Translate this page into:
Spontaneous Biliary Peritonitis in Children
Address for correspondence: Dr. Anu Singhal, 244/2d, Railway Officers’ Enclave, Panchkuian Road, New Delhi - 110 001, India. E-mail: drsinghals@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pediatric Spontaneous Bile duct perforation is a rare clinical condition with only around 150 cases reported worldwide. Early management gives excellent prognosis but the condition often presents a diagnostic dilemma. Hepato-biliary Technetium-99m-iminodiacetic acid scintiscan is the diagnostic investigation of choice but its availability in third world countries is limited. We present two cases of spontaneous biliary peritonitis in children, which were diagnosed without scintiscanning. The first case was a one-and -a half-year-old child, who was diagnosed with biliary peritonitis without pneumoperitoneum by a combination of Ultrasound (USG), Contrast enhanced computed tomography (CECT), and Magnetic Resonance Imaging (MRI). The child underwent USG-guided drainage and subsequent cholecystectomy with hepatico-jejunostomy. The second child also had biliary peritonitis without pneumoperitoneum, which was initially suspected on USG. CECT revealed dilated gall bladder and fluid collection in sub-hepatic space and pelvis. Abdominal paracentesis revealed presence of bile. The child responded to conservative therapy. Both are doing well on two-year follow-up. In a patient with jaundice, biliary tract abnormalities and/or free fluid, either generalized or localized to peri-cholecystic/sub-hepatic space on USG/CT/MRI, in the absence of pneumoperitoneum, suggest a diagnosis of biliary perforation even in the absence of scintiscanning.
Keywords
Biliary peritonitis
conjugated hyperbilirubinemia
spontaneous biliary perforation
ultrasound

INTRODUCTION
Spontaneous perforation of the bile duct (SPBD) is a rare surgical cause of jaundice in infancy.[1] Since its early reports and description by Dijkstra in 1932 and Caulfield in 1936, only about 150 cases have been reported till date, of which, the last two decades have contributed only 60 cases.[1]
This disorder is often not recognized though it usually requires immediate surgical treatment.[2] Radionuclide scan is the gold standard investigation and leakage of tracer in the peritoneal cavity is diagnostic.[1] In a prospective regional survey of infants with persistent conjugated hyperbilirubinaemia only two out of nearly 200 children presented with bile peritonitis and diagnosis was delayed in both cases. Since the clinical picture is varied and access to hepatic scintiscanning is relatively restricted in most developing countries, there is often a diagnostic dilemma that causes delay in surgical intervention.[3] However, clinical findings and other radiological investigations can often indicate the diagnosis.[3] We present two cases of spontaneous biliary peritonitis in children below 5 years, where diagnosis was made in the absence of scintiscanning. Both cases did not have any history of trauma or preceding signs and/or symptoms related to the hepato-biliary system.
CASE REPORTS
Case 1
A one-and-half-year-old male child presented with a 7-day history of fever, acholic stools, and vomiting and progressive abdominal distension for 3 days. Clinical examination revealed fever, icterus, abdominal distension, sluggish bowel sounds, tender hepatomegaly, guarding with rebound tenderness and fluid thrill. Total Leucocyte Count (TLC) was 17,000/dl with 83% neutrophils and Serum Bilirubin was 6.8 mg/dl. Ultrasound (USG) revealed ascites with dilatation of common bile duct (CBD), common hepatic duct (CHD), and intra-hepatic biliary radicals. Contrast Enhanced Computed Tomography (CECT) and Magnetic Resonance Imaging (MRI) confirmed the USG findings and also showed sudden tapering of distal CBD, distended gall bladder, peri-cholecystic fluid, and marked ascites. A disproportionately large fluid collection was seen in left posterior peri-hepatic space [Figures 1 and 2]. There was no evidence of pneumo-peritoneum. A provisional diagnosis of biliary perforation was made and the child was referred to a tertiary pediatric surgery centre, where abdominal paracentesis revealed bile. Two USG-guided pigtail drains were placed which drained nearly 800 ml of bile. The child was kept on antibiotics and nutritional support and subsequently taken up for definitive surgery. Exploratory laparotomy with adhesionolysis and cholecystectomy with Roux-en-Y hepatico-jejunostomy was performed [Figure 3]. The child recovered and has had an uneventful post-operative period over the last two years.

