Translate this page into:
Transjugular Intrahepatic Portosystemic Shunt for Maintenance of Portal Venous Patency in Liver Transplant Candidates
Address for correspondence: Dr. Ron Charles Gaba, Department of Radiology, Division of Interventional Radiology University of Illinois Hospital and Health Sciences System, 1740 West Taylor Street, MC 931, Chicago, Illinois-60612, United States. E-mail: rgaba@uic.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Maintenance of portal venous patency is vital to liver transplant candidates, as the presence of portal vein thrombosis (PVT) adversely impacts clinical outcomes by increasing surgical complexity and decreasing postoperative survival. By enhancing portal venous blood flow, transjugular intrahepatic portosystemic shunt (TIPS) creation may enable clearance of PVT and preservation of portal venous patency in cirrhotic patients. Herein, we describe four cases in which TIPS produced and sustained an open portal venous system in liver transplant candidates with partial PVT. All patients demonstrated rapid and effective flow-enabled clearance of clot and intermediate to long-term preservation of portal venous flow. On this basis, we propose that maintenance of portal venous patency in liver transplant candidates with partial PVT represents a developing indication for TIPS.
Keywords
Liver transplant
portal vein thrombosis
transjugular intrahepatic portosystemic shunt

INTRODUCTION
Partial or complete portal vein thrombosis (PVT) complicates 5-26% of liver cirrhosis cases, and is primarily related to stagnant portal venous blood flow in the setting of portal hypertension.[1] The presence of PVT negatively impacts liver transplant patients; not only are auxiliary (intraoperative thrombectomy or jump graft creation) or advanced (renoportal anastomosis, cavoportal hemitransposition, and multivisceral transplantation) maneuvers required at the time of surgery depending on the extent of clot formation, but posttransplant mortality risk is also increased.[2] Preoperative management of PVT and prevention of clot propagation is thus of paramount importance in liver transplant candidates. While systemic anticoagulation may result in portal recanalization in 40-70% of cases,[1] it does not improve portal hemodynamics; thus contributing to thrombus progression in a small percentage of cases,[1] and its use may be precluded in cirrhotic individuals with gastroesophageal variceal bleeding risk. By establishing a low pressure outflow pathway for splanchnic blood volume, transjugular intrahepatic portosystemic shunt (TIPS) creation can increase portal venous flow, and therefore represents an emerging approach for the dissolution of PVT in cirrhotic patients. Herein, we present a series of cases highlighting the utility of TIPS in producing and preserving portal venous patency in liver transplant candidates.
CASE REPORT
Institutional review board approval is not required for small retrospective case studies at the authors’ hospital.
Patients and PVT
Four patients with liver cirrhosis and partial PVT underwent TIPS creation for preservation of portal venous patency for potential liver transplantation between June 2010 and January 2012. Three of four patients were formally listed with the United Network for Organ Sharing (UNOS); one patient underwent TIPS in anticipation of future listing. The indications for proactive early liver transplantation listing consisted of clinical signs of liver decompensation, namely occurrence of ascites and/or anasarca, in registered patients. None of the patients had hepatocellular carcinoma. The study cohort consisted of one man and three women of mean age 58 ± 11 (range: 45-69) years. Causes of underlying liver disease included nonalcoholic steatohepatitis (NASH) (n = 2), nonalcoholic fatty liver disease (n = 1), autoimmune hepatitis (n = 1). Child-Pugh class included A (n = 2), B (n = 1), and C (n = 1); and mean Model for End-Stage Liver Disease (MELD) score was 14 ± 4. PVT was associated with nonocclusive superior mesenteric vein (SMV) thrombus in one case and partial splenic vein clot in one case. None of the patients were on systemic anticoagulation due to Grade 2 esophageal varices diagnosed endoscopically in all cases. All patients were referred to interventional radiology (IR) for TIPS for the specific indication to preserve portal venous patency.
