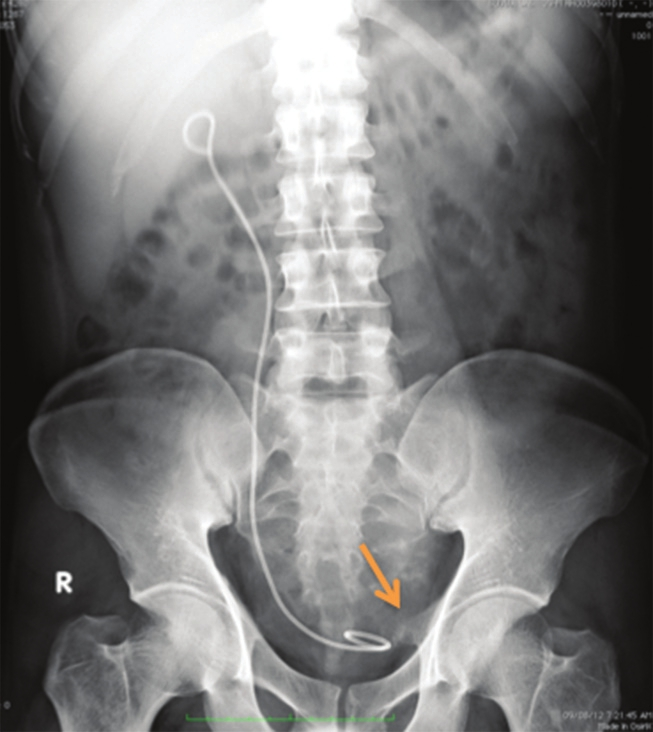
- X-ray of the kidney and urinary bladder shows calcific specks (arrow) in the left hemipelvis with Double J stent on the right side.
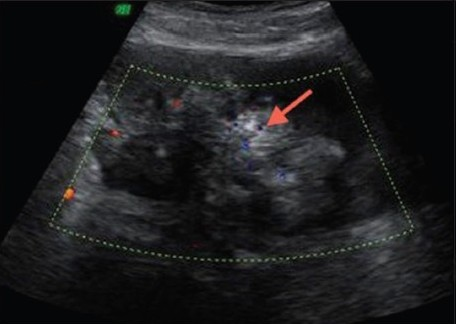
- Transverse ultrasound of the pelvis reveals a polypoidal mass in the urinary bladder with calcific specks (arrow).
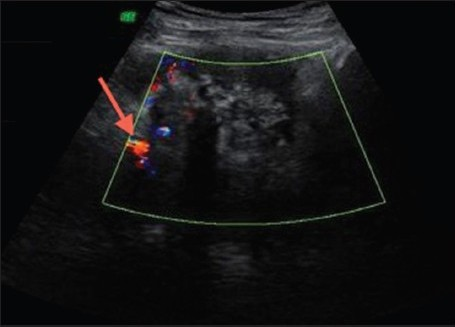
- Transverse ultrasound of the pelvis shows a polypoidal mass in the urinary bladder with vascularity (arrow) on color Doppler.
Contrast-enhanced computed tomography (CT) scan of the abdomen and pelvis revealed a heterogenously enhancing polypoidal mass involving the lateral walls and base of the urinary bladder (including VUJ). The mass measured approximately 70 mm (anteroposterior) ×80 mm (transverse) and showed multiple specks of calcification. Loss of fat planes was noted between the urinary bladder, prostate, and seminal vesicles [Figures 3 and 4]. Bilateral hydrouretronephrosis was noted with Double J stent in situ on the right side. CT of the chest showed multiple well-defined enhancing pulmonary nodules of varying sizes (5-15 mm), with calcification being noted in some of them [Figure 5].