- Case1: One-and-half-year-old male child diagnosed as having spontaneous biliary peritonitis. (a) Contrast enhanced computed tomography axial section shows dilated gall bladder (A) and dilated common bile duct (B), (b) Contrast enhanced computed tomography axial section demonstrates free fluid (C), (c) Contrast enhanced computed tomography axial section multiplanar reconstructed coronal image demonstrates dilated gall bladder (A), (d) Contrast enhanced computed tomography axial section multiplanar reconstructed coronal image demonstrates dilated common bile duct (B) and free fluid (C).
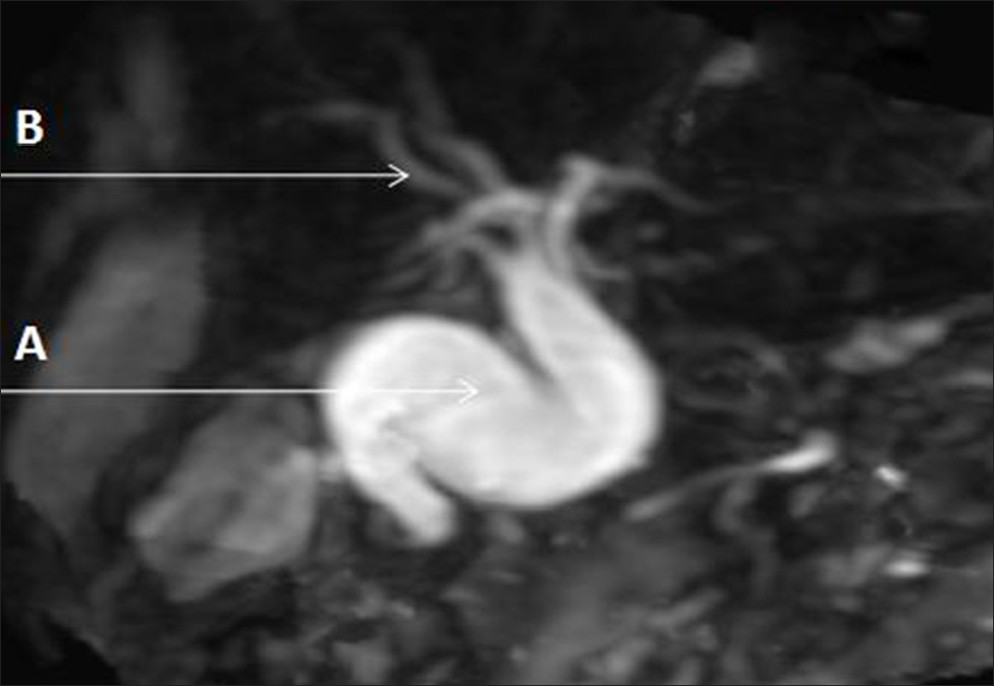
- Case 1: One-and-half-year-old male child diagnosed as having spontaneous biliary peritonitis. Magnetic resonance cholangio-pancreatography image shows grossly dilated common bile duct (A) and dilatation of intra hepatic biliary radicals (B).

- Case 1: One-and-half-year-old male child diagnosed as having spontaneous biliary peritonitis. Photograph taken during surgery shows distended gall bladder (A), dilated bile duct (B), and bile stained gastro-hepatic omentum (C) suggestive of biliary leak.
