Translate this page into:
Mandibular Canal Enlargement: Clinical and Radiological Characteristics
Address for correspondence: Dr. Chong Jun Ai, International Medical University, Faculty of Dentistry, 126, Jln Jalil Perkasa 19, 57000 Bukit Jalil, Wilayah Persekutuan, Kuala Lumpur, Malaysia. E-mail: chongjunai@imu.edu.my
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Enlargement of the mandibular canal is a rare radiological finding. Clinically, it may or may not be associated with sensory deficits. We report four cases of widening of the mandibular canal observed with various methods of imaging with different clinical characteristics. We describe this unique radiological finding and elaborate the importance of quality assessment of the imaging that is vital for accurate diagnosis and treatment planning. Clinicians should be mindful when assessing the imaging whenever the size of the mandibular canal is implicated. The case ranged from a benign tumor to malignancy, radiological errors, and artifacts. A more superior imaging or treatment modality was necessary to ascertain the diagnosis.
Keywords
Clinical characteristics
imaging characteristics
mandibular canal

INTRODUCTION
The mandibular nerve is a branch of the third division of the trigeminal nerve which innervates the mandibular teeth, labiomental region, buccal gingiva, and mucosa of the premolars to the midline.[1] It enters the mandibular foramen on the medial surface of the ramus, transverses through the mandibular canal and exits the mandible anteroinferiorly through the mental foramen.[2] The course of the mandibular canal is a vital surgical landmark that is best visualized through axial and panoramic reconstructed images.[2] It is usually assessed before procedures involving the mandible, such as surgical removal of mandibular third molars and dental implant placement to avoid neurovascular bundle injuries.[2]
Although the mandibular canal has variations such as bifid and trifid canals, it is generally known to be a single structure with a diameter of 2–2.4 mm bilaterally in the mandible.[3] Radiographically, it appears as a dark, linear shadow between two thin radiopaque borders.[45] Enlargement of the mandibular canal is a rare radiological finding and may be associated with sensory deficits.[1] The type of pathological changes that occur to the mandibular canal may in themselves aid diagnosis.[5] Ill-defined widening of the mandibular canal usually depicts malignant infiltration such as lymphoma whereas unilocular, well-defined, rounded enlargement usually arises from benign lesions such as schwannoma.[1] Meanwhile, in 6% of cases, intraosseous vascular malformations have shown calcified phleboliths or cortical erosion of bone, but generally, plain radiographs are not the imaging of choice.[6]
We report four unusual cases of widening of the mandibular canal that presented with different clinical characteristics. The clinical implication of these cases is also discussed.
CASE REPORTS
Case 1
A 57-year-old female presented with sudden onset of loss of taste and tongue deviation to the left on protrusion. She had slurring of speech but no limb weakness, no syncopal attack, no headache, no vomiting, and no history of seizure. Underlying medical problems revealed that she suffered from hypertension, psoriasis, and right knee osteoarthritis. She was first seen by the neurosurgery team as the computed tomography (CT) scan showed right posterior frontal-subcortical intraparenchymal bleed with multifocal infarcts. A magnetic resonance imaging (MRI) was also performed and there was an incidental finding of right masticator space lesion following the course of the right mandibular nerve. The patient was then referred to us for further management.
On examination, her face was symmetrical. She had slurred speech, tongue deviation to the left but no paresthesia of her tongue or right labiomental region. There was no buccal or lingual bony expansion at the right mandible. However, thick fibrous mucosa was palpable lingually.
The panoramic radiograph showed enlarged well-defined radiolucency zone of the right mandibular canal measuring 8.6 mm compared to the left side which measures 2.3 mm. There was also loss of cortication of the mandibular canal [Figure 1].
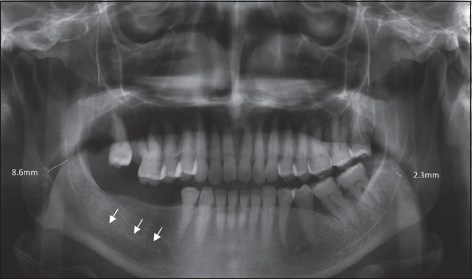
- 57-year-old female with cerebrovascular accident who presented with sudden onset of loss of taste and tongue deviation. Panoramic radiograph showing widening of the right mandibular canal (arrows).
