Translate this page into:
Clinical Significance of T2*gradient-recalled Echo/susceptibility-weighted Imaging Sequences in Evaluating Superficial Siderosis in the Setting of Intracerebral Tumors: Pilocytic Astrocytoma
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Superficial siderosis is the slow accumulation of hemosiderin on the pial surfaces of the brain and spinal cord. The most common cause of intracranial superficial siderosis is secondary to subarachnoid hemorrhage. Rarely, superficial siderosis can also be caused by tumors. Superficial siderosis presents clinically as hearing loss and gait instability that progressively worsen. The diagnosis is primarily made by magnetic resonance imaging; however, susceptibility-weighted imaging (SWI) and T2* gradient echo (GRE) sequences demonstrate the highest sensitivity in detecting this condition. To the best of our knowledge, there has been only one previous case of superficial siderosis secondary to a pilocytic astrocytoma of the spine. However, we present a case of intracerebral pilocytic astrocytoma resulting in superficial siderosis, with emphasis on acquisition and use of T2*GRE/SWI sequences.
Keywords
Hearing loss
intraventricular tumor
pilocytic astrocytoma
siderosis

INTRODUCTION
Superficial siderosis is a rare condition that involves the buildup of hemosiderin from recurrent or prolonged bleeding on the pial surfaces of the brain or spinal cord. It was first described in 1908 by Hamill,[1] but for decades to follow, it was a diagnosis that was primarily made postmortem on autopsy.[2] Superficial siderosis is characterized by the classic triad of sensorineural deafness (95%), cerebellar ataxia (88%), and pyramidal signs (76%). Other symptoms that present less frequently include dementia (24%), bladder disturbance (24%), anosmia (17%), anisocoria (10%), and sensory signs (13%).[3] There are many underlying causes of superficial siderosis which include, but are not limited to, idiopathy, trauma, arteriovenous malformations, subarachnoid hemorrhage, amyloid angiopathy, brachial plexus/root injury, and tumors. Pilocytic astrocytoma is a low-grade tumor that is most prevalent in the first two decades of life with an incidence rate of 4.8/1 million/year.[4] Here, we discuss the case of an intraventricular pilocytic astrocytoma possibly causing microhemorrhage leading to superficial siderosis that resulted in sensorineural hearing loss and gait instability, which, to our knowledge, has not been reported so far in the literature.
CASE REPORT
A 44-year-old male presented to the outpatient clinic with complaints of severe headaches, bilateral hearing loss, and gait instability. On physical examination, Rinne and Weber tests were suggestive of sensorineural hearing loss. The patient's posture was normal with a tandem gait. Cranial nerves were intact. The rest of the physical examination was unremarkable. Routine hematologic and biochemical blood tests to exclude infectious and endocrine or metabolic disorders were within normal limits. Audiometry revealed a bilateral sensorineural type of hearing loss that was more severe on the left, than on the right. A magnetic resonance imaging (MRI) of the brain with intravenous contrast demonstrated an enhancing intraventricular mass in the anterior horn of the right lateral ventricle [Figure 1]. This initial MRI did not contain T2*gradient-recalled echo (GRE) sequences. Neurosurgery was consulted and an uneventful tumor excision was performed. Pathology of the mass confirmed it to be a pilocytic astrocytoma. However, postoperatively, the patient's hearing loss did not resolve. An MRI of the brain was repeated with T2*GRE sequences. These sequences showed susceptibility along the medial aspect of the temporal lobes bilaterally with involvement of the hippocampi. In addition, T2*GRE sequence at the level of the cerebellum also demonstrated susceptibility along the vestibulocochlear nerve and facial nerve bilaterally, extending to the level of the internal acoustic meatus [Figure 2]. The patient was lost to follow-up. Since an intraventricular tumor cannot cause hearing loss, as there is no direct anatomic correlation, the most likely explanation would be that the tumor resulted in microhemorrhage at the level of the internal acoustic meatus that was not visualized on the initial MRI brain as there were no susceptibility-weighted imaging (SWI) or GRE sequences. The timing of the siderosis was likely prior to surgery, as patient's initial complaint of hearing loss was not likely related to the tumor. Furthermore, there could be a possibility that the intraventricular tumor and microhemorrhages were separate entities; however, it is less likely that the etiology of subarachnoid hemorrhage was a separate entity as the progression of the subarachnoid hemorrhage would have eventually resulted in resolution and the patient's symptoms would have improved, rather than persisted. Thus, given the literature search of a pilocytic astrocytoma of the spine resulting in siderosis, this was the most likely explanation. Nonetheless, the patient's initial complaint of hearing loss was not optimally evaluated, and the clinical aspect was more focused on detection of the tumor and the headaches rather than the hearing complaint. Therefore, again, emphasis should always be on a good physical examination and clinical history, which should have led the clinicians to understand that the intraventricular tumor was not the cause of the hearing loss, but rather a different underlying entity such as siderosis was the most likely explanation of these symptoms.