Case 2
A 3-year-old male child presented with complaints of abdominal pain and high-grade intermittent fever, mild jaundice without cholestatic features, vomiting, and a lump in the right upper abdomen for 6-7 days. Initial imaging investigations, comprising of two sonograms were done elsewhere prior to admission at our center. First USG revealed large cystic area in the region of the gall bladder (GB) that was likely to be a distended GB/choledochal cyst. Second USG showed similar findings but suggested ruptured left liver lobe abscess as a differential as the cystic area was subjacent predominantly to the left lobe, alongwith presence of free fluid in right iliac fossa. The child had been started on antibiotics and anti-pyretics by a private clinician, which was continued even after his admission. However, USG-guided abdominal paracentesis from right iliac fossa revealed the presence of bile in the fluid collection. This led to a revised diagnosis of biliary perforation and subsequently a Computed Tomography (CT) scan was done [Figure 4]. It revealed hydrops of gall bladder (GB) with the neck of the GB going across the midline from right to left, crossing anterior to common bile duct and possibly compressing it, as there was dilatation of the right and left hepatic ducts and the common hepatic duct. There was no evidence of thickening of GB wall. A small collection of fluid was seen in the posterior left peri-hepatic space around the neck of GB along with some free fluid in right paracolic gutter, indicative of localized biliary perforation [Figure 4a and b]. Hemogram revealed leukocytosis (TLC was 17300/dl and an elevated Serum Bilirubin level of 2.8 mg/dl.. The child was continued on conservative management. MRI of upper abdomen done about 7 days later [Figure 5] showed reduction in diameter of GB from 5 cm to approximately 2.8 cm. Dilatation of hepatic ducts persisted with smooth transition in region of proximal CBD which was normal in caliber. Inflammatory stranding was seen in left sub-hepatic space with no free fluid. A diagnosis of hydrops of gall bladder with dilatation of central hepatic ducts and common hepatic duct and recovering biliary perforation was made. A follow-up MRI done a year-and-a-half later showed partially distended GB in similar location, and persisting dilatation of central hepatic ducts and common hepatic duct, which tapered smoothly into a normal caliber CBD [Figure 6a and b]. The child improved with conservative management and is currently asymptomatic on follow-up investigation.
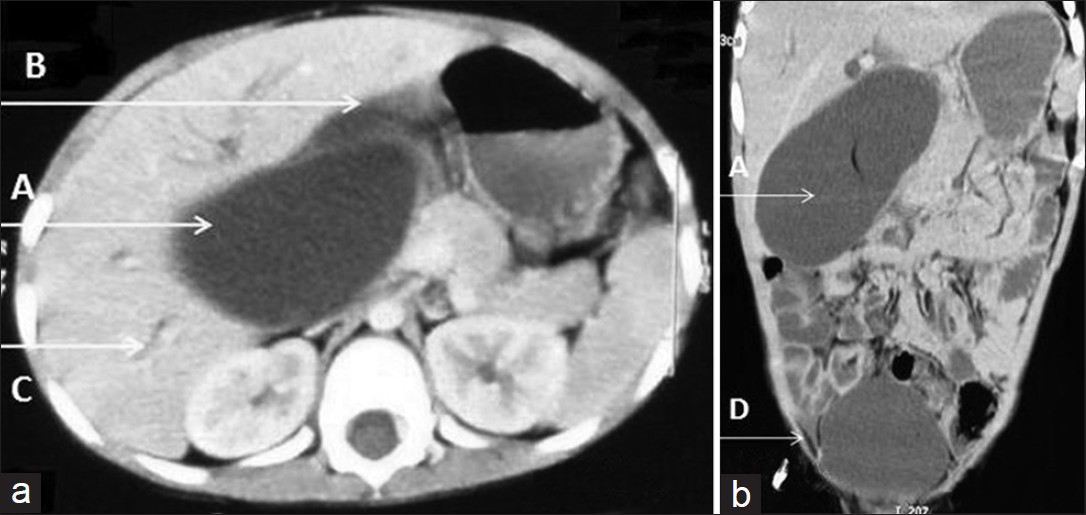
- Case 2: Three-year-old male child with abdominal pain and high-grade intermittent fever, mild jaundice without cholestatic features, vomiting, and a lump in the right upper abdomen later diagnosed as having spontaneous biliary peritonitis. (a) Contrast enhanced computed tomography axial section demonstrates dilated gallbladder crossing the midline (A), free fluid in left sub hepatic space (B), and dilated intra hepatic biliary radicals, (b) Contrast enhanced computed tomography axial section multiplanar reconstructed coronal image demonstrates dilated GB crossing midline (A) and free fluid in pelvis (D).

