Translate this page into:
Image Quality and Radiation Dose for Fibrofatty Breast using Target/filter Combinations in Two Digital Mammography Systems

-
Received: ,
Accepted: ,
How to cite this article: Alkhalifah K, Asbeutah A, Brindhaban A. Image quality and radiation dose for fibrofatty breast using target/filter combinations in two digital mammography systems. J Clin Imaging Sci 2020;10:56.
Abstract
Objectives:
The aim of this study was to determine the optimum combinations of target and filter materials for various X-ray tube voltage settings, as well as their effects on image quality and radiation dose. This was done using different digital mammography (DM) imaging systems with a breast equivalent phantom.
Material and Methods:
Two DM units with a tungsten (W) target, silver (Ag), and rhodium (Rh) filters and dual molybdenum (Mo) and Rh targets/filters were used. A tissue-equivalent mammography phantom of 6 cm thickness equivalent to a fibrofatty breast was exposed 20 times to different target/filter material combinations (W/Rh, W/Ag, Rh/Rh, Mo/Rh, and Mo/Mo) and various kV settings (28–34 kV). The signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) were calculated for each exposure.
Results:
The W/Ag combination resulted in the lowest entrance skin dose and mean glandular dose (MGD). The MGD for the W/Rh combination was 60% less than that of the W/Ag combination at 34 kV (P < 0.05). There was a direct relationship in the SNR with the Mo/Mo, Mo/Rh, and Rh/Rh combinations and an inverse relationship with the CNR in the 34 kV range. There were statistically significant differences between all five target/filter combinations, and the best SNR and CNR were observed for the W/Rh combination with a reduced radiation dose in the range of 28–30 kV (P < 0.05).
Conclusion:
For a breast thicknesses of 6 cm with a fibrofatty nature, the W/Rh combination delivers high performance in terms of image quality at a lower dose.
Keywords
Digital mammography
Mammography phantom
Exposure factors
Target/filter combination
Contrast-to-noise ratio
Signal-to-noise ratio
INTRODUCTION
Mammography is the gold standard for breast cancer imaging. Tremendous technological advancements have occurred in the past two decades with the introduction of digital image receptors and non-traditional target/filter combinations in X-ray tubes. Digital mammography (DM) offers a number of advantages compared to screen-film mammography, and advances in digital detectors have paved the way for exciting new technologies. They have shown great promise in increasing the detection of invasive breast cancer, improving the diagnostic accuracy in dense breasts, and reducing recall rates.[1]
The advancements have necessitated a review of the exposure parameters, which have been long established, while considering the optimization of image quality and the radiation dose to the patient. Optimization of the exposure parameters in DM requires maximization of the image quality, including the contrast-to-noise ratio (CNR), high contrast which enables low-contrast lesions to be differentiated and visualized, and signal-to-noise ratio (SNR), a higher noise level may prevent abnormal soft-tissue masses or microcalcifications from being detected or visualized of the breast, while minimizing the patient dose. Older women undergo more breast screening due to the increasing incidence of breast cancer.[2] Since the breast is a radiosensitive organ, it is important for the radiation dose level during mammography to be kept as low as possible in both screening and diagnosis.[3,4]
The entrance skin dose (ESD) can be used to estimate the risk provided that the X-ray beam quality is sufficiently known. The quality of the beam depends on the target/ filter combination and the peak voltage. Focusing on 6 cm breast thickness and more, there has been an increase in the number of such women with fatty large breast in Kuwait. This could allow for the use of ESD values as an indicator of risk in select populations.
