Translate this page into:
Uterine Lipoleiomyoma in the Context of Adenocarcinoma

-
Received: ,
Accepted: ,
How to cite this article: Rasmussen T, Sanchirico P, Pfeiffer D. Uterine lipoleiomyoma in the context of adenocarcinoma. J Clin Imaging Sci 2020;10:82.
Abstract
We describe a case of a 63-year-old woman referred to an oncologist for treatment of endometrial adenocarcinoma. A computed tomography scan revealed the incidental finding of a 11.5 × 10.5 × 9.0 cm myomatous mass in the uterine corpus adjacent to, yet uninvolved with, the adenocarcinoma. Histopathological analysis confirmed the mass to be a lipoleiomyoma, a rare single variant of lipoma. These fatty tumors present similar to leiomyomas and as such are generally not harmful; however, the potential exists for diagnostic confusion with other uterine tumors. This case serves to further illuminate the findings associated with these rare tumors.
Keywords
Lipoleiomyoma
Uterine tumor
Lipoma
Lipomyoma
INTRODUCTION
Lipomatous uterine tumors are rare benign neoplasms that arise most commonly in women above 55 years of age and can be mistaken for uterine fibroids (leiomyomas) on ultrasound (US) imaging.[1] These fatty masses can be categorized into three different groups: Pure lipoma, lipoma with elements of mesoderm, and liposarcoma.[2] Lipoma or lipoleiomyoma is a rare single variant of the second group of lipomatous tumors, with a reported incidence of 0.03–0.2%.[3] Histologically, these lesions consist of variable amounts of adipocytes with smooth muscle and fibrous tissue.[2,4,5]
The histologic origin of lipoleiomyoma remains unclear; however, some significance has been placed on the presence of these tumors as it may indicate the presence of coexistent malignancy originating from the uterus, cervix, or ovaries.[4] Here, we describe a case of a 63-year-old female in whom a lipoleiomyoma of the uterine corpus was viewed on computed tomography (CT) and pathologically confirmed on a hysterectomy specimen.
CASE REPORT
A postmenopausal 63-year-old female presented with a 3-week history of spotty vaginal bleeding, followed by two separate massive bleeding events in the same day. Physical examination found the patient to be overweight with a soft non-distended abdomen and no masses detected on palpation. Transabdominal US imaging identified an echogenic uterine mass and thickening of the endometrial stripe suggestive of endometrial malignancy [Figure 1]. Color Doppler US revealed hypervascularity of the endometrial mass [Figure 2]. The patient was referred to a gynecologist, where several endometrial biopsies were taken. Histopathology confirmed the presence of uterine endometrial adenocarcinoma.
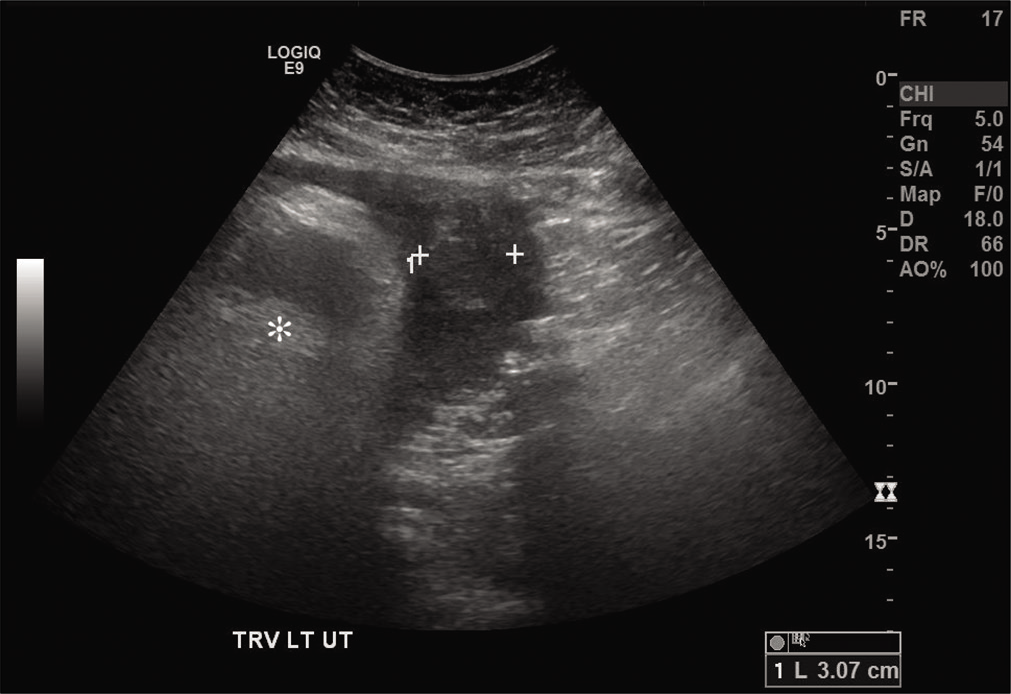
- A 63-year-old postmenopausal woman who presented with a 3-week history of vaginal bleeding. Transabdominal ultrasound imaging of the uterus displays thickening of the endometrial stripe (between calibers) compatible with endometrial malignancy. Furthermore, visible is an echogenic mass (asterisk).