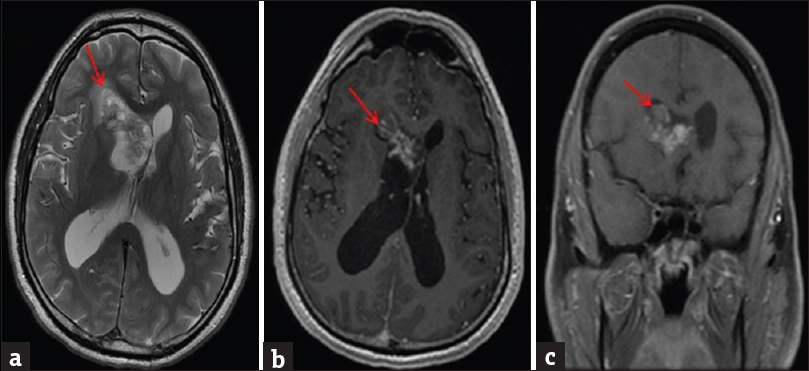
- A 44-year-old male presented with complaints of hearing loss and gait instability. He was found to have a biopsy-proven pilocytic astrocytoma. Magnetic resonance imaging of the brain showed a mass in the right lateral ventricle. (a) Axial T2 sequence demonstrates heterogeneous mass (red arrow in A) within the anterior horn of the right lateral ventricle with associated mass effect and left-sided midline shift. (b) Axial T1 postcontrast images were obtained that demonstrated the intraventricular mass (red arrow in B) to have heterogeneous enhancement. (c) Coronal T1 postcontrast sequence demonstrates heterogeneous enhancement of the right intraventricular mass (red arrow in C) resulting in compression of the left lateral ventricle with mass effect.
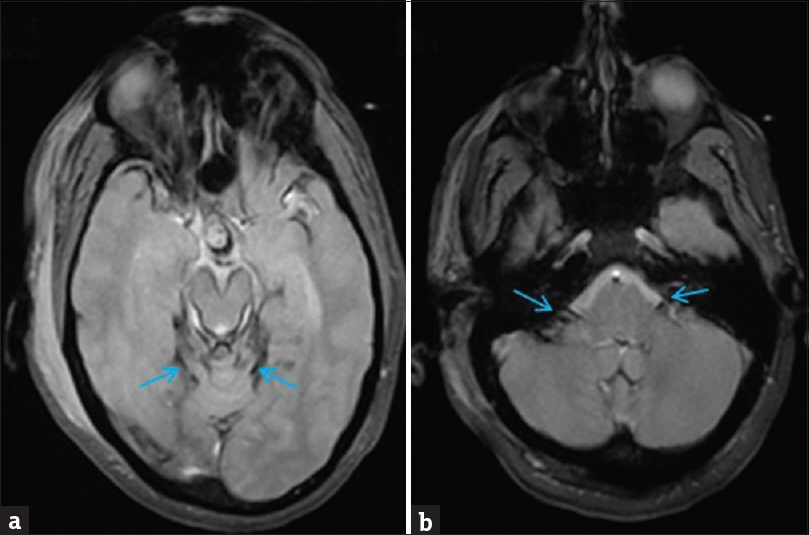
- Forty-four-year-old male status postresection of pilocytic astrocytoma with persistent hearing loss and gait instability. Superficial siderosis was shown on imaging. magnetic resonance imaging brain: Axial T2*gradient-recalled echo sequences of the brain at the level of midbrain (a) and at the level of the pons (b) show superficial siderosis. (a) Axial T2*gradient-recalled echo sequence at the level of the midbrain demonstrates susceptibility along the medial aspect of the temporal lobes bilaterally, specifically involving the hippocampus (blue arrow). (b) Axial T2*gradient-recalled echo sequence at the level of the cerebellum shows susceptibility along the vestibulocochlear nerve and facial nerve bilaterally, extending to the level of the internal acoustic meatus (blue arrow).