- Case 2. Three-year-old male child diagnosed as having spontaneous biliary peritonitis. T2-weighted fat suppressed magnetic resonance cholangio- Pancreatography image shows dilated gallbladder (A) with stranding near gall bladder neck (B).
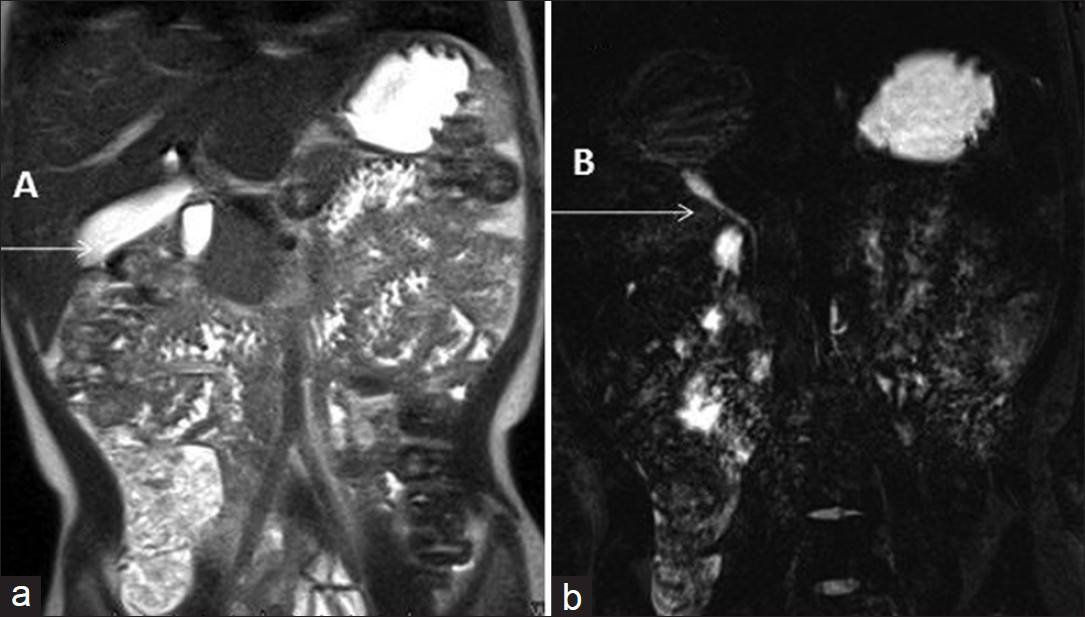
- Case 2: 3-year-old male child diagnosed as having spontaneous biliary peritonitis. (a) Follow-up T2-weighted magnetic resonance cholangio- Pancreatography image shows normally distended Gall Bladder (A), (b) Follow-up T2-weighted fat suppressed cholangio-pancreatography image of case 2 shows normal caliber common Bile duct (B).
DISCUSSION
Spontaneous bile duct perforation is usually seen in children below 4-years of age with the peak incidence during the first year.[3] The most common symptom is abdominal distension and/or jaundice. Other symptoms include fever, vomiting, abdominal mass, pale-colored stools, and poor weight-gain. Bile-staining of hydroceles, inguinal hernia or abdominal wall are characteristic. The general condition is usually good and only few cases have pyrexia. Most cases have a sub-acute onset and potentially fluctuating symptoms. However, rarely it may present acutely, with localized or generalized peritonitis and septicemic shock, without previous signs of biliary tract disease.[12] In a review of 54 cases, the clinical presentation was peritonitis with or without ascites.[3]
Serum bilirubin and liver enzymes are often normal or only mildly elevated. There may be a mild leukocytosis. The relatively low bilirubin in the presence of acholic stools is a diagnostic indicator. Diagnostic paracentesis will usually show bile-stained ascites but the bile staining may not be obvious early in the disease.[2] The common radiological investigation performed is abdominal ultrasound. The demonstration of tracer in the peritoneal cavity on a radionuclide scan with failure of tracer to enter the bowel is diagnostic.[1] However, access to scintiscanning is limited in India and other third world countries and diagnosis is based on clinical parameters and other radiological investigations.[3] Magnetic resonance cholangiopancreatography has been postulated to delineate bile duct perforation as well as demonstrate anatomical anomalies.[4]
Several theories proposed for the etiology of this entity include congenital mural weakness of the common bile duct, ischemia, distal biliary obstruction, and pancreatico-biliary malunion (PBM).[1] Most perforations occurring close to the junction of the cystic duct with CBD support the theory of a developmental weakness of the wall of the duct that perforates after reaching a critical intraductal pressure.[1] CBD receives its blood supply from two postero-lateral marginal arteries. This may predispose to focal ischemia of the anterior CBD, resulting in perforation.[5] PBM is a congenital anomaly in which a union of the pancreatic and biliary ducts is located outside the duodenal wall containing the sphincter of Oddi.[6] Pancreatic juice refluxing into the bile duct is activated by mixing with bile to become potentially destructive. The dilated bile duct caused by the PBM may lead to acute inflammation and micro-abscess formation in the duct wall, eventually resulting in perforation.