Cone-beam CT (CBCT) confirmed the above radiological findings with intact, uninterrupted cortication of the mandibular canal only at the superior border [Figure 2].
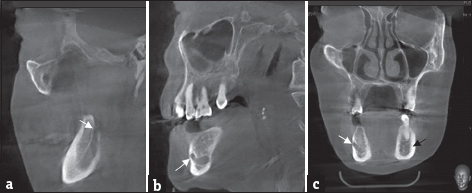
- 57-year-old female with cerebrovascular accident who presented with sudden onset of loss of taste and tongue deviation. Cone-beam computed tomography image showing various tomographic views. (a and b) Sagittal view showing enlargement of the mandibular canal from the mandibular foramen (white arrow) toward the mental foramen (white arrow). (c) Coronal view comparing the size of the mandibular canal bilaterally (white arrow: Right canal, black arrow: Left canal).
The MRI scan showed well-defined T1-hypointense and T2-hyperintense lesion at the right masticator space invaginating into the right mandibular canal measuring 2.6 cm × 1.7 cm × 3.4 cm (AP × W × L) [Figure 3]. It had minimal central enhancement seen postcontrast. No evidence of intracranial perineural spread.

- 57-year-old female with cerebrovascular accident who presented with sudden onset of loss of taste and tongue deviation. Magnetic resonance imaging showing well-defined T1-hypointense and T2-hyperintense lesion at the right masticator space invaginating into the right mandibular canal at axial section (white arrow).
Impression of the lesion radiographically was either schwannoma or neuroma. The patient declined incisional biopsy to establish the diagnosis of the lesion as she was asymptomatic and unwilling to take the risk of paresthesia postbiopsy.
Case 2
A 60-year-old female was referred to us for the left lateral access mandibulotomy for an open biopsy to a left infratemporal lesion found on CT scan in June 2014. She had a history of toothache at a left mandibular molar tooth which was extracted approximately a year earlier. The patient subsequently developed hypoesthesia 2-week postextraction at the left angle of mandible to the neck. She previously underwent transoral alveolar bone biopsy in a nearby hospital of which the report came back as osteomyelitis and she was treated with multiple long duration of antibiotics. Her condition worsened further with progressive trismus and left otalgia. A left mastoid exploration was performed in February 2014 under the ear, nose, and throat department. She developed House–Brackmann Classification V left facial nerve palsy complication from the surgery.
On examination, she had left facial asymmetry. She was unable to close her left eye fully but no conjunctival ulcer present. She had left lower lip hypoesthesia and drooling. Her mouth opening was 2 cm measured intrinsically. Her gag reflex was positive. There was no mandibular bowing at the angle region, no shallowing of buccal sulcus or tenderness bilaterally at the mandible. The mucosa at the left mandibular posterior alveolar ridge was intact.
The panoramic radiograph [Figure 4] showed multiple root treated teeth with complex crown and bridgework. There was ill-defined, enlarged radiolucency along the left mandibular canal measuring about 7.7 mm.

- 60-year-old female with squamous cell carcinoma who presented with left lower lip hypoesthesia. Panoramic radiograph showing ill-defined widening of the left mandibular canal (white arrows).
Meanwhile, the CT scan showed hyperintense lesion over the left infratemporal fossa mass involving the pterygoid muscle and deep lobe of the left parotid gland. There was widening of the mandibular canal region extending to the mental foramen. There was cortical irregularity with periosteal reaction of the medial aspect of the left mandible [Figure 5].