DISCUSSION
Superficial siderosis is the deposition of hemosiderin that has the propensity to affect the superior vermis, quadrigeminal plate, and basal cerebral surface. It spares the peripheral nerves, but commonly affects cranial nerves II, V, VII, and VIII.[5] The classic triad in patients with superficial siderosis is sensorineural hearing loss, cerebellar ataxia, and pyramidal signs.[5] Patients with superficial siderosis will often have a prior history of trauma or surgery. Superficial siderosis affects more males than females at a ratio of 3:1 and primarily affects older adults though there have been reported cases involving individuals as young as 14.[67891011] The above-presented case demonstrates a patient presenting with intermittent ataxia and bilateral sensorineural hearing loss. An MRI of the brain with contrast was obtained that showed a heterogeneously enhancing lesion in the anterior horn of the right lateral ventricle with associated mass effect and compression on the left lateral ventricle. The initially obtained MRI did not have T2*GRE sequences since superficial siderosis was not considered as part of the diagnostic workup. Biopsy of the mass confirmed pilocytic astrocytoma. Pilocytic astrocytoma is a WHO Grade I, low-grade tumor of glial cells that primarily affects children under the age of 15. The incidence of pilocytic astrocytoma is 4.8 cases/1 million/year. It accounts for approximately 2% of all central nervous system (CNS) tumors when considering all age groups. Only 17% of patients with pilocytic astrocytoma are over the age of 30. It most frequently develops in the cerebellum in children, but can be supratentorial or cerebellar in adults. Pilocytic astrocytoma has a great prognosis with a 10-year survival rate of 95.8%.[4]
The pathophysiology of superficial siderosis depends on the underlying cause though all etiologies will have some form of a chronic bleed to allow for the buildup of hemosiderin, such as subarachnoid hemorrhage.[8] Intraventricular tumors can result in microhemorrhage leading to the deposition of hemosiderin onto the subependyma.[12] A study done by Levy et al., viewed a total of 270 cases with superficial siderosis. Among these, 21% of patients were found to have superficial siderosis secondary to CNS tumors.[13] There is variation with regard to the bleeding mechanism of a tumor causing siderosis. Tumors may undergo spontaneous intratumoral hemorrhage which can, over time, lead to superficial siderosis. The exact mechanism of the intratumoral hemorrhage is unknown, but it is hypothesized that the blood vessel walls within the tumor and connective tissue stroma degenerate and eventually rupture.[14] Surgical removal of an intracerebral/intraventricular mass can result in siderosis secondary to bleeding as a result of postsurgical changes.[5] In 50% of documented cases of siderosis, the exact cause or etiology is unknown.[12]
Suspicion for superficial siderosis is usually prompted by imaging. Contrast-enhanced images will not show enhancement. On noncontrast-enhanced computed tomography (NECT), superficial siderosis will appear as a hyperdense rim, most prominent along the brainstem and surrounding the vestibulocochlear nerve. There may also be cerebral and cerebellar atrophy; however, NECT has low sensitivity in detecting superficial siderosis and an MRI should be considered. On T1-weighted images, regions with siderosis will be hyperintense. On T2-weighted images, the vestibulocochlear nerve will appear thicker and there will be a hypodense rim along the contours of the brain accompanied by cerebellar atrophy. The hypodense rim is often missed because it follows the contours of the brain and spinal cord. As such, it might be beneficial to look at the adjacent tissue which will be hyperintense relative to the affected tissue.[15] On T2 fluid-attenuated inversion recovery (FLAIR), hemosiderin deposition will appear as a dark border lining the cranial nerves and CNS. T2*GRE or GRE with SWI has better sensitivity in detecting superficial siderosis. On T2*GRE sequences, the hemosiderin deposition will appear thicker than on T2-weighted images. There will also be a blooming dark signal along the pial- and sub-pial brain [Figure 2].[67891011] Other imaging modalities can be pursued based on the underlying etiology of the suspected superficial siderosis. CT myelography can detect dural diverticula, pseudomeningoceles, or transdural leaks that may be the cause of siderosis. Cerebral angiography has low utility except with slow-flow pial arteriovenous malformations.[16]
SWI is an MRI sequence sensitive to compounds that cause distortion in the local magnetic field and is useful for detecting blood products, calcium, etc. SWI is a three-dimensional high-spatial resolution velocity gradient echo MRI sequence. Compounds that have paramagnetic, diamagnetic, or ferromagnetic properties can distort the magnetic field and alter the phase of local tissue that results in the loss of signal. Since hemosiderin is a paramagnetic compound, it is detectable on an SWI sequence, and thus this sequence is useful in the radiological evaluation of siderosis. A similar sequence is T2*GRE. In contrast to T2 relaxation, which normally acquires a spin echo signal, T2* acquires a gradient echo signal and thus requires a high uniformity of the magnetic field. This change in uniformity of the magnetic field can improve the rate of small lesion detection. Hemosiderin can result in small changes in the local magnetic fields and shortens the T2* relaxation times. Therefore, T2*GRE sequence is useful in the radiological diagnosis of siderosis.[1718192021]
