Translate this page into:
Omental Nodular Deposits of Recurrent Chromophobe Renal Cell Carcinoma Seen on FDG-PET/CT
Address for correspondence: Dr. Aung Zaw Win, Department of Radiology, San Francisco VA Medical Center, 4150 Clement Street, San Francisco, California - 94121, USA. E-mail: aungzwin@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We present the case of a 69-year-old male with chromophobe renal cell carcinoma (RCC). Chromophobe RCC accounts for only 4% of renal cancers and it is the least aggressive type. Omental nodular deposits due to RCC metastasis are very rare and it is reported only in more aggressive forms of RCC. This is the first report that shows FluoroDeoxyGlucose – Positron Emission Tomography/Computed Tomgraphy (FDG-PET/CT) images of omental nodular deposits from chromophobe RCC. FDG-PET/CT is becoming very useful in restaging RCC with distant metastases.
Keywords
Chromophobe renal cell carcinoma
FDG-PET/CT
omental caking
peritoneal carcinomatosis
INTRODUCTION

Renal cell carcinoma (RCC) makes up about 3% of all adult cancers. Cigarette smoking is a major risk factor. Incidence in males is higher than in females. In females, the disease is associated with better prognosis.[1] In the United States, Asian Americans have lower incidence rate and higher survival rate than all others.[1] According to the World Health Organization (WHO) classification, the subtypes of RCC are: Clear cell (70%), papillary (15%), chromophobe (4%), collecting duct (1%), and others (10%).[2] The chromophobe subtype is derived from the cortical collecting ducts. Most cases of chromophobe RCC arise due to a new gene mutation, without any family history of this entity. Women have a higher proportion of chromophobe RCC than men.[1] Incidence of metastatic disease in chromophobe RCC is only about 0.6%.[3] Liver and lungs are the most common sites of metastasis for chromophobe RCC. Chromophobe RCC has a favorable prognosis and a 5-year survival rate of 80-100%, compared with 20% for most RCC.[3]
CASE REPORT
Our patient is a 69-year-old Caucasian male who was diagnosed with T3aN0M0 chromophobe renal cell carcinoma (RCC) in 2011. He underwent laparoscopic total right nephrectomy. On a surveillance CT done in June 2012, he was found to have a new interaortocaval mass (2.5 cm) with some limited mesenteric stranding. He underwent lymph node dissection and during the procedure, a suspicious omental implant sample was removed and it was found to be positive for chromophobe RCC. He was treated with sunitinib and everolimus. This patient had a series of surveillance FDG-PET/CT scans. On the most recent restaging FDG-PET/CT examination done in January 2014, there was new development of omental nodular deposits with FDG avidity [Figures 1 and 2]. Furthermore, cluster of hypermetabolic omental nodularity was seen in the right inferior abdominal quadrant with a SUVmax = 4.2. Hypermetabolic osseous metastases were also seen in right ilium, left ilium, and T10 vertebral body. The patient was referred to hospice care.
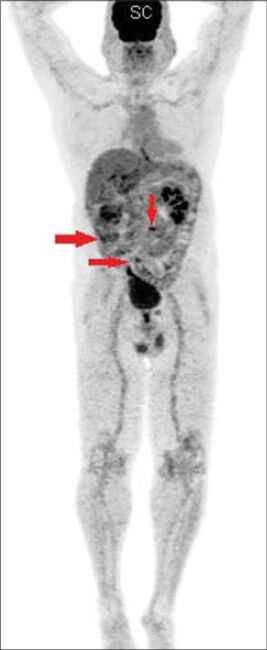
- 69-year-old male with blood in the urine was diagnosed with chromophobe renal cell carcinoma. Maximum intensity projection (MIP) image shows omental deposits from chromophobe renal cell carcinoma (arrows).
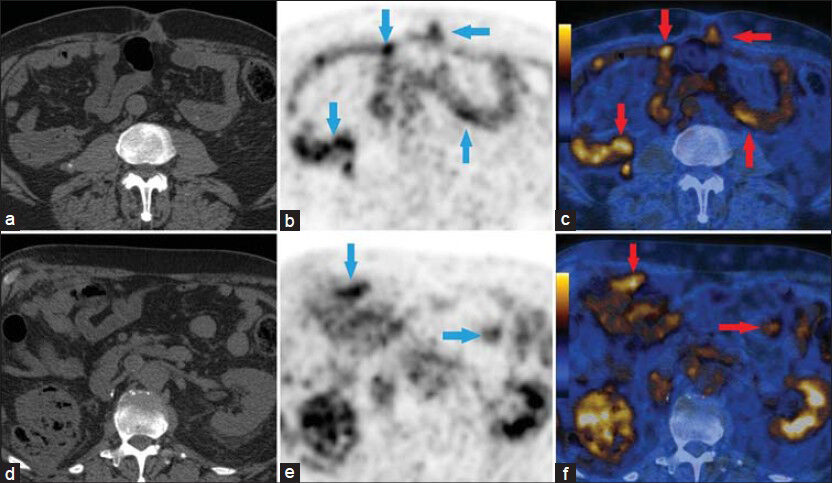
- 69-year-old male with blood in the urine was diagnosed with chromophobe renal cell carcinoma. (a) Axial CT image for attenuation correction and anatomic localization, (b and c) Axial PET/CT images show scattered focal areas of increased FDG avidity in the cecal wall and small bowel (arrows). This was consistent with serosal implants from chromophobe renal cell carcinoma, (d) Axial CT image for attenuation correction and anatomic localization, and (e and f) Axial PET/CT images show omental nodular deposits in the mid abdomen (arrows). The SUVmax was 4.6.