A major factor that determines both the image quality and patient dose is the spectral composition of the X-ray beam. The energy spectrum is determined primarily by the X-ray tube’s target material, the type of filtration, and the tube’s operating voltage.[5-7] The X-ray beam quality is determined by the X-ray tube voltage and the materials of the target and filter. The quality determines the intrinsic/ subject contrast generated in the tissues. The subject contrast decreases with increasing beam energies irrespective of the dose.[8] In conventional mammography, molybdenum (Mo) and rhodium (Rh) have usually been used as target and filter materials. However, with digital detectors and their energy responses, other choices have been introduced, such as tungsten (W), aluminum (Al), and silver (Ag).[9-12]
The composition of breast tissue can vary in different women according to age, breast glandularity, and adipose tissue. A large variety of breast phantoms have been produced by different vendors with tissue-equivalent materials and used to study attenuation, density of tissue, and image visibility.[13] The previous studies have shown that a fully digital mammography (FDM) system has optimum image quality and is capable of detecting subtle calcification clusters with low dose.[14,15]
Aminah et al.[7] reported a potential for dose reduction of up to 11% for a set CNR of 3.0 when using different beam quality from that determined by selecting automatic exposure control (AEC). This study also found that exposure factors for optimal image quality depend on the composition of breast tissue (glandular vs. adipose tissue). However, the dependence of exposure factors on different thicknesses of breast tissue has not been studied widely.
The Mo/Mo combination was superior for a compressed breast thickness of 2 cm. Alternative anode/filter combinations, such as W/Rh, have been recommended for compressed breast thicknesses of 4–6 cm over Mo/Rh, Rh/Rh, and Rh/Al. The W/Rh combination has been established to deliver a lower dose for the same CNR.[12] and is the preferred target for the detection of infiltrating ductal carcinoma and calcifications.[16,17] As breast thickness increased, a W target with a Tin (Sn) filter resulted in 34% improvement in CNR for the same dose to the breast.[18]
A study has reported benefits of using Mo filters for a breast thickness of 3 cm, Ag filters for 4.5 cm, Sn filters for 6 cm, and Al filters for 7.5 cm.[19] There are reports of using the W/Rh combination for compressed breast thicknesses ranging from 4 to 6 cm and different breast glandularities, which delivered high performance in terms of image quality at a lower radiation dose.[20,21] The main aim of this study was to determine the effects on the image quality and radiation dose of different combinations of target/filter materials with various settings of the X-ray tube voltage. Two DM imaging systems were used on a 6 cm thickness equivalent breast phantom containing materials equivalent to 20% glandular tissue and 80% adipose tissue.
MATERIAL AND METHODS
DM imaging systems
The two full FDM systems were used throughout this study: A Hologic-Selenia system (Hologic, Inc., Marlborough, USA) and a GE Senographe Essential system (Ge Medical manufactured by GE Healthcare, Milwaukee, WI). The Hologic-Selenia system consists of an X-ray tube with a W target and Ag and Rh as filter materials (30 mm and 25 mm thick, respectively). It also has 70 μm amorphous selenium detectors. The GE Senographe Essential system consists of an X-ray tube with Mo and Rh as target materials and Mo and Rh as filter materials (30 mm and 25 mm thick, respectively). This results in three possible target/filter combinations: Mo/Mo, Mo/Rh, and Rh/Rh. It also has a flat-panel cesium iodide (CsI) detector with 100 μm pixels. AEC was used for both systems to maintain a constant pixel value (PV), and the systems were set up in standard dose mode.
Mammography phantoms
The Computerized Imaging Reference Systems (CIRS, Inc., Norfolk, VA) Model 010 C tissue-equivalent mammography phantom was used to compare the radiation dose and image quality. The phantom is shaped as a compressed breast of 6 cm thickness. It is made of epoxy resin equivalent to 20% glandular and 80% adipose tissues in terms of their X-ray attenuation properties. The phantom contains 12 calcium carbonate specks with grain sizes of 0.13, 0.165, 0.196, 0.23, 0.275, 0.4, 0.23, 0.196, 0.166, 0.23, 0.196, and 0.165 mm. It also has five nylon fibers with diameters of 1.25, 0.83, 0.71, 0.53, and 0.3 mm, as well as hemispheric masses of 55% glandular and 45% adipose tissue with diameters of 4.76, 3.16, 2.38, 1.98, 1.59, 1.19, and 0.90 mm.
The phantom has a step wedge for contrast measurements consisting of five 1 cm thick inserts corresponding to glandular compositions of 0%, 30%, 50%, 70%, and 100%. Near the step wedge, there is a reference zone in a uniform region of the phantom for the measurement of the PV. A diagram of a similar phantom with different thickness and tissue composition is shown in Figure 1.

