Translate this page into:
Acute Calculous Cholecystitis Missed on Computed Tomography and Ultrasound but Diagnosed with Fluorodeoxyglucose-Positron Emission Tomography/Computed Tomography
Address for correspondence: Dr. Aung Zaw Win, Department of Radiology, San Francisco VA Medical Center, 4150 Clement Street, San Francisco, CA 94121, USA. E-mail: aungzwin@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We present a case of a 69-year-old patient who underwent ascending aortic aneurysm repair with aortic valve replacement. On postsurgical day 12, he developed leukocytosis and low-grade fevers. The chest computed tomography (CT) showed a periaortic hematoma which represents a postsurgical change from aortic aneurysm repair, and a small pericardial effusion. The abdominal ultrasound showed cholelithiasis without any sign of cholecystitis. Finally, a fluorodeoxyglucose (FDG)-positron emission tomography (PET)/CT examination was ordered to find the cause of fever of unknown origin, and it showed increased FDG uptake in the gallbladder wall, with no uptake in the lumen. FDG-PET/CT can diagnose acute cholecystitis in patients with nonspecific clinical symptoms and laboratory results.
Keywords
Acute calculous cholecystitis
computed tomography
fluorodeoxyglucose-positron emission tomography/computed tomography
ultrasound

INTRODUCTION
Acute cholecystitis is caused by gallstones in the majority of cases. When a stone obstructs the gallbladder (GB) neck or cystic duct, an acute inflammation process can occur. This obstruction leads to overdistension of the GB and increased intraluminal pressure. Secondary bacterial infection may occur in some cases. The prevalence of cholelithiasis, presence of stones in the GB, is about 10–15% in the general population.[1] Among those with cholilithiasis, 1–4% will become symptomatic per year.[1] Overall, acute cholecystitis will develop in up to 30% of patients with cholilithiasis.[1] However, acute cholecystitis develops in men more frequently than would be expected from the relative prevalence of gallstones (about half that in women), and cholecystitis tends to be more severe in men.[2] In patients with diabetes, acute cholecystitis seems to develop more frequently than in patients without diabetes, and such patients are more likely to have complications of acute cholecystitis when it occurs.[2] The symptoms include right upper quadrant abdominal pain, fever, nausea and vomiting, loss of appetite, and mild jaundice. The symptoms usually occur after eating a fatty meal. The clinical symptoms and laboratory findings for acute cholecystitis are nonspecific and they can also be found in other conditions. In elderly patients, delays in diagnosis are common because physical examination and laboratory indexes may be normal.[2] Imaging plays an important role in the diagnosis of acute cholecystitis.
CASE REPORT
A 69-year old male, who underwent ascending aortic aneurysm repair with no past medical history of alcohol or tobacco abuse, hypertension, diabetes mellitus, obesity and peptic ulcer disease on day twelve postoperatively developed low-grade fever and leukocytosis. His white blood cell count was 16.60 (normal 4.8–10.8 billion cells/L). The urine culture was negative and he was started on vancomycin and ertapenem. A chest computed tomography (CT) revealed a periaortic hematoma which represents a postsurgical change from aortic aneurysm repair, and a small pericardial effusion. An ultrasound (US) examination of the abdomen was done and it showed cholelithiasis and GB sludge without evidence of cholecystitis. After this, a positron emission tomography (PET)/CT was ordered to look for any metabolic activity in the periaortic hematoma to rule out infection. The fluorodeoxyglucose (FDG)-PET/CT examination found no abnormal FDG activity in the periaortic hematoma to indicate infection. There was an incidental finding of intensely increased FDG activity within the distended GB wall, with associated mild pericholecystic fat stranding and stones in the GB neck [Figure 1]. He underwent cholecystectomy and pathology confirmed the diagnosis as acute cholecystitis.
