Translate this page into:
Non-Syndromic Non-Familial Agenesis of Major Salivary Glands: A Report of Two Cases with Review of Literature
Address for correspondence: Dr. Ravi Prakash Sasankoti Mohan, Dhanwantri Nursing Home, Sarai Khalsa, Behind Head Post Office, Moradabad - 244 001, Uttar Pradesh, India. E-mail: sasan_ravi@rediffmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Agenesis of the major salivary glands is a rare and unusual condition, with only a few cases documented in the literature. The anomaly can be total or partial, unilateral or bilateral, and involve the parotid, submandibular, and sublingual glands. The resultant xerostomia leads to extensive dental demineralization. The authors report two cases with decreased saliva volume, impaired dental condition with extensive loss of tooth structure, and an astonishing pattern of dental destruction most notable on the facial and lingual surfaces of incisors and canines that can be best described as “chipping.” After detailed review of patient history, clinical examination, ultrasonography, contrast enhanced computed tomography, and magnetic resonance imaging a diagnosis of congenital absence of major salivary glands in both the patients was made. Dentists should be aware that salivary gland aplasia is an uncommon cause of dental deterioration. It may manifest itself not by extensive caries but as dental chipping effect. Early recognition and a therapeutic strategy can prevent further dental damage.
Keywords
Agenesis
chipping
major salivary glands
salivary glands
xerostomia
INTRODUCTION

The major salivary glands in humans develop from the ectodermal lining of the stomatodeum during the 6th week and 8th week of intrauterine life. Disturbances affecting ectodermal structures may include hypoplasia or agenesis of these glands. Congenital absence of major salivary glands is rare. Moreover, xerostomia and rampant caries are present due to reduced salivary flow. Anyone of the glands or group of glands may be absent either unilaterally or bilaterally. Salivary gland aplasia may be isolated or in association with other anomalies, particularly defects in the lacrimal apparatus.[1] Although, heredity is a significant factor, there are cases reported with no familial history of this entity. Males appear to be more commonly affected than females (male: female ratio = 2:1.2).[2] The precise incidence of major salivary gland agenesis is difficult to establish due to the asymptomatic nature of many cases.
In this report, we present the clinical and radiological characteristics of two cases of non-familial, non-syndromic agenesis of all the major salivary glands along with a brief literature review.
CASE REPORTS
Case 1
A 15-year-old male patient was referred to the dental out-patient department with an extensive carious breakdown of the mandibular permanent incisor teeth. His medical and family history was unremarkable. Extra-oral examination revealed no obvious abnormality or syndromal stigmata, including any features suggestive of ectodermal dysplasia, but the parotid and submandibular glands were impalpable. Intra-oral examination revealed obvious signs of xerostomia, dry and scaly lips, and rampant dental caries. A careful examination revealed the absence of Stenson's duct and Wharton's duct bilaterally. Minor salivary glands biopsies revealed the presence of labial and palatal glands that were found to be functional.
Complete complement of teeth was present but florid caries were seen. The decayed missing filled teeth index and decayed missing filled surface index recorded for the patient was 22 and 55 respectively suggestive of the severity of the condition. An unusual form of enamel loss due to chipping was observed in areas such as cervical regions and incisal and cuspal surfaces of incisors and molars. These areas do not normally become carious [Figure 1a]. The usual carious soft base was absent on the affected teeth.
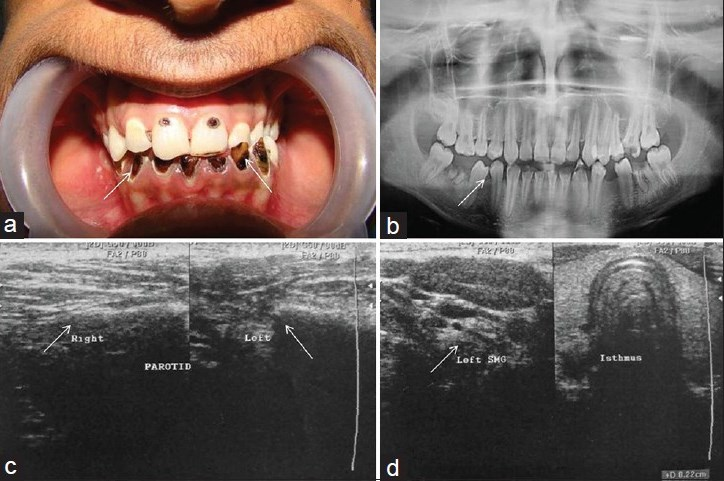
- Case 1: 15-year-old male child: (a) Intra-oral photograph shows chipping of incisal and cuspal surfaces of incisors best described as “chipping” defects. (b) Panoramic radiograph demonstrates extensive loss of tooth structure. (c) Longitudinal ultrasonogram demonstrates small atrophied echogenic tissue of bilateral parotid glands (white arrow). (d) Longitudinal ultrasonogram reveals small atrophied echogenic tissue of bilateral submandibular glands (white arrow).