- Schematic diagram of a CIRS phantom. The step wedge for the contrast-to-noise ratio measure is represented by details 14–18: detail 14, 100% glandular; detail 15, 70% glandular; detail 16, 50% glandular; detail 17, 30% glandular; detail 18, 100% adipose. The region of interest (ROI) 31 is the reference ROI.
Image acquisition
Images of the phantoms were acquired using AEC at a source image receptor distance of 65 cm for all exposures on both mammography systems. The X-ray tube voltages were from 28 to 34 kV at intervals of 2 kV. Filter materials were selected manually. The phantom was exposed 20 times in total (4 times for each target/filter combination: W/Rh, W/Ag, Rh/Rh, Mo/Rh, and Mo/Mo). Special attention was given to place the phantom in the same position on the detector, and the uniformity of the detector was measured according to the European guidelines.[22] The ESD and mean glandular dose (MGD) were recorded for each exposure.
Image analysis
Three regions of interest (ROIs) were selected from each image for SNR measurements. SNR was calculated by determining the mean PV and its standard deviation (SD) in each ROI. The CNR was measured between the step wedges of 70% glandularity in the phantom against the three ROIs selected for SNR measurements. For each detail, the CNR was calculated according to the definition in the European guidelines for quality assurance in mammography screening:[20]
Where, MCD is the mean PV of the contrast disc, MBG is the mean PV of the background, and σBG is the SD of the background.
Statistical analysis
All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 25 for Windows (SPSS Inc., Chicago, IL, USA). Non-parametric Kruskal–Wallis test and Mann–Whitney U-test were used to test for statistical significance of the differences in the SNR and CNR values for different combinations of target/filter materials and various kV settings. The lowest radiation dose and optimum SNR and CNR in all 20 phantom exposures were compared. Statistical significance was established at the level of P = 0.05 for all statistical tests.
RESULTS
The ESD and MGD values in mGy were obtained directly from the digital mammographic units after each exposure. As shown in Tables 1 and 2, the target/filter combination of W/Ag resulted in lower ESD and MGD values than the W/Rh combination. The Mo target with different filter materials yielded higher ESD and MGD values, and the highest values were observed for the Mo/Mo target/filter combination. The MGD for the W/Ag combination was 60% less than that of the W/Rh combination at 28 kV, 55% less at 30 kV, 55% less at 32 kV, and 62% less at 34 kV. In the comparisons between the W, Rh, and Mo targets, there was a significant difference in the MGD from that of W/Ag at 34 kV (P < 0.05).
| Target/Filter – kV | W/Rh | W/Ag | ||||
|---|---|---|---|---|---|---|
| mAs | ESD (mGy) | MGD (mGy) | mAs | ESD (mGy) | MGD (mGy) | |
| 28 | 118 | 5.01 | 1.2 | 69.6 | 3.5 | 0.72 |
| 30 | 89.8 | 4.6 | 1.2 | 52.7 | 3.2 | 0.65 |
| 32 | 67.7 | 4.02 | 1.1 | 40.8 | 2.9 | 0.61 |
| 34 | 49.3 | 3.3 | 0.94 | 32.2 | 2.6 | 0.56 |
ESD: Entrance skin dose, MGD: Mean glandular dose, W: Tungsten target, Rh: Rhodium, Ag: Silver
| Filter kV | Rh/Rh | Mo/Rh | Mo/Mo | ||||||
|---|---|---|---|---|---|---|---|---|---|
| mAs | ESD (mGy) | MGD (mGy) | mAs | ESD (mGy) | MGD (mGy) | mAs | ESD (mGy) | MGD (mGy) | |
| 28 | 90 | 14.9 | 4 | 100 | 15.7 | 4.7 | 110 | 18.3 | 5.1 |
| 30 | 80 | 11.9 | 2.9 | 90 | 12.5 | 3.4 | 100 | 13.7 | 3.6 |
| 32 | 71 | 9.1 | 2 | 80 | 9.5 | 2.4 | 90 | 10 | 2.9 |
| 34 | 63 | 5.6 | 1.4 | 71 | 6.5 | 1.6 | 80 | 7.1 | 1.8 |
ESD: Entrance skin dose, MGD: Mean glandular dose, Mo: Molybdenum, Rh: Rhodium, Ag: Silver
Figures 2 and 3 show the SNR and CNR values for the target/ filter material combinations of W/Rh and W/Ag. The non- parametric Kruskal–Wallis test and Mann–Whitney U-test showed statistically significant differences between these combinations (P = 0.02). The SNR values decreased with increasing voltage, but the highest SNR was obtained at 28 kV. Figure 3 shows the average CNR results. The non-parametric Kruskal–Wallis test and Mann–Whitney U-test showed statistically significant differences between the combinations (P = 0.015). There was an increase in the CNR as the voltage increased in the range tested, which was more obvious with W/Rh than with W/Ag.