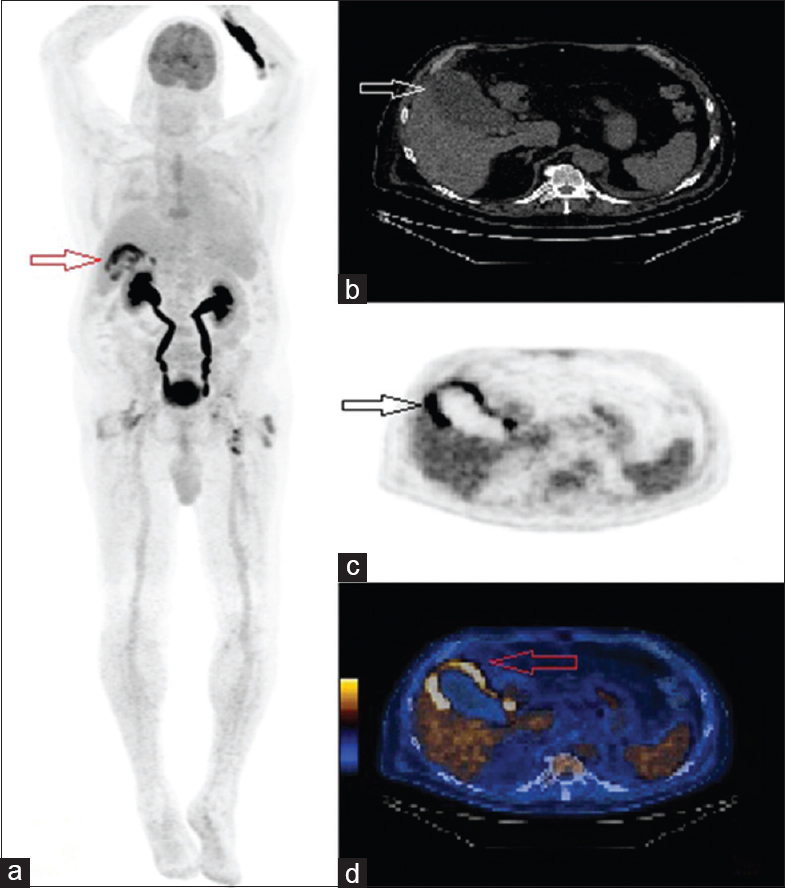
- A 69-year-old male developed low-grade fevers and leukocytosis, after ascending aortic aneurysm repair with aortic valve replacement. (a) Fluorodeoxyglucose-positron emission tomography/computed tomography maximum intensity projection image shows no signs of infection around the aorta but increased metabolic activity around the gallbladder (arrow). (b) Axial view computed tomography image shows a distended gallbladder with mild pericholecystic fat stranding (arrow). (c) Fluorodeoxyglucose positron emission tomography image and (d) hybrid fluorodeoxyglucose-positron emission tomography/computed tomography, axial views, show increased tracer uptake in the wall of the gallbladder, with no uptake in the lumen (arrows).
DISCUSSIONS
To the best of our knowledge, there are only two prior reports in the English language literature that mention the use of FDG-PET/CT to image acute calculous cholecystitis.[34] Our paper is unique; in that, we did not intend to diagnose acute cholecystitis with FDG-PET/CT. It was an incidental finding in the workup for postoperative fever of unknown origin. The abdominal US is often the first step in the workup for suspected acute cholecystitis because it is safe, widely available, and inexpensive. US is accurate for diagnosing cholilithiasis but less for diagnosing acute cholecystitis.[1] Stogryn et al., reported that US has a low negative predictive value and it can underdiagnose acute cholecystitis.[1] In the current case, the US examination found cholilithiasis but no signs of cholecystitis. A prospective study by Bingener et al., found that the sensitivity and specificity of US were 54% and 67%, respectively.[5] The same study reported that the US's ability to predict acute cholecystitis in patients with clinical symptoms appears limited.[5] Moreover, US is operator-dependent. Some patients may not have sonographic Murphy sign or GB wall thickening.[6] Our patient did not have those two signs on US. Age, diabetes mellitus, and pain medications can potentially mask a sonographic Murphy sign. Our patient was a 69-year-old diabetic who was on pain medications after the surgery. With US, a gallstone may or may not be visualized within the GB neck or cystic duct.[7] The patient must be in the prone or left lateral decubitus position, to better visualize a stone impacted in the GB neck or cystic duct. These positions can prove very difficult for Intensive Care Unit and emergency department patients. US has limited value in checking for complications of acute cholecystitis. The presence of complications can change the management.