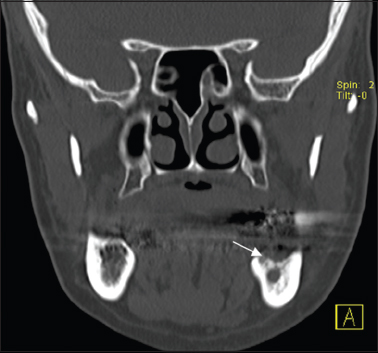
- 60-year-old female with squamous cell carcinoma who presented with left lower lip hypoesthesia. Sagittal view of the computed tomography scan showing cortical irregularity with periosteal reaction of the medial aspect of the left mandible (white arrow).
The MRI showed ill-defined heterogeneous enhancing mass in the left infratemporal fossa. The mass extended down to the left angle of mandible with extension along the mandibular canal [Figure 6].
- 60-year-old female with squamous cell carcinoma who presented with left lower lip hypoesthesia. Axial view of the magnetic resonance imaging showing the mass extending to the left angle of mandible and into the mandibular canal (white arrows).
Both alveolar cortical bone and the left infratemporal lesion were concurrently biopsied and reported as differentiated squamous cell carcinoma. She subsequently underwent left hemimandibulectomy and superficial parotidectomy. She, however, finally succumbed to her disease.
Case 3
An 86-year-old male was referred for the management of lingual nerve injury after surgical removal of the left third mandibular molar. He complained of reduce taste sensation over his tongue with reduce oral intake. In addition, he claimed to have numbness over his left lower lip and tip of his tongue that only developed after 3 weeks postoperatively. He had diabetes mellitus type 2 complicated with neuropathy over bilateral hands and feet and an underlying dyslipidemia.
On examination, he had no facial swelling and good mouth opening. There was hypoesthesia to soft touch at the lower left lip, left buccal gingiva and mucosa, and tip of the tongue but he was able to differentiate sharp and blunt objects. The extraction socket was in healing progress with no signs of infection and no bony exposure.
A panoramic radiograph was taken and noted widening of the left mandibular canal measuring 5.1 mm compared to the right side which measures 2.5 mm [Figure 7]. There was a retained root of tooth 36 and generalized sclerosis of the mandible. On further close assessment from this imaging, it was noticeable that there was gross widening of the upper left teeth and reduced quality at the anterior region.

- 86-year-old male with reduced taste sensation of the left lower lip and tongue. Panoramic radiograph showing widening of the left mandibular canal (white arrows).
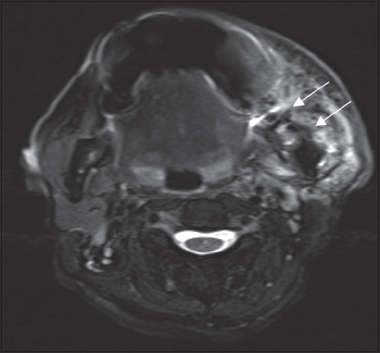
MRI brain which was performed showed that the mandibular canal was of normal configuration. Incidentally, there was T1-hyperintense signal seen at the cortical region of the left frontal lobe and hypointense on T2 representing laminar necrosis. Comparison of the trigeminal nerve bilaterally revealed no asymmetry.
Case 4
A 34-year-old male presented for minor oral surgery of the left mandibular third molar (tooth 38) due to recurrent pericoronitis since a year ago. Clinically, tooth 38 was partially erupted with tenderness on the buccal gingiva. A panoramic radiograph was requested.
On reviewing the panoramic radiograph, the radiographic appearance of another possible mandibular canal was highly suspected with the continuation of this canal to the anterior loop before exiting at the mental foramen [Figure 8].
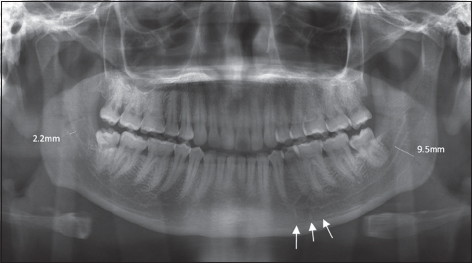
- 34-year-old male with left recurrent pericoronitis. Panoramic radiograph showing “double mandibular canal” (white arrows).