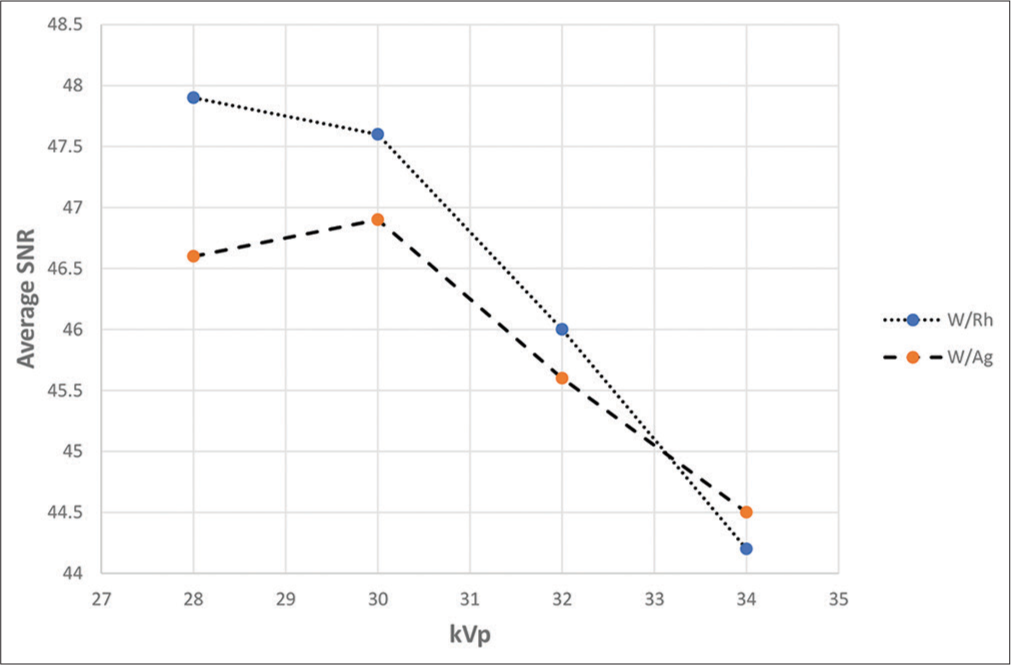
- A graph showing the relationship between average signal- to-noise ratio (SNR) for target/filter combination for tungsten/ rhodium (W/Rh) and tungsten/silver (W/Ag) at various kV settings.