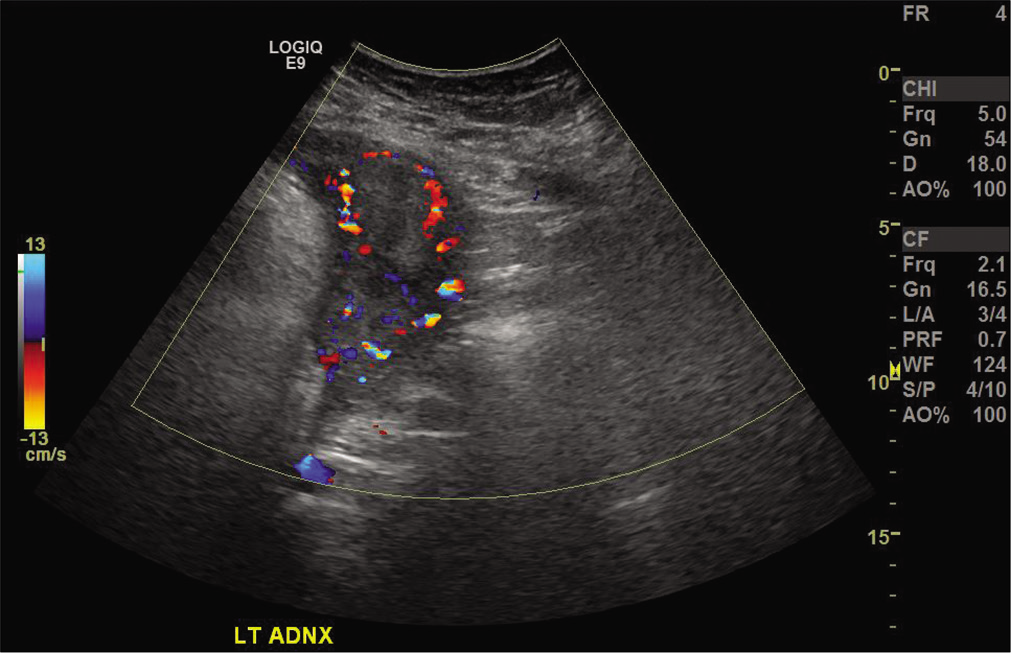
- A 63-year-old postmenopausal woman who presented with a 3-week history of vaginal bleeding. Color Doppler ultrasound image of the uterus displays hypervascularity of the endometrial adenocarcinoma adjacent to the fatty mass.
During the same day on which the endometrial biopsies were taken, the patient underwent enhanced CT scan of her abdomen and pelvis. CT imaging revealed a fatty mass located on the right aspect of uterine corpus, superolateral to the endometrial malignancy [Figures 3-5].

- A 63-year-old postmenopausal woman who presented with a 3-week history of vaginal bleeding. Axial contrast-enhanced computed tomography image of pelvis displays a fatty mass on the right aspect of uterus (asterisk) with thickening of the endometrial stripe on the left aspect of the uterus (arrow).