The patient was unaware of any subjective xerostomia, changes in sweating or lacrimation. Sialometry showed a salivary flow rate of 0.02 mL/min. Sialography was not possible due to congenital absence of ducts and orifices. Laboratory blood test results (complete blood count, electrolytes, erythrocyte sedimentation, C-reactive protein, clotting ability) were normal.
Panoramic radiography revealed extensive loss of teeth structure [Figure 1b]. Further investigations included an ultrasound scan [Figure 1c and d] and contrast enhanced computed tomography in which the submandibular and parotid glands were not visualized [Figure 2a and b]. Magnetic resonance imaging (MRI) was performed which revealed complete absence of all major salivary glands [Figure 2c and d].

- Case 1: (a and b) Non-contrast computed tomography axial sections demonstrate bilateral absence of parotid glands (long arrows) and bilateral submandibular glands (Figure a, small arrows). (c) Multiplanar Magnetic Resonance (MR) image, coronal sections demonstrates absence of bilateral submandibular glands (small arrows). (d) Multiplanar MR axial sections shows absence of bilateral parotid glands (small arrows).
A complete work up by a team of ophthalmologist, Ear Nose Throat (ENT) surgeon, and dermatologist ruled out any other abnormality.
Case 2
An 18-year-old female patient was referred to the Out Patient Department with complaints of dry mouth and carious teeth. Other medical and family history were unremarkable. Extra-orally no abnormality was detected, except for the inability to palpate the parotid and submandibular salivary glands. However, her lips were dry and scaly. Intra-oral examination revealed signs of xerostomia, reduced salivary flow, dry erythematous oral mucosa, and extensive chipping of teeth, particularly incisors and canines [Figure 3a]. Wharton and Stenson papillae were absent. The patient claimed no problems with ocular or lacrimal secretions. Sialometry showed a salivary flow rate of 0.08 mL/min. Haematological examination findings were within normal limits.

- Case 2: An 18-year-old female: a) Intra-oral photograph shows extensive chipping of teeth, mainly incisors and canines. (b) Multiplanar MR coronal sections demonstrates agenesis of bilateral submandibular glands (small arrows). (c) Panoramic radiograph reveals multiple missing teeth and extensive destruction of teeth mainly incisors and canines. (d) Multiplanar MR axial sections reveals agenesis of bilateral parotid glands (small arrows).
Panoramic radiography revealed extensive destruction of teeth, particularly incisors and canines [Figure 3c]. Ultrasonography was unable to visualize any of the major salivary glands. MRI scan was performed, which confirmed the agenesis of all the major salivary glands [Figure 3b and d].
Consultation with an ophthalmologist, ENT surgeon, and dermatologist ruled out any other abnormality while there was no abnormality visible in the minor salivary gland biopsy.
For both the patients, the treatment was directed toward symptomatic relief and restoration of functional status of the teeth, and prophylactic prevention of further dental breakdown. Patients were given sialogogues (pilocarpine) and sugarless chewing gums. Both the patients were advised topical fluoride applications and fluoride toothpastes. The damaged teeth were restored with esthetic restorations and sealants. A non-cariogenic diet and proper brushing with soft bristled tooth brush was advised.