TIPS creation
TIPS procedures were performed in the IR suite using general anesthesia. Right jugular venous access was gained with dilation to a 10 French sheath. A 5 French catheter was used to engage the right hepatic vein. After hepatic venography and pressure measurement, wedged hepatic venography was performed. Next, a Rösch-Uchida Transjugular Liver Access Set (Cook Medical Co., Bloomington IN) was used to access the right portal vein. After portal vein catheterization and direct portal vein pressure measurement, balloon dilation of the hepatic parenchymal tract was performed. Next, direct portography was performed. Subsequently, an 8 (n = 1) or 10 mm (n = 3) Viatorr covered stent grafts (W.L. Gore and Associates, Flagstaff, AZ) were deployed across the liver tract. Balloon angioplasty was performed using a 6-8 mm balloon. After measurement of final portal and right atrial pressures, completion shunt venography was performed. Clot dissolution techniques, including catheter-directed thrombolysis and mechanical thrombectomy, were not employed.
TIPS creation was technically successful in all cases. Mean initial portosystemic pressure gradient (PSG) was 18 ± 7 (range: 9-26) mmHg, and mean final PSG was 8 ± 1 (range: 7-9) mmHg. Mean PSG reduction was 10 ± 8 (range: 0-19) mmHg. There were no procedure related complications. One patient developed mild hepatic encephalopathy (West Haven Classification System Grade 1) after TIPS.
Portal venous patency, liver transplantation, and patient survival
Following TIPS creation, patients underwent cross-sectional imaging at approximately 1-month post-procedure and then at 3-4 month interval to assess clot clearance and venous patency. After TIPS, Doppler ultrasound imaging performed at median 27 ± 79 (mean: 63) days post-procedure showed mean portal venous velocity increase from 13.5 ± 6.7 (range: 5.5–21.8) cm/s to 84.9 ± 22.2 (range: 68.0-116.8) cm/s, or an increase of 71.5 ± 28.5 (range: 46.2-111.3) cm/s. PVT and concomitant SMV or splenic vein thrombus spontaneously fully cleared in all cases within mean 79 ± 47 (range: 16-124) days post-TIPS [Figures 1 and 2]. Although no patient has yet undergone liver transplantation to date, as only 19% of liver transplantations occur in patients with MELD scores <15 in the geographic region of our transplant center,[3] no recurrence of PVT has been identified after mean 460 ± 199 (range: 185-609) days of imaging follow-up. One patient died 620 days after TIPS due to sepsis. The other three patients remain alive at mean 489 ± 123 (range: 358-602) days after TIPS.
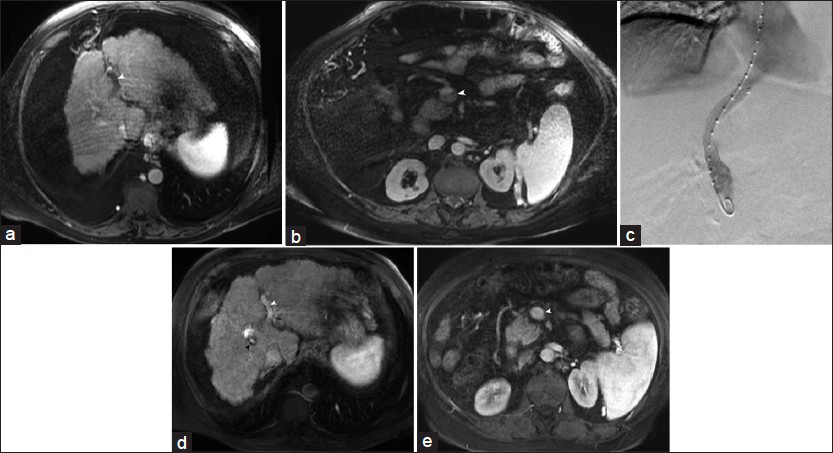
- 63-year-old man with portal vein and superior mesenteric vein thrombosis. (a and b) Contrast-enhanced axial magnetic resonance images reveal left intrahepatic portal vein thrombosis (arrowhead) and nonocclusive superior mesenteric vein clot (arrowhead). (c) Digital subtraction venogram performed after 10 mm transjugular intrahepatic portosystemic shunt creation demonstrates widely patent shunt. (d and e) Contrast-enhanced magnetic resonance images taken 4-months later displays complete recanalization of left portal vein and superior mesenteric vein (white arrowheads). Black arrowhead in (d) indicates patent transjugular intrahepatic portosystemic shunt.
