Translate this page into:
Uterine Lipoleiomyoma: A Report of Two Cases
Address for correspondence: Dr. Haji Mohammed Nazir, Flat No - 226, Alsa Townsville, 38/170, Arcot Road, Valasravakkam, Chennai, Tamil Nadu, India. E-mail: hajimohamed867@yahoo.co.in
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report two cases of uterine lipoleiomyoma in postmenopausal women of ages 52 and 55 years, who presented with complaints of leukorrhea and lower abdominal pain, respectively. Lipoleiomyoma is a rare benign variant of leiomyoma, having an incidence of 0.03%–0.2%. These are benign pelvic tumors which are usually asymptomatic and commonly occur in obese postmenopausal women. However, they can occasionally present with typical leiomyoma symptoms. Imaging plays a crucial role in the diagnosis of benign pelvic tumors. Ultrasonography is the first imaging modality for diagnosis of pelvic tumors in females. Computed tomography and magnetic resonance imaging are specific in demonstrating the uterine origin and fat component.
Keywords
Benign
leiomyoma
lipoleiomyoma
postmenopausal
uterine

INTRODUCTION
Leiomyomas or fibroids are commonly seen tumors of the uterus that originate from the smooth muscle layer of the uterine wall, with a high incidence rate in the reproductive age group.[1] Lipoleiomyomas are benign variants of leiomyomas occurring due to the fatty metamorphogenesis of their smooth muscle cells.[2345] These lipoleiomyomas are composed of variable amounts of adipocytes and smooth muscle cells, separated by thin fibrous tissue. Other lipoid tumors of the uterus include pure lipomas and fibrolipomyoma. Improved understanding and imaging diagnosis of the tumor can prevent unnecessary invasive procedures.
CASE REPORTS
Case 1
A 52-year-old postmenopausal multiparous woman presented with complaints of leukorrhea for 2 months. There was no history of bleeding per vaginum, abdominal distension, abdominal pain, or fever. She had attained menopause 7 years prior and had no known comorbid conditions, no previous history of any surgeries or any significant family history.
On physical examination, her vitals were stable. Abdominal examination revealed a firm, nontender mass of 15 weeks size in the left lower quadrant. Routine hematological investigations were within normal limits.
Ultrasonography (USG) was done for the patient transabdominally and transvaginally. Upper abdomen revealed fatty liver and no other significant abnormality. Pelvic and transvaginal USG showed an enlarged uterus of size 17.6 cm × 10.9 cm × 11.6 cm with a large, well-defined, uniformly hyperechoic lesion of size ~11.4 cm × 10.6 cm × 8.8 cm in the uterine fundus myometrium with minimal peripheral vascularity. No evidence of calcification was noted within [Figure 1].
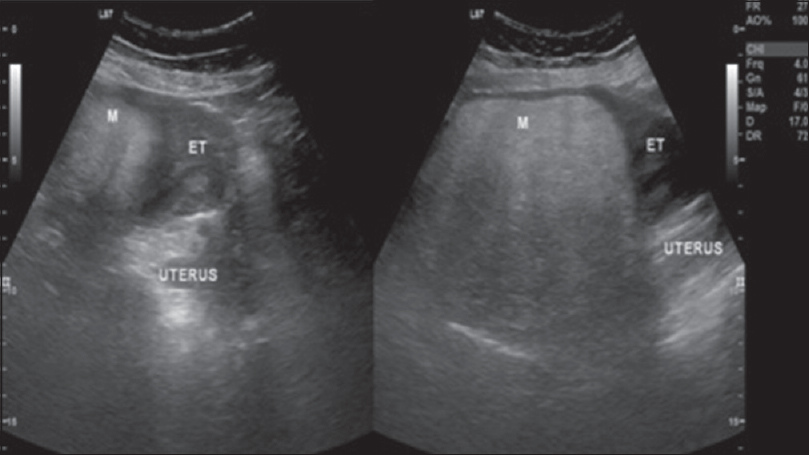
- A 52-year-old female presenting with leukorrhea for 2 months. Longitudinal ultrasound images of the pelvis demonstrate a large echogenic mass in the fundus of the uterus.
Computed tomography (CT) showed an enlarged uterus with a well-circumcised predominantly fat-containing lesion with regular margins arising from the uterine fundus. No evidence of calcification was noted within [Figure 2].

- A 52-year-old female presenting with leukorrhea for 2 months. Computed tomography plain axial section of the pelvis demonstrates a predominantly low attenuation mass, corresponding to fat density in the fundus of the uterus.
Her further work up by magnetic resonance imaging (MRI) showed an enlarged uterus with a well-marginated mass of size 11.5 cm × 10.5 cm × 9 cm within the uterine fundus subserosal myometrium, predominantly hyperintense on T1 and T2 and hypointense on T2 fat suppression sequences [Figure 3], consistent with a diagnosis of lipoleiomyoma.