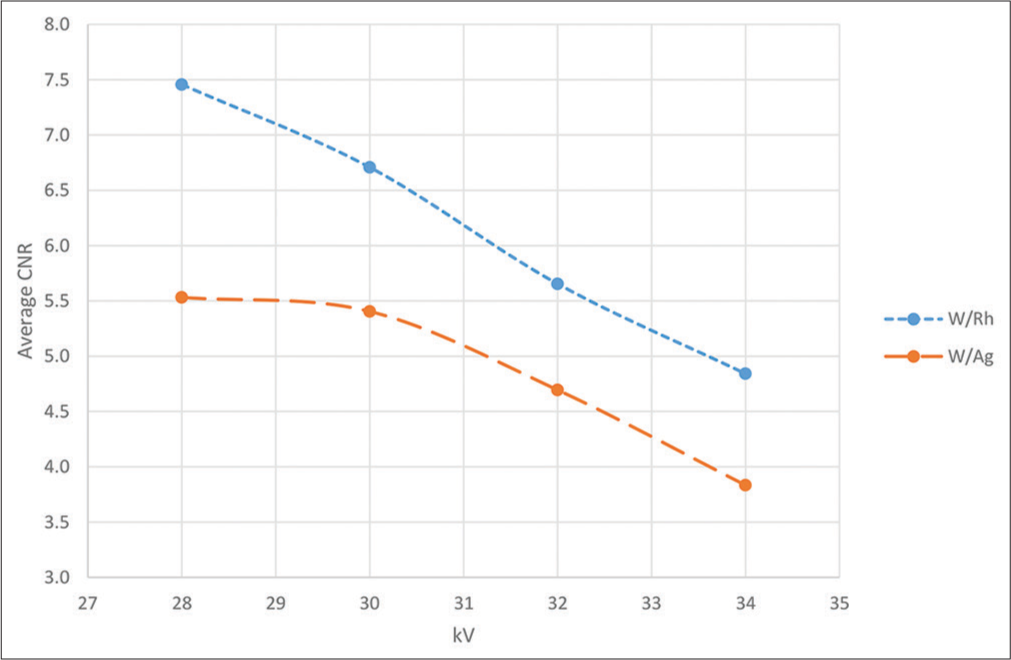
- A graph showing the relationship between average contrast-to-noise ratio (CNR) for target/filter combination for tungsten/rhodium (W/Rh) and tungsten/silver (W/Ag) at various kV settings.
Figures 4 and 5 show the SNR and CNR for the target/filter material combinations of Rh/Rh, Mo/Rh, and Mo/Mo. The non-parametric Kruskal–Wallis test and Mann–Whitney U-test showed statistically significant differences between the different combinations (P = 0.025). In general, the SNR increases as the voltage increases, especially for the Mo/Mo combination, while the CNR decreases.
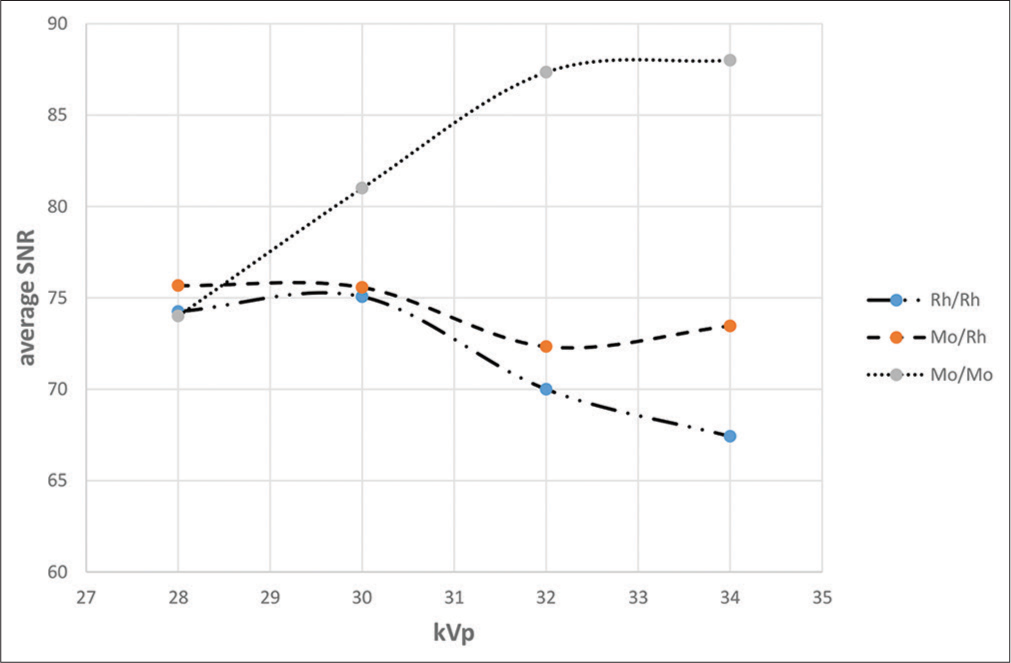
- A graph showing the relationship between average signal- to-noise ratio (SNR) for target/filter combination for molybdenum (Mo) and rhodium (Rh) and various filter combination materials at various kV settings.