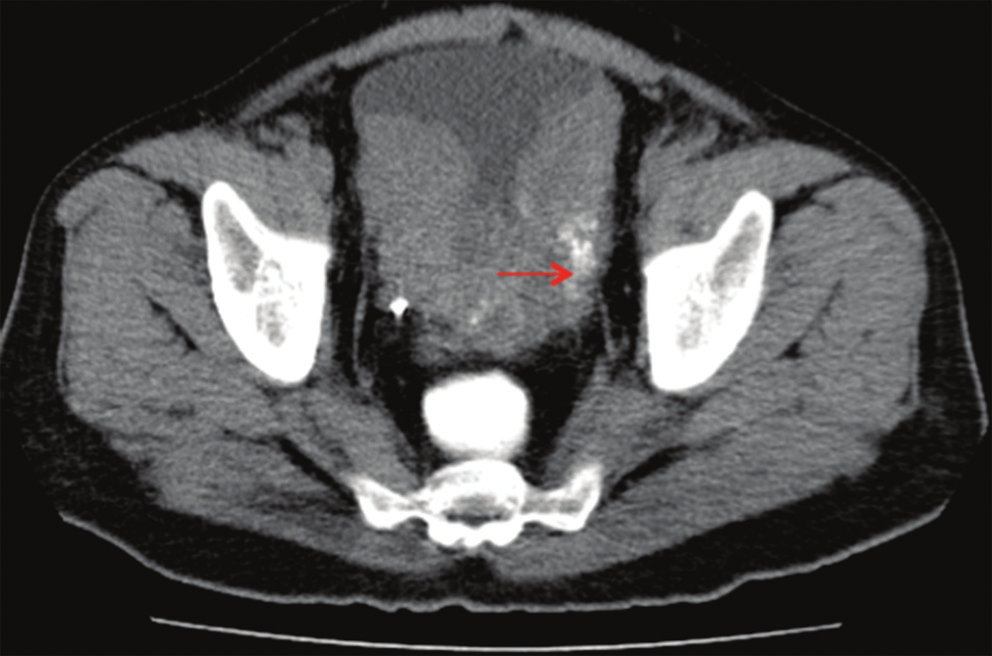
- Plain computed tomography of the pelvis shows polypoidal mass within the urinary bladder with dense foci of calcification on the left side (arrow).
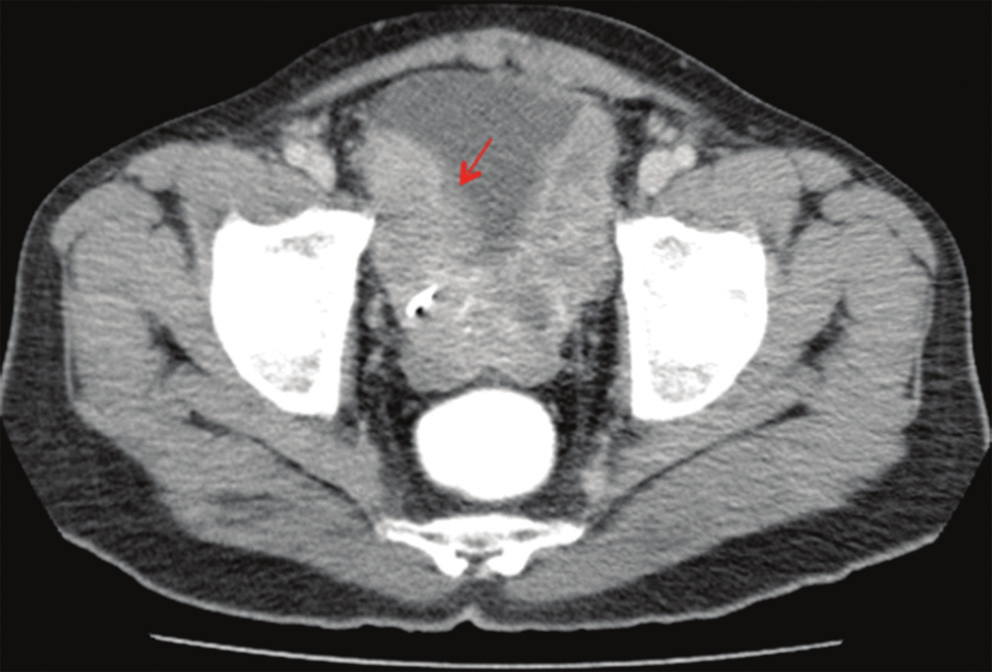
- Contrast-enhanced computed tomography of the pelvis shows a heterogenously enhancing polypoidal mass involving the bilateral lateral and posterior walls.