DISCUSSION
During the 4th-12th week of embryonic development, each of the salivary glands is formed at specific locations in the oral cavity through the growth of a bud from the oral epithelium into underlying ectomesenchyme. The epithelial bud grows and is branched forming ducts.[34] Presence of functional innervations was regarded essential for proper growth and maintenance of salivary gland structure. Parasympathetic denervation results in loss of glandular weight, while sympathetic denervation causes either atrophy of major salivary glands or hypertrophy of the others. Although the pathogenesis of congenital aplasia of salivary glands remains cryptogenic, a developmental basis along with sympathetic denervation is suspected. Developmentally, it is thought to be a pleotropic autosomal dominant disorder.[3]
Aplasia of major salivary glands is uncommon with an incidence of 1 in 5000 births.[5] This may be hereditary or syndromic. Salivary glands aplasia can develop in the absence of a familial history and may exist with no associated anomalies. Aplasia of the major salivary glands was described for the first time in 1885 by Gruber, who reported a case of bilateral agenesis of the submandibular gland.[6] Since then, 41 cases of salivary gland aplasia have been documented. Non-syndromic, non-familial presentation of complete agenesis of all major salivary glands as seen in our cases is rare, although agenesis is reported in a variety of unilateral and bilateral combinations.
The pattern of enamel defects seen in our cases was not typical of a carious lesion, the enamel could be easily chipped and involved cervical areas, cuspal and incisal tips. The chipping and demineralization of enamel can be explained on the basis that the diminished secretion of saliva resulted in impaired buffering of the dietary acids and a failure to form a protective enamel pellicle. Significant functional stress on these teeth explains the chipping of occlusal and incisal enamel. Such dental condition can occur in Sjogren's syndrome and radiation caries.[7]
Salivary gland aplasia may be isolated or in association with other anomalies, particularly defects in the lacrimal apparatus. The absence of major salivary glands has been observed in Lacrimo-auriculo-dento-digital syndrome, hemifacial microsomia, mandibulofacial dysostosis (Treacher Collins syndrome), multiple facial anomalies, and ectodermal dysplasia, and it can be a feature in first and second branchial arch anomalies.[89] Single case of bilateral parotid gland agenesis associated with Down's syndrome and bilateral agenesis of parotid glands and unilateral agenesis of submandibular gland in a cleft lip and palate patient have been described. Major salivary gland agenesis associated with lacrimoauriculodentodigital syndrome has also been reported by a number of investigators.[10]
Treatment is directed toward restoration of teeth with esthetic restorations, prevention of further dental damage by topical fluoride applications, fluoride toothpastes, mouthwashes, and sealants and to amplify the residual salivary function. Dietary instructions regarding a non-cariogenic diet and instructions of proper brushing with a soft bristled toothbrush were also advised.[2]
In a dental office, we encounter a wide variety of salivary gland disorders and secretory dysfunction. The oral examination must be thorough and include close scrutiny of salivary flow, mucosal state, and dental status. A non-familial, non-syndromic agenesis of all major salivary glands is rare and causes atypical dental demineralization. Attaining a definitive diagnosis requires organized examination and investigations.
CONCLUSION
We have presented two cases of congenital absence of all the major salivary glands. The history and clinical evidence of xerostomia, the unusual pattern of dental breakdown best described as “chipping,” the absence of duct orifices, and the results of specialized radiographic investigations, all served to confirm that both the patients had major salivary gland agenesis. The case report is unique in that no other anatomical structures were involved and there was no indication of a similar condition in any family member. It also emphasizes the general dental practitioner needs to be aware of this unusual pattern of dental breakdown that could be a result of salivary gland agenesis.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/2/6/109474
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- An unusual pattern of dental damage with salivary gland aplasia. J Am Dent Assoc. 2006;137:984-9.
- [Google Scholar]
- Unilateral agenesis of the parotid gland: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:712-4.
- [Google Scholar]
- Congenital unilateral absence of the submandibular gland. J Oral Maxillofac Surg. 1999;57:344-6.
- [Google Scholar]
- Aplasia of salivary glands with trisomy 13 syndrome: A rare association. J Anat Soc India. 2000;49:174-5.
- [Google Scholar]
- Congenital bilateral parotid gland agenesis in Klinefelter syndrome. J Craniomaxillofac Surg. 2010;38:248-50.
- [Google Scholar]
- FGF10 missense mutations in aplasia of lacrimal and salivary glands (ALSG) Eur J Hum Genet. 2007;15:379-82.
- [Google Scholar]
- Congenital absence of submaxillary gland detected on 99mTc-pertechnetate thyroid imaging. Clin Nucl Med. 1978;3:442.
- [Google Scholar]
- Aplasia of the submandibular gland.A case report. J Craniomaxillofac Surg. 1990;18:119-21.
- [Google Scholar]
- salivary gland aplasia with cleft lip and palate. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:594-9.
- [Google Scholar]