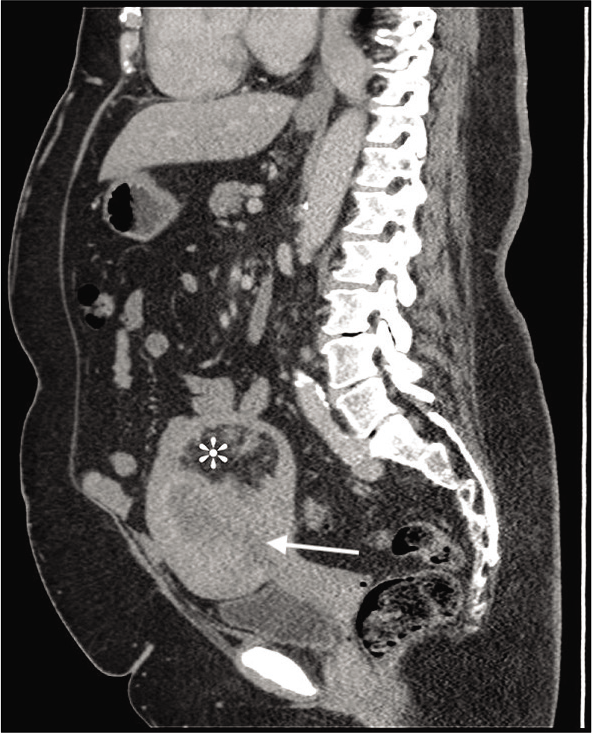
- A 63-year-old postmenopausal woman who presented with a 3-week history of vaginal bleeding. Sagittal contrast-enhanced computed tomography image of abdomen and pelvis displays a fatty mass (asterisk) in the uterus superiorly with endometrial malignancy (arrow) inferiorly.
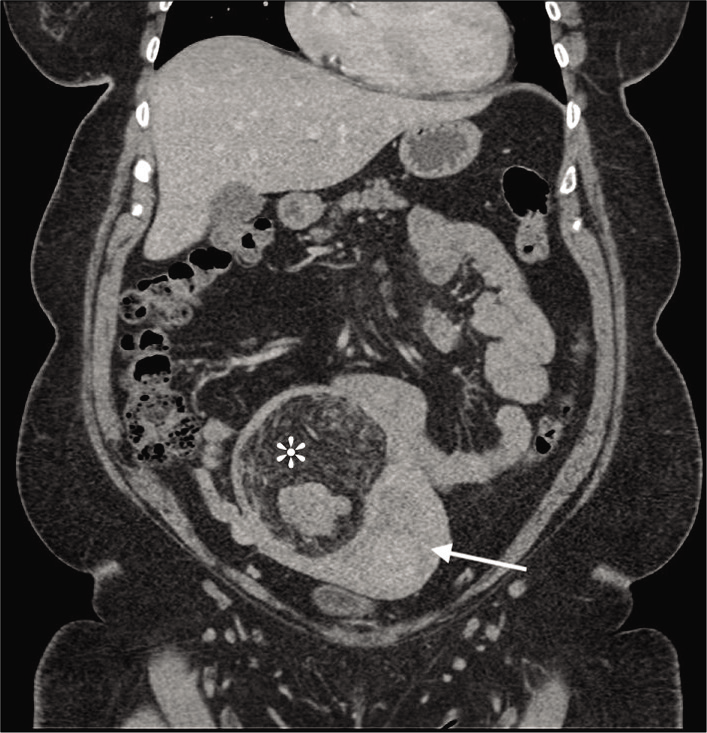
- A 63-year-old postmenopausal woman who presented with a 3-week history of vaginal bleeding. Coronal contrast-enhanced computed tomography image of abdomen and pelvis displays a fatty mass in the right aspect of the uterus (asterisk) and endometrial malignancy left the uterus (arrow).
Three weeks later, the patient underwent a hysterectomy with bilateral salpingo-oophorectomy. Pathology of the extracted uterus, fallopian tubes, and ovaries revealed an 8.1 × 7.5 × 4.8 cm endometrial mass located on the lower anterior and posterior endometrium. This was confirmed to be endometrial adenocarcinoma with 2.2 cm of invasion into a 3.5 cm myometrium on the posterior aspect. No serosal involvement or regional lymph node metastases were noted and the mass was classified as a high Grade 3 endometrial adenocarcinoma.