Radionuclide scanning using 99mTechnetium-labeled hepato iminodiacetic acid (HIDA) is usually ordered after a normal US to exclude acute cholecystitis. It is a sensitive and accurate test to evaluate GB function. Riyad et al., reported that HIDA scan is very useful in early diagnosis of biliary pain in patients who have a normal abdominal US.[8] However, our patient had no complaints of abdominal pain, and acute cholecystitis was not suspected at first and HIDA scan was not ordered. CT is suitable for evaluating the complications of acute cholecystitis. A significant fraction of mixed, cholesterol or pigment stones are similar in attenuation to bile and may not be detected on CT.[9] In addition, sludge in the GB can hide the gallstones. In the present case, our patient had an almost normal CT except for postsurgical changes and a small pericardial effusion. Similar to our case, Fidler et al., reported that many of their patients had normal or nearly normal CT scans.[10] Thus, acute cholecystitis cannot be ruled out in the absence of CT findings.[10] In a mild form or early manifestation of acute cholecystitis, the CT may be normal and inflammatory changes may be absent on CT in early stages of acute cholecystitis.
US and CT rely on physical features to make a diagnosis. PET/CT provides both anatomical and functional imaging information and it can scan the whole body in one examination everywhere to assess for possible complications after the surgery. Since it relies on detecting the changes in metabolic activity of tissues, it can detect pathology even before anatomic changes are apparent. In acute cholecystitis, there is an increased blood flow from the cystic artery to the GB wall. FDG is taken up by activated inflammatory cells in the GB wall. In the current case, there was an increased FDG uptake in the GB wall, with no uptake in the lumen. This is called the rim sign, and the description is consistent with the previously reported findings of acute cholecystitis on FDG-PET/CT.[34] In contrast, in GB cancers, the FDG uptake is either focal or it fills up the GB, with no photopenic areas.[11] Thus, FDG-PET/CT can distinguish between benign and malignant lesions in the GB. Finally, the patients can undergo multiple imaging studies for evaluation of acute cholecystitis before cholecystectomy. Our case has shown that FDG-PET/CT can eliminate the need for multiple examinations and the delay in treatment.
CONCLUSION
The present case report has shown that both US and CT can miss acute cholecystitis. FDG-PET/CT can diagnose acute cholecystitis in patients with nonspecific clinical symptoms and non-specific imaging results. It is useful in the workup for fever of unknown origin in postoperative patients. It can avoid multiple imaging studies and save associated costs. It has the potential to reduce delays in the treatment. FDG-PET/CT has a promising role in the management of acute cholecystitis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/31/188474
REFERENCES
- Does ultrasongraphy predict intraoperative findings at cholecystectomy? An institutional review. Can J Surg. 2016;59:12-8.
- [Google Scholar]
- Does the correlation of acute cholecystitis on ultrasound and at surgery reflect a mirror image? Am J Surg. 2004;188:703-7.
- [Google Scholar]
- Increased enhancement of the liver adjacent to the gallbladder seen with contrast ultrasound: Comparison between acute cholecystitis and non-cholecystitis. BMC Med Imaging. 2016;16:21.
- [Google Scholar]
- Cross-sectional imaging of acute and chronic gallbladder inflammatory disease. AJR Am J Roentgenol. 2009;192:188-96.
- [Google Scholar]
- The role of (99m) technetium-labelled hepato imino diacetic acid (HIDA) scan in the management of biliary pain. HPB (Oxford). 2007;9:219-24.
- [Google Scholar]
- CT findings of acute cholecystitis and its complications. AJR Am J Roentgenol. 2010;194:1523-9.
- [Google Scholar]
- CT evaluation of acute cholecystitis: Findings and usefulness in diagnosis. AJR Am J Roentgenol. 1996;166:1085-8.
- [Google Scholar]
- PET/CT evaluation of the physiologic accumulation of 18F-FDG within the gallbladder vesicle. Nucl Med Biol. 2007;34:961-6.
- [Google Scholar]