CBCT was performed to further evaluate the proximity of the mandibular nerve to tooth 38. The CBCT [Figure 9] showed that the canal is a single mandibular canal and not a bifid canal as appeared in the panoramic radiograph.
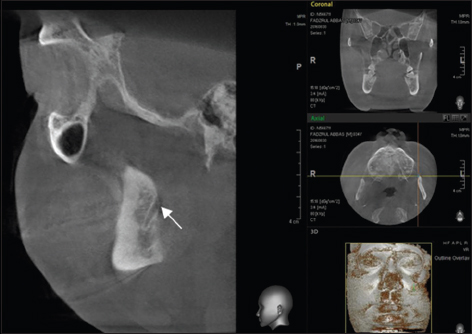
- 34-year-old male with left recurrent pericoronitis. Sagittal section of the cone-beam computed tomography showing a single mandibular canal (white arrow).
DISCUSSION
Anatomic variations of the mandibular canal could be detected by panoramic radiographs.[1] However, quality assessment of radiographs is important to avoid any misinterpretation that could lead to misdiagnosis and improper treatment planning.[78]
This case series discussed a range of causes of enlargement of the mandibular canal from radiographic artifact to anatomical variation and finally, benign and malignant tumors.
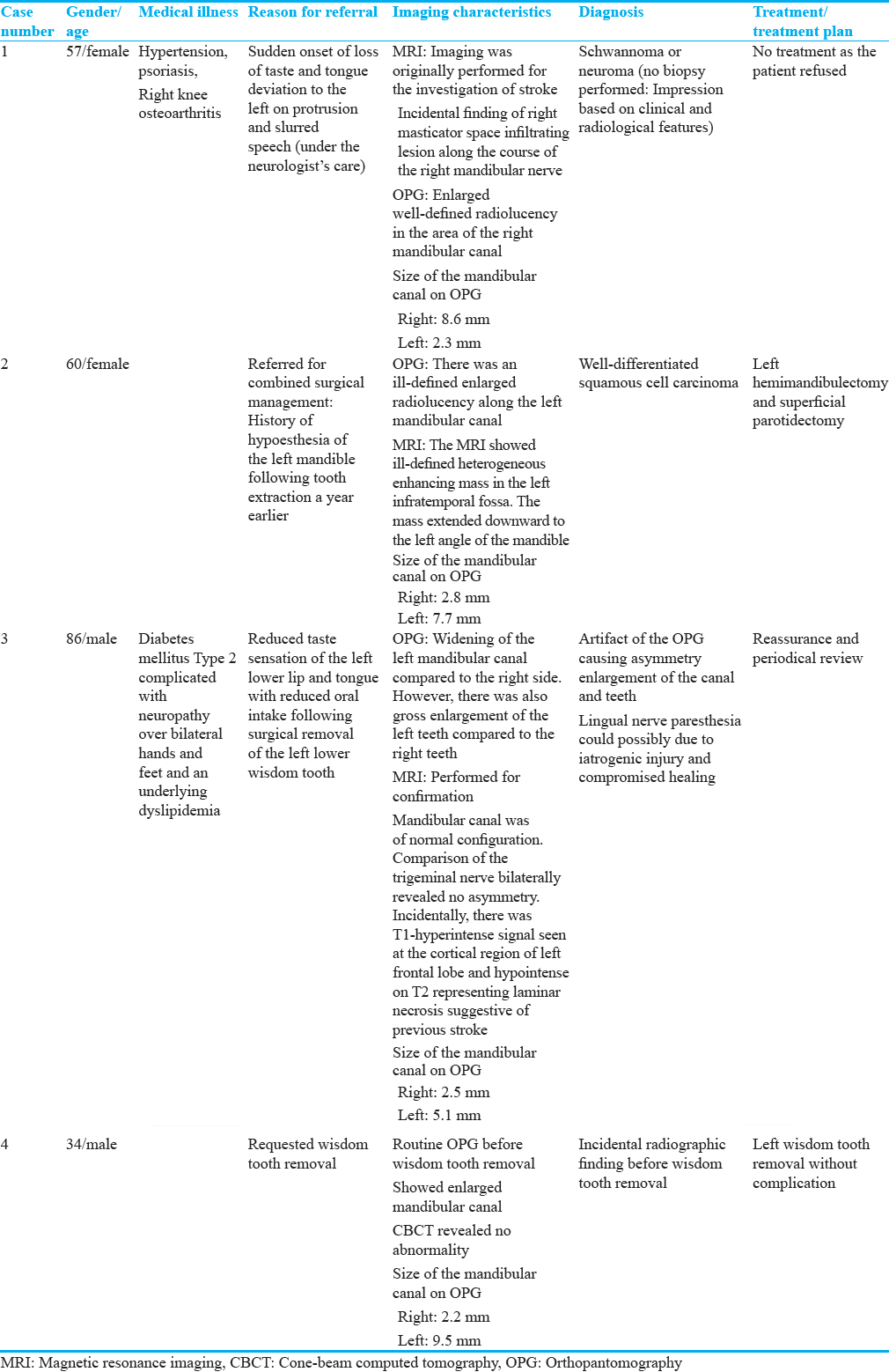
Table 1 summarizes the clinical and imaging characteristics of the cases.
Radiographic artifact could occur due to error in positioning[8] as observed in Case 3. The patient's head was rotated to the right side leading to wider teeth on the left side and an increase overlapping of contact points. In addition, the condyle and ramus were much wider on the left side.[8] In general, there was uneven pattern of blurring throughout the arch and narrowing at the right parasymphysis region,[8] which should raised the index of suspicion in regards to the panoramic positioning error. If an error occurs, a repeat same radiograph or another superior imaging should be requested.
Tumors whether benign or malignant, need to be ruled out by thorough clinical and imaging assessment. In Case 1, the radiographic appearance of an enlarged well-defined unilocular radiolucent lesion of the mandibular canal gave an impression of a schwannoma. It is occasionally associated with root divergence if expansive growth or root resorption in teeth contacting the lesion.[9] It represents less than 1% of primary benign bone tumors.[910] It is usually asymptomatic but may cause bony swelling, pain, or paresthesia after a few years as the lesion slowly progressively grows in size.[910] There are three possible mechanisms which could explain the onset of the tumor, that is, a tumor arising centrally within the bone or the nutrient canal producing canal enlargement or a periosteal tumor causing secondary erosion and penetration into bone.[91011]