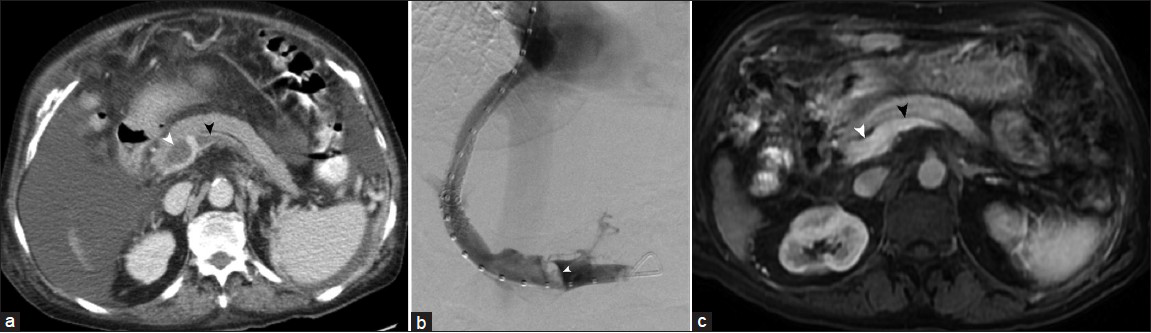
- 69-year-old woman with portal vein and splenic vein thrombosis. (a) Contrast -enhanced axial computed tomography image reveals nonocclusive thrombus at portal confluence (white arrowhead) and within splenic vein (black arrowhead). (b) Digital subtraction venogram performed after 10 mm transjugular intrahepatic portosystemic shunt creation demonstrates patent shunt, and shows presence of filling defect at portal confluence (arrowhead). (c) Contrast enhanced magnetic resonance images taken 6-months later displays complete recanalization of portal vein (white arrowhead) and splenic vein (black arrowhead).
DISCUSSION
The success of TIPS in the management of portal hypertensive complications[4] has prompted translation of this procedure from traditional indications, such as medically refractory gastroesophageal variceal hemorrhage and intractable ascites or hepatic hydrothorax, to newer indications, such as early use in variceal bleeding patients. In this vein, the application of TIPS for the treatment of PVT represents another developing indication for this procedure, and may enhance the care of liver transplant candidates by ensuring conventional operative approaches to transplantation, which may be significantly complicated or even precluded in the setting of partial or complete PVT,[1] as well as optimizing posttransplant survival, which is negatively impacted by PVT.[2]
In the current case series, partial PVT was successfully cleared from the portal venous system as well as the superior mesenteric and splenic veins using TIPS to enhance portal venous flow. Although the biochemistry of fibrinolysis is well-described, the role of hemodynamic factors in this process is often neglected. Originally described by Virchow, flow stasis contributes to vascular thrombosis by reducing laminar clearance of local thrombin and fibrin monomer. Experimental and mathematical models have demonstrated that the shear forces exerted by circulating blood promote mechanical dissolution of nonocclusive thrombi.[5] Higher velocity blood flow results in increased rates of mechanical degradation, as well as increased deposition of physiologic fibrinolytic agents. In the cases herein, portal venous flow was increased more than five-fold after TIPS to a mean of greater than 80 cm/s; normal portal venous flow velocity approximates 16-40 cm/s. The increased portal venous flow following TIPS creation may resolve any extant thrombus and obviate the need for concomitant use of anticoagulation and/or mechanical or thrombolytic techniques. As a final note, because complete PVT may damage vascular endothelium and increase probability for recurrent clot formation, early TIPS intervention should be considered while PVT is partial or nonocclusive to avert this risk.