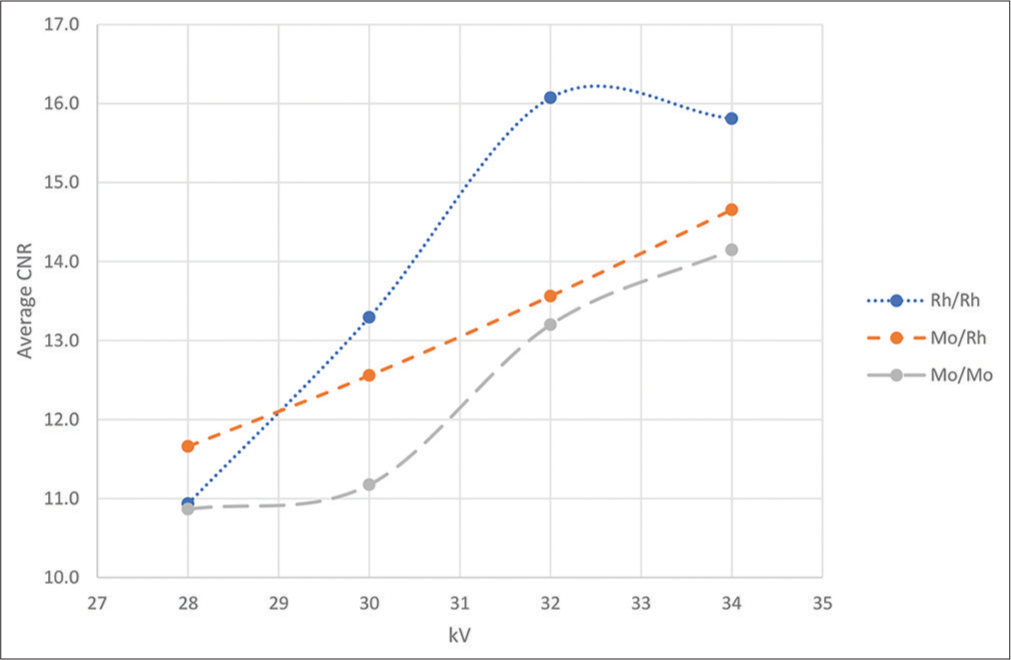
- A graph showing the relationship between average contrast-to-noise ratio (CNR) for target/filter combination for molybdenum (Mo) and rhodium (Rh) and various filter combination materials at various kV settings.
DISCUSSION
Figures 6 and 7 show the different spectrum between Mo and W targets. Mo target gives excellent range of energy with film screen but the disadvantage creates high breast dose, while W target works excellent with DM cos of the high-energy k-edge absorption of the detector. The major advantage it reduces breast dose due to beam harder. The results in Figures 2 through 5 show that W/Rh always has the highest SNR and CNR, whereas Mo/Mo has lower CNR and higher SNR. The standard value for SNR should be 40 and above. For the Mo/Mo combination, the optimum tube potential is 2–4 kV lower than that of the other combinations for the 6 cm breast thickness. This means that the W/Rh combination is always a better choice than W/Ag, whereas the Mo/Mo combination is always the least suitable choice for optimal acquisition. The Mo/Rh curve is similar to the W/Ag curve for 6 cm breast thickness.

- Show the different spectrum for Mo target. (a) Mo spectrum for different kVp’s without filter. (b) Mo spectrum for different kVp’s with Mo filter.

- W spectrum for different kVp’s.
The previous studies have shown that the W/Rh combination is always the optimum choice to deliver high performance in terms of image quality at a lower dose,[20,21] but they did not specify the breast thickness. The CNR for a 34 kV Rh filter was significantly better than that for other kV values (P = 0.027). In contrast, there were no significant changes in SNR for various kV values with Rh filters (P = 0.35). The CNR for silver filters showed significant differences in the 34 kV range (P = 0.02), while there was no change in the SNR for various kV values with the Ag filter (P = 0.57).