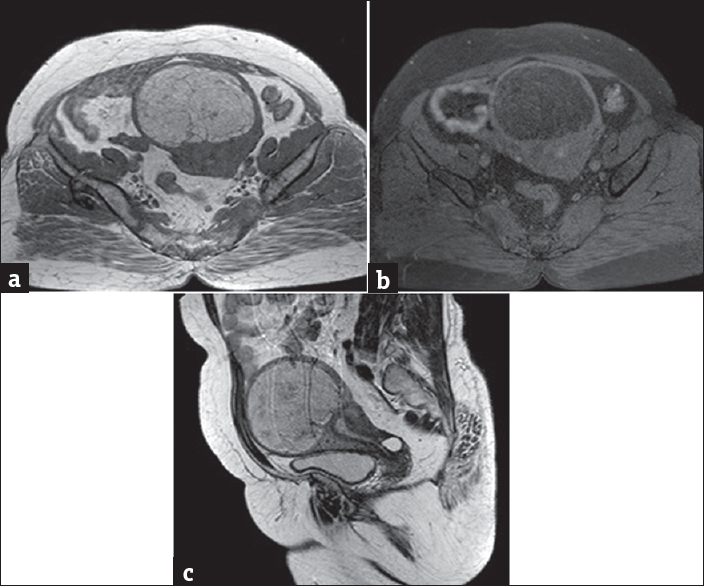
- A 52-year-old female presenting with leukorrhea for 2 months. (a) Magnetic resonance imaging T1-weighted image axial section of the pelvis demonstrates a large T1 hyperintense mass in the uterine fundus subserosal myometrium. (b) Magnetic resonance imaging T2 fat suppression sequence axial section of the pelvis demonstrates a predominantly hypointense mass in the uterine fundus subserosal myometrium. (c) Magnetic resonance imaging T2-weighted image sagittal section of the pelvis demonstrates a large T2 hyperintense mass in the uterine fundus subserosal myometrium.
In view of large lipoleiomyoma, surgery was advised, but the patient opted for conservative treatment with follow-up imaging.
Case 2
A 55-year-old postmenopausal woman presented with complaints of lower abdominal distension for 6 months. There was no history of discharge per vaginum, abdominal pain, or fever.
On physical examination, her vitals were stable. Abdominal examination revealed a firm, nontender mass of 12 weeks size in the right lower quadrant. Routine hematological investigations were within normal limits.
Ultrasound was done in another institute which revealed enlarged uterus with a large echogenic mass in uterine fundus. The patient was referred to our institute for further evaluation of the uterine mass. CT plain and contrast abdomen was done which showed an enlarged uterus of size 13.2 cm × 7.7 cm × 7.3 cm with a large, predominantly fat density mass lesion of size 6.3 cm × 6.1 cm × 6.3 cm in the myometrium of the uterine fundus with nonenhancing soft tissue strands noted within [Figure 4]. Both ovaries were atrophied.
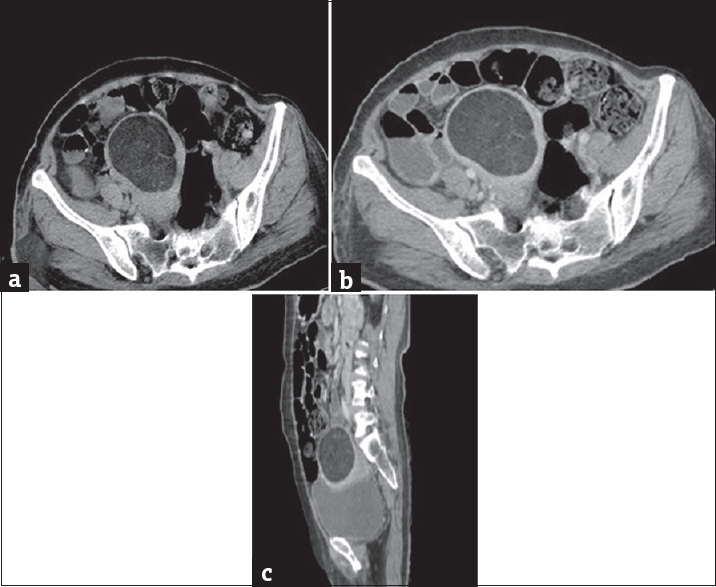
- A 55-year-old female presenting with lower abdominal distension for 6 months. (a) Computed tomography plain axial section of pelvis demonstrates a predominantly low attenuation mass, corresponding to fat density in the uterine fundus. (b) Computed tomography contrast axial image of pelvis demonstrates a predominantly low attenuation mass, corresponding to fat density in the myometrium of the uterine fundus with few nonenhancing soft tissue strands noted within. (c) Computed tomography contrast sagittal image of the pelvis demonstrates a predominantly low attenuation mass, corresponding to fat density in the myometrium of the uterine fundus with few nonenhancing soft tissue strands noted within.
Based on the CT findings of predominantly fatty component with some areas of soft tissue density, diagnosis of lipoleiomyoma was made.
Since the patient was asymptomatic, except for abdominal distention, she was managed conservatively with follow-up imaging.