Our experience with flow-enabled PVT dissolution is corroborated by other series describing the effectiveness of TIPS in promoting portal venous patency. Two studies have addressed the specific application of TIPS for maintenance of portal venous patency in liver transplant patients. In 2012, D’Avola et al., reported 100% portal vein patency in 15 patients with main trunk or branch vessel partial PVT who underwent TIPS followed by orthotopic liver transplantation (OLT) at median 185 days postprocedure.[6] In that study, a control group of eight patients with similar nonocclusive PVT who did not undergo TIPS showed 50% portal vein patency at OLT performed at median 213 days after PVT diagnosis.[6] In 2006, Bauer et al., reported nearly 90% improvement in portal venous patency 2-45 months post-TIPS for treatment of varying degrees of nonocclusive PVT.[7] The findings of these studies are further supported by report of at least one individual case describing use of TIPS to keep the portal vein open for liver transplantation.[8] Other large studies have confirmed the utility of TIPS in treating PVT in cirrhotic patients without specific intent as a bridge to liver transplantation. In 2011, Luca et al., described 87% patency improvement (complete recanalization in 57%) among 70 patients with nontumoral PVT who underwent TIPS.[9] In 2011, Han et al., reported 100% portal venous patency after TIPS in 43 patients with varying degrees of PVT.[10] Once a contraindication to TIPS creation, PVT may now represent an unequivocal procedural indication for TIPS given the efficacy demonstrated in such investigations.
The benefits of TIPS for clearance of PVT must be weighed against possible risks. When performed by experienced operators in properly selected candidates, TIPS may be created with a reasonable safety profile. TIPS complications that particularly affect subsequent transplantation are uncommon, and the presence of TIPS does not typically impact operative technique or result in detrimental effects on posttransplant patient clinical outcomes. As a matter of caution, IR operators should take great care in proper stent length selection as well as device deployment, as shunt extension into the portal vein or hepatic level inferior vena cava (IVC) and right atrium, either due to device misplacement or migration, may leave inadequate room for vascular cross-clamping at the time of surgery.
CONCLUSION
In conclusion, we describe four cases of partial PVT in liver transplant candidates successfully cleared after TIPS creation. In all cases, portosystemic shunting of blood resulted in rapid and effective flow-enabled clearance of clot and intermediate to long-term preservation of vessel patency. While our clinical observations are made on the basis of a small sample size and should thus not be overstated, the findings herein are corroborated by other studies presenting similar findings, and affirm the utility of TIPS for maintenance of portal venous patency prior to liver transplant and highlight this application as an emerging indication for TIPS.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/1/29/115761
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Portal vein thrombosis, cirrhosis, and liver transplantation. J Hepatol. 2012;57:203-12.
- [Google Scholar]
- Portal vein thrombosis and liver transplant survival benefit. Liver Transpl. 2010;16:999-1005.
- [Google Scholar]
- 2010 Annual Report of the U. S. Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients. Rockville MD: Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation; 2011.
- [Google Scholar]
- American Association for the Study of Liver Diseases Practice Guidelines: The role of transjugular intrahepatic portosystemic shunt creation in the management of portal hypertension. J Vasc Interv Radiol. 2005;16:615-29.
- [Google Scholar]
- Blood clot dissolution dynamics simulation during thrombolytic therapy. J Chem Inf Model. 2005;45:1686-90.
- [Google Scholar]
- Efficacy of transjugular intrahepatic portosystemic shunt to prevent total portal vein thrombosis in cirrhotic patients awaiting for liver transplantation. Transplant Proc. 2012;44:2603-5.
- [Google Scholar]
- The role of TIPS for portal vein patency in liver transplant patients with portal vein thrombosis. Liver Transpl. 2006;12:1544-51.
- [Google Scholar]
- Transjugular intrahepatic portosystemic shunt to keep vein open. Liver Transpl. 2009;15:558-60.
- [Google Scholar]
- Short- and long-term effects of the transjugular intrahepatic portosystemic shunt on portal vein thrombosis in patients with cirrhosis. Gut. 2011;60:846-52.
- [Google Scholar]
- Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with symptomatic portal hypertension in liver cirrhosis. J Hepatol. 2011;54:78-88.
- [Google Scholar]