Histopathological investigation of the mandibular canal enlargement is highly advised even in asymptomatic cases to rule out malignancy such as lymphoma.[12] Injury to the nerve is unavoidable during surgical intervention. Temporary or permanent lingual sensory disturbances leading to hypoesthesia with taste alterations could be similar following surgical removal of the third molar.[13]
In Case 1, the tongue deviation to the opposite side of the lesion rules out hypoglossal nerve palsy because hypoglossal schwannomas would cause ipsilateral atrophy of the tongue and deviation of the tongue to the side of the lesion.[1415] This is confirmed with the absence of the lesion along the hypoglossal canal from the intraaxial, cisternal, and skull base to extracranial segments.[16] The tongue deviation is attributed to the right posterior frontal-subcortical intraparenchymal bleed affecting the upper motor neurons which is contralateral to the paralyzed genioglossus muscle.
In Case 2, the findings of perineural spread of oral squamous cell carcinoma along the mandibular canal were rare as it usually occurs by local invasion and lymphatic spread.[17] Spread of malignant cells into the mandibular canal often arises at edentulous areas of the mandible which has cortical defects.[17] However, apart from the history of toothache, there was no other intraoral findings that could suggest a malignant lesion of oral mucosa origin. Neurological deficits denote perineural invasion whereas pain may be due to secondary infection of the lesion which undergoes repeated irritation of the nerve endings.[17] Although the CT scan revealed the mass in the ipsilateral infratemporal fossa and warrant further biopsy, a similar change was already seen within the left mandible and left mandibular canal. This implied that her dental surgeon could have first detected the lesion on observing the radiological signs from her panoramic radiograph and a biopsy could be advised through a transoral approach.