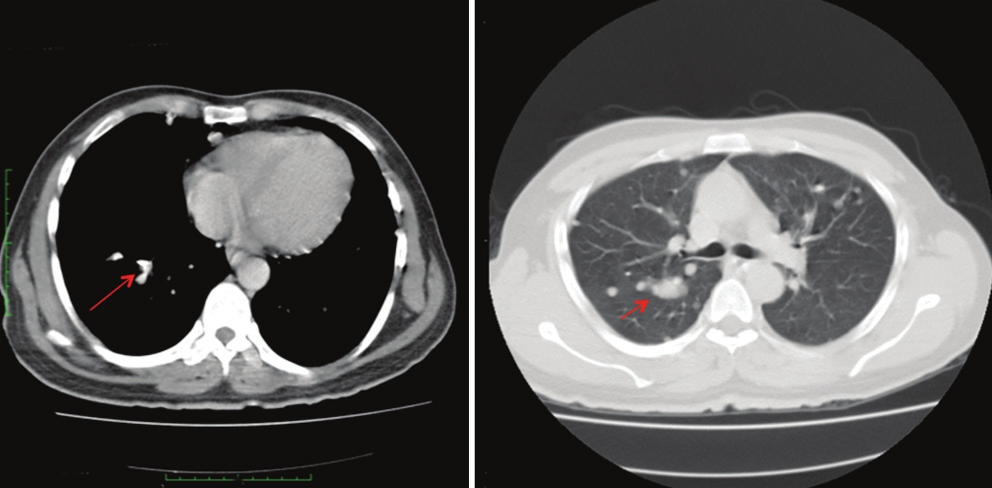
- Computed tomography scan of the chest shows multiple well-defined pulmonary nodules in bilateral lung parenchyma (lung window) with specks of calcification in few nodules (mediastinum window).
Microscopic examination revealed a tumor infiltrating into the vascularized fibrocollagenous tissue with extensive tumor necrosis. Tumor cells showed marked pleomorphism, with hyperchromatic tumor cells arranged singly and in small nests. Focally, tumor cells were seen embedded in lakes of osteoid matrix with focal calcification. Diagnosis of sarcomatoid variant (osteosarcomatous type) of urothelial carcinoma was made and the sample was sent for immunohistochemistry to rule out primary osteosarcoma of the urinary bladder [Figure 6]. Immunohistochemical investigations showed diffusely positive results with vimentin and negative results with cytokeratin. The final pathological diagnosis made was primary extraskeletal osteosarcoma of the urinary bladder. Radiographs of the upper and lower limbs were taken to rule out skeletal osteosarcoma.
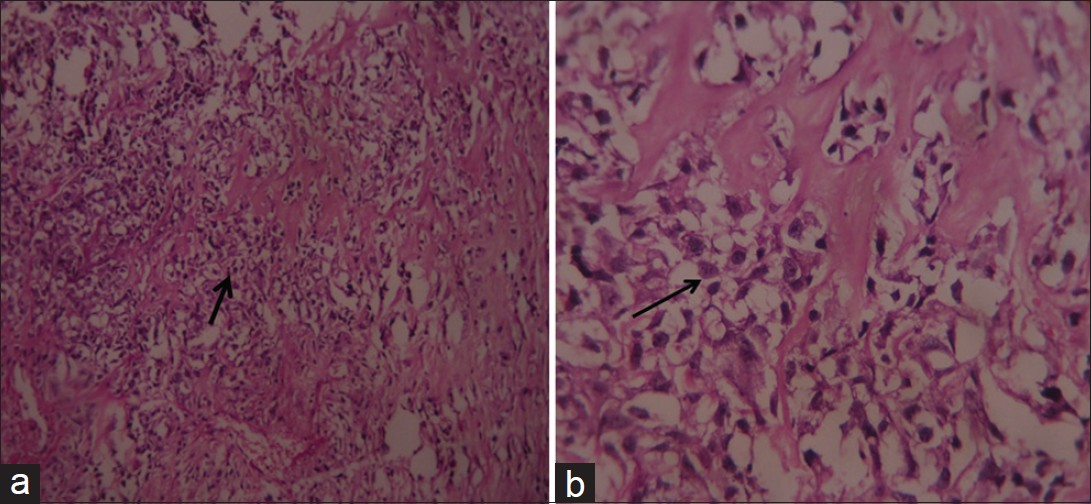
- Hematoxylin and eosin-stained specimen (a) at ×20, (b) at ×40, show tumor cells arranged singly and in small nests, embedded in a lace-like malignant osteoid matrix.
DISCUSSION
Fine and Stout[3] in 1956 suggested that extraskeletal osteosarcomas show behavior similar to primary osteogenic osteosarcoma in the bone. Subsequent studies have indicated that extraskeletal osteosarcoma should be considered clinically and therapeutically separate from osteogenic osteosarcoma.[4] Osteosarcoma, by definition, is a malignant tumor showing osteoid production and is known to occur in the 7th decade. It is more common in males (male to female ratio: 4:1). Some have a history of radiation therapy for urothelial carcinoma. The time interval between radiotherapy and development of sarcoma can be long, with a mean interval of 12 years. Most osteosarcomas arise in the trigone region, although cases have been reported in the renal pelvis and ureter as well. They present as solitary, large, polypoid, gritty, often deeply invasive, variably hemorrhagic mass, with size varying between 2 cm and 15 cm (median: 6.5 cm).