In comparisons between Rh and Ag filters at 28, 30, 32, and 34 kV, the CNR was better for the Rh filters (P = 0.05), but there were no significant differences in the SNR (P > 0.05). In the 34 kV range, the Rh filter was the best, resulting in excellent CNR and SNR. The SNR was almost the same and did not differ with different kV or filter materials. For the Mo/Mo target/filter material combination, 32 kVp and 34 kVp were the best in terms of SNR (P < 0.05). In the 28 kV range, Mo/Rh was the best with respect to CNR but not for SNR. The comparison of three target/filter material combinations in terms of kV showed changes in CNR in the range of 30–34 kV for Rh/Rh.
Using the data in Tables 1 and 2, it is possible to compare the performance of each target/filter combination at the optimum tube potential value (PV). A dose reduction was obtained for images with the same PV in the reference zone, particularly when using the W/Ag combination with tube potentials of 28–34 kV at 6 cm. The MGD for the Ag filter was 60% less than that for the Rh filter at 28 kV, while at 30 kV, it was 55% less than that for the Rh filter at 32 kV and 62% less at 34 kV. When comparing between the three targets with Mo and W, W/Rh yielded better MGD for 34 kVp with 60% less dose reduction than Mo/Mo in the 28 kV range. We attributed this to the fact that the W/Ag combination produces more penetrating X-ray beams that present a higher half value layer value and lower MGD.
Our results are in good agreement with those of other studies. Bernhardt et al.[23] examined parameter optimization for the detection of microcalcifications and tumors with different breast thicknesses and compositions using three different anode/filter combinations. They reported that for a DM system based on an a-Se detector, the W/Rh combination is the best choice for all detection tasks. They used a 4 cm breast thickness and 50% glandular composition. For tumor detection, they found that the optimal tube voltages for the Mo/Mo, Mo/Rh, and W/Rh combinations are 26.5 kV, 28.5 kV, and 28 kV, respectively, for a 4 cm breast thickness and 50% glandular composition. They also found that the W/Rh combination was the best for a 6 cm breast thickness with 20% glandular tissue and 80% fatty tissue at a voltage of 34 kV.
The optimum tube voltages estimated in our work are also in good agreement with those estimated by Toroi et al.[24] They indicated the lowest and highest acceptable tube voltages for every thickness. They also concluded that the W/Rh combination provided a lower dose with the same image quality. However, in our study, the W/Rh combination yielded the best image quality in terms of SNR and CNR with the lowest radiation dose in comparison to the W/Ag combination alone. Flynn et al.[18] did a simulation study and concluded that the use of a W tube rather than a traditional Mo tube should lead to significant reductions in exposure time and tube heat while maintaining similar image quality and dose. As in our study, they found that the CNR/square root (average glandular dose) for the W/Ag combination is maximized in the range of about 28–30 kV.
The main limitation of this study is that we applied the techniques to a tissue-equivalent phantom that resembles a human fibrofatty breast and it is limited study to 6 cm thickness equivalent. Further studies are needed with real human cases, different breast thicknesses, and different compositions to verify our findings. In addition, more target/material combinations need to be tested with other exposure factors and parameters that are available on many DM units to achieve the best image quality with the lowest radiation dose. Modern mammography units do not allow a choice of filters in everyday practice.
CONCLUSION
Our results demonstrated that the W/Rh combination is the optimum choice for compressed breast thicknesses of 6 cm with 20% glandular tissue and 80% adipose tissue. This combination delivered high performance in terms of image quality at a lower radiation dose. It is highly recommended to use this combination for this purpose, but if not possible, it is best to use Rh/Rh or Mo/Rh. The machine automatically chooses the filter depending on breast thickness and density. The Hologic DM is W/Rh and automatically switches to W/Ag for thick/dense breast to get the optimal image with no choice. Film screen is Rh/Rh or Mo/Rh and can be done manually. However, there is a trade off if the image is not optimized although the dose is less.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A comparison of digital mammography detectors and emerging technology. Radiography. 2015;21:315-23.