In the last case, Case 4, the illusion of a bifid mandibular canal as seen in Figure 8 could not possibly due to the superimposition of a deep mylohyoid groove as reported in some cases of misinterpretation of bifid mandibular canals.[18] This was because the third radiopaque line is located close to the inferior border of the mandible and not in the region of the apex of the mandibular teeth. Moreover, the third radiopaque line was well defined and not corticated to be considered a border of the mandibular canal. Misinterpretation of bifid mandibular canals in panoramic X-rays may lead to overestimation of the presence of it and thus, further three-dimensional radiographic examination is advocated.[18]
CONCLUSION
Widening of the mandibular canal is a rare radiological finding. Quality assessment of radiographs is vital before interpretation to avoid misdiagnosis. Further three-dimensional radiographic examination is advised for better imaging outcome. Histopathological examination of suspicious lesions that cause enlargement of the mandibular canal is suggested although mandibular nerve injury is often implicated.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/28/210637
REFERENCES
- Widening of the inferior alveolar canal: A case report with atypical lymphocytic infiltration of the nerve. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e35-9.
- [Google Scholar]
- Evaluation of the inferior alveolar canal for cysts and tumors of the mandible-comparison of multidetector computed tomography and 3-dimensional volume interpolated breath-hold examination magnetic resonance sequence with curved multiplanar reformatted reconstructions. J Oral Maxillofac Surg. 2012;70:2327-32.
- [Google Scholar]
- Anatomy of mandibular vital structures. Part I: Mandibular canal and inferior alveolar neurovascular bundle in relation with dental implantology. J Oral Maxillofac Res. 2010;1:e2.
- [Google Scholar]
- Bifid mandibular canals: Prevalence and implications. J Oral Maxillofac Surg. 2015;73:387-90.
- [Google Scholar]
- Entrapment of the inferior dental nerve by a 3-rooted mandibular third molar - Case report. Asian J Oral Maxillofac Surg. 2002;14:105-8.
- [Google Scholar]
- Management of mandibular vascular malformation with sclerotherapy. Report of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:99-103.
- [Google Scholar]
- Positioning errors and quality assessment in panoramic radiography. Imaging Sci Dent. 2012;42:207-12.
- [Google Scholar]
- Common positioning errors in panoramic radiography: A review. Imaging Sci Dent. 2014;44:1-6.
- [Google Scholar]
- Progressively enlarging inferior alveolar nerve canal radiolucency - Schwannoma? A rare intraosseous lesion. IJSS Case Rep Rev. 2015;2:10-2.
- [Google Scholar]
- Intrabony schwannoma of the mandible: Case report and review of literature. Open J Stomatol. 2014;4:233-7.
- [Google Scholar]
- Intraosseous schwannoma originating in inferior alveolar nerve: A case report. Bull Tokyo Dent Coll. 2013;54:19-25.
- [Google Scholar]
- Enlargement of mandibular canal without hypesthesia caused by extranodal non-Hodgkin's lymphoma: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:388-92.
- [Google Scholar]
- Lingual nerve injury after third molar removal: Unilateral atrophy of fungiform papillae. J Clin Exp Dent. 2014;6:e193-6.
- [Google Scholar]
- Hypoglossal schwannoma: A case report and review of literature. Iran J Otorhinolaryngol. 2011;23:45-50.
- [Google Scholar]
- Isolated hypoglossal nerve schwannoma: An uncommon presentation of schwannoma. J Clin Diagn Res. 2015;9:TJ01-2.
- [Google Scholar]
- Assessment of perineural infiltration and spread of oral squamous cell carcinoma: A clinicohistopathologic study. Indian J Cancer. 2010;47:199-205.
- [Google Scholar]
- CBCT finding of double bifid inferior alveolar canals: Literature review and case report. EC Dent Sci. 2015;1:90-7.
- [Google Scholar]