Pathology also confirmed the presence of a myomatous mass seen in the imaging studies. The mass was located on the posterior uterine wall and measured 11.5 × 10.5 × 9.0 cm. It was 0.3 cm from the endometrial adenocarcinoma without appearance of involvement with it. Microscopic examination of the myomatous mass revealed multiple groupings of mature adipocytes mostly uniform in size and shape separated by bundles of spindle cells [Figure 6a]. Higher magnification revealed the spindle cell bundles to consist mostly of benign mature smooth muscle cells without significant atypia or mitotic activity with small numbers of admixed mast cells and eosinophils [Figure 6b]. Histopathology was consistent with a final diagnosis of lipoleiomyoma.
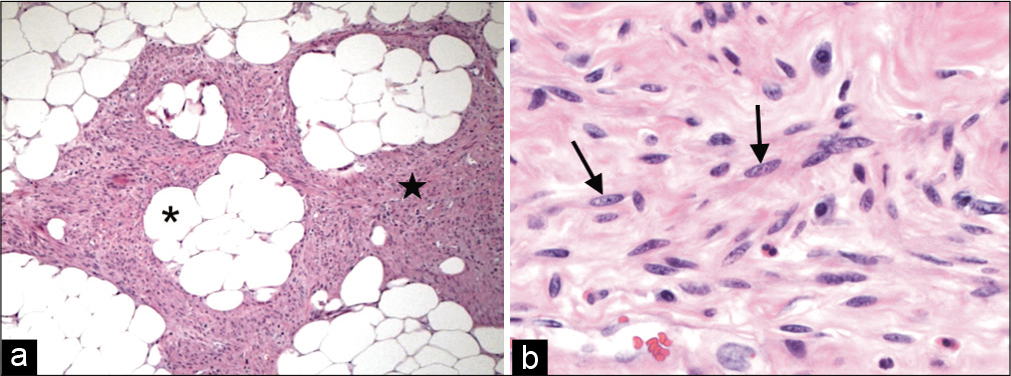
- A 63-year-old postmenopausal woman who presented with a 3-week history of vaginal bleeding. Histopathology of the uterine lipoleiomyoma (hematoxylin-eosin). (a) Lower power (×100) shows admixture of spindle cell (star) and adipose tissue (asterisk). (b) Higher power view (×400) shows benign smooth muscle cells (arrows) without significant atypia or mitotic activity.
DISCUSSION
The patient presented in this report is a 63-year-old postmenopausal female who was diagnosed with a 11.5 cm lipomyoma or lipoleiomyoma of the uterine corpus, found incidentally during the diagnosis of a high Grade 3 endometrial adenocarcinoma. Lipoleiomyomas are benign neoplasms that are a rare fat containing variant of leiomyoma.[6] Fatty uterine masses in general can be categorized into three different groups: Pure lipoma, lipoma with elements of mesoderm, and liposarcoma.[2] Pure uterine lipomas and liposarcoma of the uterus are very rare with only a handful of cases reported to date.[1] Lipoma with elements of mesoderm consists of mixed tumors that can be further subdivided into lipoleiomyomas, angiomyolipomas or fibromyolipomas, based on the amount of adipose tissue, smooth muscle cells, and fibrous tissue present.[2,5] When present, lipoleiomyoma may occur in association with the much more common leiomyoma.