- [CrossRef] [Google Scholar]
- The impact of age on the art of mammography and how to adapt accordingly. Radiography. 2017;23:e120-1.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of dose reduction on the detection of mammographic lesions: A mathematical observer model analysis. Med Phys. 2007;8:3385-97.
- [CrossRef] [PubMed] [Google Scholar]
- The Essential Physics of Medical Imaging Philadelphia, PA: Lippincott Williams and Wilkins; 2002.
- [Google Scholar]
- Optimal beam quality selection in digital mammography. Br J Radiol. 2006;79:981-90.
- [CrossRef] [PubMed] [Google Scholar]
- Optimization of exposure parameters in full field digital mammography. Med Phys. 2008;35:2414-23.
- [CrossRef] [PubMed] [Google Scholar]
- Optimal beam quality selection based on contrast-to-noise ratio and mean glandular dose in digital mammography. Australas Phys Eng Sci Med. 2010;33:329-34.
- [CrossRef] [PubMed] [Google Scholar]
- Physical characterization of a prototype selenium-based full field digital mammography detector. Med Phys. 2005;32:588-99.
- [CrossRef] [PubMed] [Google Scholar]
- Contrast and dose with Mo-Mo, Mo-Rh, and Rh-Rh target-filter combinations in mammography. Radiology. 1995;195:639-44.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of anode and filter material on image quality and glandular dose for screen-film mammography. Phys Med Biol. 1991;36:1165-82.
- [CrossRef] [PubMed] [Google Scholar]
- Optimal X-ray spectra for screen-film mammography. Med Phys. 1981;8:629-39.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of anode/filter material and tube potential on contrast, signal-to-noise ratio and average absorbed dose in mammography: A Monte Carlo study. Br J Radiol. 2000;73:1056-67.
- [CrossRef] [PubMed] [Google Scholar]
- Study of Attenuation Coefficient of a Breast Phantom used in Diagnostic Radiology.
- Evaluation of doses and image quality in mammography with screen-film, CR, and DR detectors-application of the ACR phantom. Pol J Radiol. 2016;18:386-91.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of image quality on calcification detection in digital mammography. Med Phys. 2012;39:3202-13.
- [CrossRef] [PubMed] [Google Scholar]
- Optimization of spectral shape in digital mammography: Dependence on anode material, breast thickness, and lesion type. Med Phys. 1994;21:1473-81.
- [CrossRef] [PubMed] [Google Scholar]
- A model for optimization of spectral shape in digital mammography. Med Phys. 1994;21:1463-71.
- [CrossRef] [Google Scholar]
- Optimal radiographic techniques for digital mammograms obtained with an amorphous selenium detector. Proc SPIE. 2003;5030:147-56.
- [CrossRef] [Google Scholar]
- Optimization of tungsten X-ray spectra for digital mammography: A comparison of model to experiment. Proc SPIE. 1997;3032:411-8.
- [CrossRef] [Google Scholar]
- Investigation of the effect of anode/filter materials on the dose and image quality of a digital mammography system based on an amorphous selenium flat panel detector. Br J Radiol. 2010;83:290-5.
- [CrossRef] [PubMed] [Google Scholar]
- Investigation of exposure factors for various breast composition and thicknesses in digital screening mammography related to breast dose. Med Princ Pract. 2018;27:211-6.
- [CrossRef] [PubMed] [Google Scholar]
- European Guidelines for Quality Assurance in Breast Cancer Screening and Diagnosis (4th ed). Luxembourg: Office for Official Publications of the European Communities; 2006.
- [Google Scholar]
- X-ray spectrum optimization of full-field digital mammography: Simulation and phantom study. Med Phys. 2006;33:4337-49.
- [CrossRef] [PubMed] [Google Scholar]
- Experimental investigation on the choice of the tungsten/rhodium anode/filter combination for an amorphous selenium-based digital mammography system. Eur Radiol. 2007;17:2368-75.
- [CrossRef] [PubMed] [Google Scholar]