DISCUSSION
This is the first report that shows FDG-PET/CT images of omental nodular deposits from chromophobe RCC. Lymph node metastasis of chromophobe RCC is rare and only about 11 cases have been previously reported.[4] Most of these cases described chromophobe RCCs with sarcomatoid differentiation. Chromophobe RCC can transform to the more aggressive sarcomatoid form. In this case, omental deposits were seen without transformation to the sarcomatoid form. Peritoneal metastasis is most often associated with aggressive forms of RCC such as clear cell, papillary, granular, rhabdoid, and sarcomatoid.[2] RCC is a rare cause of peritoneal metastases, occurring in 1% of cases.[5] Peritoneal disease may present as discrete peritoneal implants, ascites or widespread omental infiltration.[5] Moderate ascites was present in our patient. Lymph node dissection is not indicated for peritoneal lymph nodes. In this patient, omental metastasis was found during retroperitoneal lymph node dissection.
Moreover, the usual RCC prognostic trends might not apply to chromophobe RCC. Most of the published papers focused on other types of RCC and Fuhrman grading is used as a prognostic indicator. Fuhrman grading is not appropriate for chromophobe RCC and more research needs to be done on chromophobe RCC.[6] Our patient had total right nephrectomy and metastasis was detected less than a year after the surgery. This shows that surgery is not curative for localized RCC. Our patient was treated with sunitinib, a tyrosine kinase inhibitor, which has been proven to be effective for peritoneal carcinomatosis.[7]
CT remains the primary imaging modality in the management of RCC. Use of intravenous (IV) contrast is contraindicated in patients with renal insufficiency and CT without IV contrast provides limited information in identifying metastases. Tumor size is an important component of TNM staging and radiological size estimation is an essential parameter to select the appropriate treatment for RCC. According to Liu et al., CT scan tends to overestimate the tumor size.[8] Furthermore, CT has a low accuracy in detecting perinephric tumor extension because stranding in the perinephric fat is nonspecific and it can be due to edema, vascular engorgement, or previous inflammation.[8] Both CT and magnetic resonance imaging (MRI) cannot identify metastasis in normal-size lymph nodes.
FDG-PET/CT has the ability to visualize the biological activity of tissues and it can clearly differentiate tumor recurrence from fibrosis or necrosis. Hepatocellular carcinoma (HCC) metastasis can present as an isolated omental lesion.[9] Thus, on FDG-PET/CT, metastases to the omentum can be seen as solitary or widespread lesions. Fuccio et al., recommended the use of FDG-PET/CT in RCC restaging because they found that the number of false-negative cases is limited.[10]
CONCLUSION
FDG is eliminated by the kidneys and this can produce a high background. This issue can be overcome by increasing diuresis with hydration or by administering diuretics. Use of furosemidelasix, is part of the protocol for renal FDG-PET/CT imaging at our institution. Thus, FDG-PET/CT is becoming a very useful tool for restaging RCC with distant metastases.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/51/141560
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Gender-specific clinicopathological features and survival in patients with renal cell carcinoma (RCC) BJU Int. 2012;110:E28-33.
- [Google Scholar]
- Cervical lymph node metastasis in chromophobe renal cell carcinoma: A case report and review of the literature. Case Rep Otolaryngol 2013 2013:814175.
- [Google Scholar]
- Prognostic value of histologic subtypes in renal cell carcinoma: A multicenter experience. J Clin Oncol. 2005;23:2763-71.
- [Google Scholar]
- Chromophobe renal cell carcinoma with prominent lymph node metastasis and polysomy of chromosome 21: Poorly differentiated form or “presarcomatoid” form? Med Mol Morphol. 2011;44:168-73.
- [Google Scholar]
- Computed tomography in metastatic renal cell carcinoma. Semin Ultrasound CT MR. 2009;30:359-66.
- [Google Scholar]
- Fuhrman grading is not appropriate for chromophobe renal cell carcinoma. Am J Surg Pathol. 2007;31:957-60.
- [Google Scholar]
- A case of advanced renal cell carcinoma with peritoneal carcinomatosis responding to sorafenib therapy. Int Canc Conf J. 2012;1:198-200.
- [Google Scholar]
- The accuracy of multidetector Computed Tomography for preoperative staging of renal cell carcinoma. Int Braz J Urol. 2012;38:627-36.
- [Google Scholar]
- Positron emission tomography/computer tomography in guidance of extrahepatic hepatocellular carcinoma metastasis management. World J Gastroenterol. 2007;13:5413-5.
- [Google Scholar]
- Restaging clear cell renal carcinoma with 18F-FDG PET/CT. Clin Nucl Med. 2014;39:e320-4.
- [Google Scholar]