Differential diagnosis of superficial siderosis includes neurocutaneous melanosis, which is a congenital syndrome that demonstrates multiple cutaneous melanocytic nevi that appear as T1 hyperintense and T2 hypointense signals at the pia-arachnoid surface. These lesions demonstrate postcontrast enhancement but are not susceptible on T2*GRE or SWI sequences. Brain surface vessels can also appear similar to superficial siderosis; however, the surface veins will enhance on T1 postcontrast sequences, whereas siderosis will demonstrate no enhancement. Meningioangiomatosis can also be considered as part of the differential diagnosis. This hamartomatous proliferation of meningeal cells can extend into the underlying cerebral cortex. The leptomeninges are thick, infiltrated with fibrous tissue, and are usually calcified. However, meningioangiomatosis demonstrates T1 postcontrast enhancement as compared to siderosis where there is no enhancement on postcontrast sequences. A bounce-point artifact can appear similar to siderosis. The artifact demonstrates a mismatch between repetition time and inversion recovery time on inversion recovery, T1, and FLAIR sequences. However, the artifact is not present on all sequences.[6789101116]
If left untreated, superficial siderosis can lead to progressive worsening of hearing loss and gait instability with as many as 25% of patients being bedridden within a few years. Treatment of superficial siderosis is primarily aimed at addressing the underlying cause of the bleed and preventing further progression of the disease.[67891011] There is no cure for superficial siderosis and treatment is still a matter of ongoing research. One drug which has shown promising results is deferiprone. Deferiprone is a lipid-soluble iron chelator that is Food and Drug Administration approved for thalassemia. In a case report published by Levy et al., one patient showed complete resolution of his ataxia and hearing loss after 3 years of treatment with deferiprone.[13]
CONCLUSION
Superficial siderosis should be included as part of the initial diagnostic workup for intracerebral/intraventricular tumors. T2*GRE or SWI sequence demonstrates high sensitivity and specificity in detecting the siderosis and thus should be included in the initial image acquisition process.
Financial support and sponsorship
This study was financially supported by the Department of Radiology at SUNY Upstate Medical University.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Jeevak Almast, M.B.B.S. for providing support.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/36/239709
REFERENCES
- Report of a case of melanosis of the brain, cord, and meninges. J Nerv Ment Dis. 1908;35:594.
- [Google Scholar]
- The importance of suspecting superficial siderosis of the central nervous system in clinical practice. J Neurol Neurosurg Psychiatry. 2004;75:188-90.
- [Google Scholar]
- Superficial siderosis of the central nervous system. Brain. 1995;118(Pt 4):1051-66.
- [Google Scholar]
- A population-based study of the incidence and survival rates in patients with pilocytic astrocytoma. J Neurosurg. 2003;98:1170-4.
- [Google Scholar]
- Posterior fossa surgery: An unusual cause of superficial siderosis. Neurosurgery. 1993;32:455-7.
- [Google Scholar]
- Diffuse superficial siderosis of the central nervous system: Four case reports and review of the literature. Rev Neurol. 2014;59:354-8.
- [Google Scholar]
- Cortical superficial siderosis and intracerebral hemorrhage risk in cerebral amyloid angiopathy. Neurology. 2013;81:1666-73.
- [Google Scholar]
- The pathology of superficial siderosis of the central nervous system. Acta Neuropathol. 2008;116:371-82.
- [Google Scholar]
- Superficial siderosis of the central nervous system secondary to spinal ependymoma. J Clin Neurosci. 2014;21:2017-9.
- [Google Scholar]
- Three cases of superficial siderosis of the central nervous system and review of the literature. Acta Neurochir (Wien). 2011;153:2067-73.
- [Google Scholar]
- Superficial siderosis of the central nervous system: MR findings with susceptibility-weighted imaging. Clin Imaging. 2011;35:217-21.
- [Google Scholar]
- Superficial siderosis of the central nervous system. A report on nine cases with autopsy. Acta Neuropathol. 1969;13:56-74.
- [Google Scholar]
- Superficial siderosis: A case report and review of the literature. Nat Clin Pract Neurol. 2007;3:54-8.
- [Google Scholar]
- Superficial siderosis of the central nervous system caused by hemorrhagic intraventricular craniopharyngioma: Case report and literature review. Neurol Med Chir (Tokyo). 2015;55:89-94.
- [Google Scholar]
- Superficial siderosis of the central nervous system. Its MRI manifestations. Clin Imaging. 1997;21:241-5.
- [Google Scholar]
- Neuroimaging in superficial siderosis: An in-depth look. AJNR Am J Neuroradiol. 2010;31:5-14.
- [Google Scholar]
- Cerebral microbleed detection and mapping: Principles, methodological aspects and rationale in vascular dementia. Exp Gerontol. 2012;47:843-52.
- [Google Scholar]
- GRE T2*-weighted MRI: Principles and clinical applications. Biomed Res Int 2014 2014 312142
- [Google Scholar]
- Identification of mineral deposits in the brain on radiological images: A systematic review. Eur Radiol. 2012;22:2371-81.
- [Google Scholar]
- Cognitive dysfunction in patients with cerebral microbleeds on T2*-weighted gradient-echo MRI. Brain. 2004;127:2265-75.
- [Google Scholar]