[1] SPBD in association with PBM is related to an abrupt increase in intra-luminal pressure from impaction of a protein plug.[7] There is evidence to suggest that SPBD and choledochal cysts are interrelated entities with a common pathogenic factor. PBM, intrinsic bile duct weakness, and distal bile duct stenoses have been implicated in both of these conditions.[48] A short segment involvement predisposes to perforation whereas involvement of a longer segment gives rise to a choledochal cyst.[9] The incidence of spontaneous perforation in a choledochal cyst is around 2%.[3]
Almost all cases need peritoneal drainage with or without cholecystectomy, primary repair with or without t-tube drainage or hepatico-jejunostomy.[1] Definitive treatment may be done primarily but is often delayed until the patient improves on peritoneal drainage and supportive therapy. Recently, peritoneal drainage with endoscopic retrograde cholangio-pancreaticography and stenting of CBD has also been reported.[10] However, in patients with choledochal cysts, PBM or distal obstruction-biliary reconstruction is the procedure of choice.[1] In our series, the first case underwent initial peritoneal drainage and subsequent hepatico-jejunostomy, whereas the second case was managed conservatively, only the second such case reported so far.[1]
CONCLUSION
Diagnosis of biliary peritonitis includes a high degree of suspicion both on the part of the clinician and the radiologist. Though scintiscan is the most appropriate diagnostic investigation for diagnosing biliary leak,[1] however, it is not universally available.[3] In a patient of jaundice, biliary tract abnormalities and/or free fluid either generalized or localized to peri-cholecystic/sub-hepatic space on USG/CT/MRI in the absence of pneumoperitoneum, a diagnosis of biliary perforation should be entertained.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/1/25/114213
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Spontaneous perforation of the bile duct in infancy and childhood: A systematic review. J Pediatr Gastroenterol Nutr. 2010;50:677-81.
- [Google Scholar]
- Spontaneous perforation of common bile duct in infants. Arch Dis Child. 1976;51:883-6.
- [Google Scholar]
- Spontaneous biliary perforation in infancy and childhood: Clues to diagnosis. Indian J Pediatr. 2007;74:509-10.
- [Google Scholar]
- Bile duct perforation in children: Is it truly spontaneous? Ann Acad Med Singapore. 2006;35:905-8.
- [Google Scholar]
- A new look at the arterial supply of the bile duct in man and its surgical implications. Br J Surg. 1979;66:379-84.
- [Google Scholar]
- Does pancreatico-biliary maljunction play a role in spontaneous perforation of the bile duct in children? Pediatr Surg Int. 2000;16:550-3.
- [Google Scholar]
- Choledochal cyst following operation for idiopathic perforation of the biliary tract in childhood. Jpn J Surg. 1983;13:441-5.
- [Google Scholar]
- Spontaneous biliary perforation: Biloma resembling a small bowel duplication cyst. J Pediatr Gastroenterol Nutr. 2000;31:201-3.
- [Google Scholar]
- Spontaneous rupture of the bile duct associated with pancreatitis. A rare presentation. JOP. 2011;12:149-51.
- [Google Scholar]