Lipoleiomyoma consists of variable amounts of mature smooth muscle cells, adipocytes, and fibrous tissue but the exact histogenesis of these benign tumors remains unclear.[7] It has been proposed that these tumors may arise from misplaced embryonic adipocytes, metaplasia of muscle tissue, lipolytic differentiation of primitive connective tissue cells, or transformation of mesenchymal totipotent cells.[2,7] One study reports that at least some lipoleiomyomas arise from leiomyomas undergoing lipomatous metaplasia.[8]
Regardless of the origin, lipoleiomyoma has been shown to most commonly arise in women above 55. Most are localized in the corpus of the uterus and are usually intramural.[5] Lipoleiomyoma can be asymptomatic, with the lesion only discovered incidentally or it can present with symptoms similar to those of patients with leiomyomas of similar size.[5,7] These symptoms may include a palpable abdominal mass, lower abdominal pain, increased frequency of urination, and/or urinary incontinence.[2,5] Our patient presented with symptoms of postmenopausal vaginal bleeding. It is difficult to determine whether this was due to the presence of the lipoleiomyoma or the coexisting endometrial malignancy; however, postmenopausal bleeding in patients with isolated lipoleiomyoma has been reported to be quite rare.[9] As observed in the previous studies, lipoleiomyoma can co-occur with other conditions, including gynecological malignancies, as seen in our patient.[7]
US imaging of lipoleiomyoma commonly reveals a well-delineated fatty mass with increased echogenicity surrounded by a hypoechoic strip representing the adjacent myometrium.[2,3] On CT imaging the appearance of predominantly fat density tissue within a uterine mass is diagnostic of a lipoleiomyoma.[5] CT imaging in our patient revealed a well-marginated, mostly radiolucent mass, with tissues of varying radiodensities mixed within it, indicating that the mass is not a pure lipoma. While imaging plays an important role in diagnosing and localizing the pre-operative lipoleiomyoma, post-operative histopathological examination is required to confirm the final diagnosis.[10]
The most common fatty tumor of the female pelvis is the benign mature cystic ovarian teratoma.[2] Differentiating lipoleiomyoma from cystic ovarian teratoma on US can be challenging, mainly if the lipoleiomyoma is located at the posterior wall of the uterus close to the ovary.[5] Correct identification of these tumors is important, however, as their management is very different. Isolated lipomatous tumors such as lipoleiomyoma are mostly benign and when asymptomatic require no surgery and do not affect mortality on their own.[6] Ovarian teratomas, by contrast, must be surgically excised due to the risk of torsion, rupture, or other future complications.[2,6,10] In addition to cystic ovarian teratoma, the differential for lipoleiomyoma should include other lipid containing tumors, including lipoblastic lymphadenopathy, well-differentiated liposarcoma, retroperitoneal cystic hamartoma, and non-teratomatous lipomatous ovarian tumor.[2,5,6,10]
CONCLUSION
This case helps draw attention to uterine lipoleiomyoma, one of the rarest benign neoplasms of the uterus. These fatty tumors present similar to leiomyomas and as such are generally not harmful; however, the potential exits for diagnostic confusion with other uterine tumors. Therefore, increased awareness of lipoleiomyoma, its imaging features, and clinical presentation can help avoid unnecessary surgery in asymptomatic patients.
Acknowledgment
We thank Dr. Michele T. Rooney for help with the histopathology analysis and diagnosis.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Uterine lipoma with a coincidental brenners tumor in the ovary in postmenopausal women: A case report. J Midlife Health. 2015;6:88-90.
- [CrossRef] [PubMed] [Google Scholar]
- Uterine lipoleiomyoma: A report of two cases. J Clin Imaging Sci. 2017;7:26.
- [CrossRef] [PubMed] [Google Scholar]
- Uterine lipoleiomyomas: US and CT findings. Abdom Imaging. 2000;25:655-7.
- [CrossRef] [PubMed] [Google Scholar]
- Uterine lipoleiomyomas: A clinicopathologic study of 50 cases. Int J Gynecol Pathol. 2006;25:239-42.
- [CrossRef] [PubMed] [Google Scholar]
- Lipoleiomyoma of uterus in a postmenopausal woman. J Midlife Health. 2010;1:86-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and pathological features of lipoleiomyoma of the uterine corpus: A review of 76 cases. Balkan Med J. 2014;31:224-9.
- [CrossRef] [PubMed] [Google Scholar]
- Benign metastasizing lipoleiomyoma of the uterus. Int J Gynecol Pathol. 2003;22:202-4.
- [CrossRef] [PubMed] [Google Scholar]
- Lipoleiomyoma of uterus: A case report. J Evol Med Dent Sci. 2015;4:4893-6.
- [CrossRef] [Google Scholar]