Histologically, tumors are composed of malignant cells surrounding variably calcified, woven bone lamellae. Foci of chondrosarcomatous differentiation or spindle cell areas may also be observed. The differential diagnosis includes urothelial carcinoma with osseous metaplasia and sarcomatoid variant of urothelial carcinoma (carcinosarcoma). The cytologic atypia differentiates osteosarcoma from stromal osseous metaplasia occurring in some urothelial carcinomas. A recognizable malignant epithelial component is diagnosis of sarcomatoid carcinoma even when osteoid is present The diagnosis of osteosarcoma should only be made after excluding all these possibilities, as osteosarcoma has worse prognosis than the other two disease entities.
Criteria for the diagnosis of primary extraskeletal osteosarcoma by Allan et al.,[5] are: (1) the presence of a uniform morphological pattern of sarcomatous tissue that excludes the possibility of malignant mesenchymoma, (2) the production of malignant osteoid or bone by the sarcomatous tissue, and the (3) ready exclusion of an osseous origin.
Immunohistochemical analysis in osteosarcoma is negative for pan-cytokeratin 7 and 20, epithelial membrane antigen, as well as a smooth muscle actin, desmin, CD34, and CD68. Vimentin[6] and p53 are strongly expressed in more than 95% of the neoplastic cells. In our case, vimentin was diffusely positive and cytokeratin was negative.
In carcinosarcoma, the immunostains for keratin or ultrastructural presence of desmosomes are seen, and can confirm their true carcinomatous nature with the presence of at least focal epithelial differentiation. The signs and symptoms are non-specific and include hematuria, dysuria, polyuria, and flank pain.
Primary tumor in the bladder on imaging may be detected either as a thickening of the bladder walls or as an intra-luminal mass. On CT, intra-luminal tumors may occasionally show fine calcifications. Sensitivity of CT in detecting the bladder carcinomas is in the range of 79-89%, and has a specificity ranging from 91% to 94.7%.[7] The high specificity enables direct referral for rigid cystoscopy and biopsy thus expediting diagnosis and treatment.
The treatment protocol depends on the depth of invasion, which is categorized as superficial, muscle invasive, or hyperinvasive. Superficial malignancies may be treated with electrocautery or instillation of Bacille Calmette-Guérin. Hyperinvasive tumors necessitate radical cystectomy with chemoradiation. For muscle-invasive tumors, radical cystectomy with or without chemotherapy has been the traditional standard, but, in an effort to improve the quality of life by avoiding urinary diversion procedures, the bladder-sparing trimodality therapy of transurethral resection of bladder tumor, systemic chemotherapy, and concurrent radiation therapy has increasingly been used in selected patients. As our patient already had pulmonary metastasis, surgical treatment was deferred and systemic chemotherapy (ifosfamide and doxorubicin) was being administered. Osteosarcoma of the urinary bladder is a rare aggressive tumor with poor prognosis. Majority of the patients have advanced stage at presentation and die within 6 months, most from the effects of local spread (urinary obstruction, uremia, secondary infection, etc.) and often with lung metastases. The stage of the disease at the time of diagnosis is the best predictor of survival.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/82/105145
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Primary osteosarcoma of the urinary bladder following cyclophosphamide therapy for systemic lupus erythematosus: A case report. J Med Case Rep. 2009;3:39.
- [Google Scholar]
- Extraskeletal osteosarcoma: Spectrum of imaging findings. AJR Am J Roentgenol. 2012;198:W31-7.
- [Google Scholar]
- Extraskeletal osteosarcoma. A clinicopathologic review of 26 cases. Cancer. 1990;65:2762-70.
- [Google Scholar]
- Osteogenic sarcoma of the somatic soft tissues. Clinicopathologic study of 26 cases and review of literature. Cancer. 1971;27:1121-33.
- [Google Scholar]
- Primary osteosarcoma of the urinary bladder treated with external radiotherapy in a patient with a history of transitional cell carcinoma: A case report. J Med Case Rep. 2010;4:70.
- [Google Scholar]
- Imaging and staging of transitional cell carcinoma: Part 1, lower urinary tract. AJR Am J Roentgenol. 2009;192:1481-7.
- [Google Scholar]