DISCUSSION
Lipomatous tumors of the uterus can be classified into three types:
-
Pure lipomas – composed of encapsulated mature fat cells
-
Lipomas with mesodermal components
-
Lipoleiomyoma
-
Angiomyolipoma
-
Fibromyolipoma
-
-
Liposarcoma – the exceedingly rare and malignant type.[6]
Uterine lipoleiomyomas are rare benign tumors, having an incidence of about 0.03%–0.2%.[135678910] They are said to be subsets of leiomyomas with fatty metamorphosis of smooth muscle cells into adipose tissue.[112345] Other theories suggest that these tumors may arise due to misplaced remnants of fatty cells of the embryo, due to the extension of retroperitoneal or peritoneal fat perivascularly, due to fatty infiltration of the connective tissue, or due to the transformation of mesenchymal totipotent cell.[312] Studies show that an increased estrogenic state may also be a contributing factor. Hence, alteration in the lipid metabolism with menopause may have a role in its development. Furthermore, these patients commonly suffer from metabolic disorders such as hypothyroidism, hyperlipidemia, and diabetes mellitus.[67]
They are often seen in postmenopausal women[67913] who remain either asymptomatic or present with symptoms similar to those of uterine leiomyomas such as bleeding per vaginum, abdominal pain, palpable abdominal mass, increased frequency of urine, and urinary incontinence. They present usually as solitary enlarged masses of varying sizes with the common site of occurrence in the corpus of the uterus; however, they have also been known to occur in the cervix, broad ligament, retroperitoneum, and ovary.[14]
Imaging by USG commonly shows a well-defined hyperechoic mass surrounded by a hypoechoic rim, which may suggest a strip of myometrium around the fatty component. Vascularity is often poor.[67]
CT usually shows a well-marginated, dense mass with predominantly fatty component.[679]
MRI is the imaging modality of choice and shows a well-circumcised mass which is hyperintense on T1 with a peripheral hypointense rim. It also appears hyperintense on T2. Confirmation can be done by fat suppression sequence which shows a hypointense mass.[6715]
Chemical shift imaging, based on the innate differences in the inherent magnetic field experienced by the protons in fat molecules compared with those in water molecules, can also be used for confirmation of fat. Using Dixon method of chemical shift imaging, fat-only image is acquired showing hyperintense fatty component.[16]
Differential diagnosis of lipoid pelvic tumors can be benign ovarian teratoma, benign pelvic lipoma, fatty lymphadenopathy, degeneration of leiomyoma, retroperitoneal cystic hamartoma, and well-differentiated liposarcoma.[67914] Among the differentials, the most common one is benign cystic ovarian teratoma, which requires surgical excision.
Asymptomatic uterine lipoleiomyoma, due to its benign nature, can be managed conservatively. Hence, accurate diagnosis of lipoma/lipoleiomyoma of the uterus and their differentiation from various other fat-containing pelvic tumors are important in the management of the patient and can prevent unnecessary surgical excision.[17] Treatment of a lipoleiomyoma generally depends on the symptoms the patient presents with and the size of the mass. In symptomatic patients with large masses, the symptoms are resolved by medical management with painkillers and hormone regulation pills. Surgical options include myomectomy, hysterectomy, myolysis, tumor embolization, and radiofrequency ablation.
CONCLUSION
Uterine lipoleiomyomas may symptomatically present as leiomyomas and can be difficult to differentiate if found extrauterine on imaging.
Fatty component of lipoleiomyomas is more specific on CT and MRI when compared to USG. MRI, with its multiplanar capabilities, high sensitivity, and specificity to fat and tissue characterization, is the modality of choice for confirmation of diagnosis.
Thus, awareness of lipoleiomyoma, its clinical presentation, and imaging features is important to avoid unnecessary surgeries as it has an excellent prognosis, especially when asymptomatic.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/26/209092
REFERENCES
- Uterine lipoleiomyoma: A histopathological review of 17 cases. Pathol Int. 2004;54:751-8.
- [Google Scholar]
- Lipomatous tumors of the uterus. Clinico-pathological features of 10 cases with immunocytochemical study of histogenesis. Pathol Res Pract. 1994;190:378-83.
- [Google Scholar]
- Uterine lipoleiomyoma: A case report of a rare entity. Int J Appl Basic Med Res. 2016;6:134-6.
- [Google Scholar]
- Diagnostic challenge of lipomatous uterine tumors in three patients. World J Radiol. 2012;4:58-62.
- [Google Scholar]
- Uterine lipoleiomyoma: MRI, CT and ultrasonographic findings. Br J Radiol. 1997;70:1068-70.
- [Google Scholar]
- Clinical and pathological features of lipoleiomyoma of the uterine corpus: A review of 76 cases. Balkan Med J. 2014;31:224-9.
- [Google Scholar]
- MRI findings of uterine lipoleiomyoma correlated with pathologic findings. AJR Am J Roentgenol. 2007;189:W100-4.
- [Google Scholar]
- Lipomatous uterine tumors: Diagnosis by ultrasound, CT, and MR. J Comput Assist Tomogr. 1990;14:629-32.
- [Google Scholar]






